Research Article - Journal of Clinical Dentistry and Oral Health (2022) Volume 6, Issue 4
Average number of patients underwent root canal treatment during COVID time
Pradeep S and Ravichandran V*
Department of Conservative dentistry and Endodontics, Saveetha University, Chennai, Tamil Nadu, India
- Corresponding Author:
- Ravichandran V
Department of Conservative dentistry and Endodontics
Saveetha University, Chennai, Tamil Nadu, India
E-mail: mahalakshmij.sdc@saveetha.com
Received: 27-Jun-2022, Manuscript No. AACDOH-22-67810; Editor assigned: 29-Jun-2022, PreQC No. AACDOH-22-67810(PQ); Reviewed: 14-Jul-2022, QC No.AACDOH-22-67810; Revised: 19-Jul-2022, Manuscript No. AACDOH-22-67810(R); Published: 26-Jul-2022, DOI:10.35841/aacdoh-6.4.120
Citation: Pradeep S, Ravichandran V. Average number of patients underwent root canal treatment during COVID time. J Clin Dent Oral Health. 2022;6(4):120
Abstract
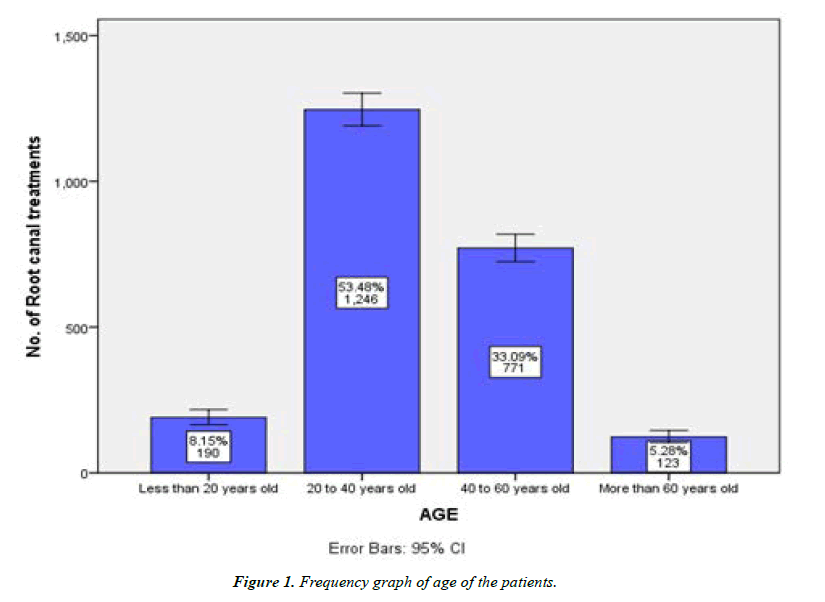
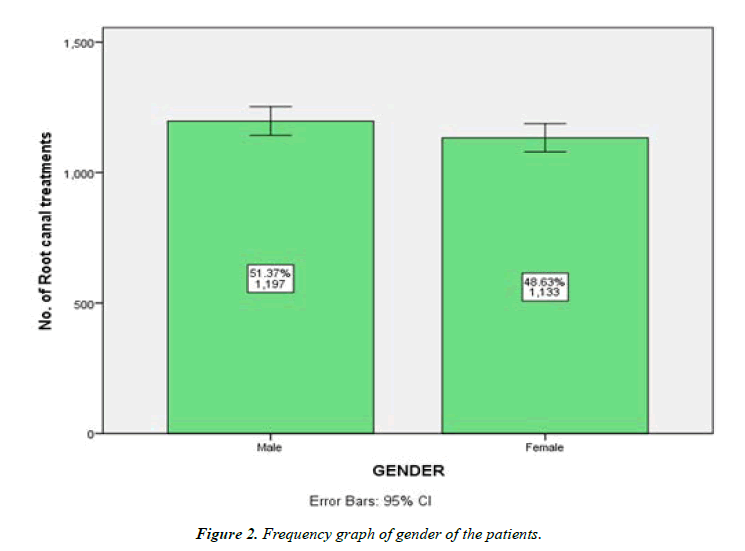
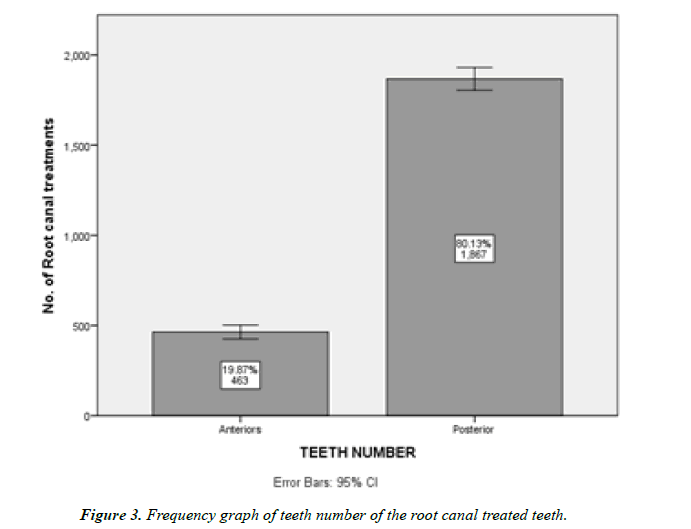
Introduction: The advent of the COVID-19 pandemic poses a significant global health risk. As dental care providers, we have major duties to both our dental team and our patients in terms of limiting virus exposure. The crew is at a significant risk of getting the virus and potentially transferring it due to the nature of our work. Enforcing adequate social distancing is one of the most important ways to contain this pandemic. We are faced with the dual problem of safeguarding ourselves and also our patients from community transmission while still ensuring that patients have access to urgent/emergency dental care. This study analyses the average number of patients underwent root canal treatment during the COVID time. Materials and Methods: The case sheet records (DIAS data) of patients who underwent Root canal treatment during COVID time were extracted. The data were analysed and transferred to MS Excel. Descriptive statistics and inferential test (Chi square test) were performed. Results: Among the total 2330 samples, Majority of the patients (53.5%) underwent Root canal treatment were 20 to 40 years old (1246. Patients). Majority of the root canal treatments (48.6%) were done in Posterior teeth (1867). The Gender ratio of the patients who underwent root canal treatment during COVID time was almost equal. Conclusion: In a COVID-19 high-risk location, endodontic emergencies account for a much larger proportion of dental emergencies than they would otherwise. During the COVID-19 outbreak, rubber dams, personal protective equipment, and patient screening all play a key role in keeping physicians safe.
Keywords
COVID, Dental emergencies, Novel method, Root canal treatment.
Introduction
Coronaviruses (CoVs) are zoonotic encapsulated single stranded RNA viruses that induce symptoms which range from the common cold to more severe respiratory, intestinal, hepatic, and neurological problems [1]. There are six known CoVs in humans, in addition to SARSCoV2: HCoV229E, HCoVOC43, SARS CoV, HCoVNL63, HCoVHKU1, and Middle East respiratory disease (MERS) CoV. In the previous two decades, CoVs have generated two large-scale pandemics: SARS and MERS [2]. Because of the nature of the dental environment, the dentist and the dental team, as well as the patient, are at a significant risk of cross infection. The COVID-19 pandemic has necessitated the implementation of strong and effective infection control policies in addition to those already in place in the dentistry context. In the current atmosphere, the goal of this position statement is to establish a Standard Operating Protocol (SOP) for endodontic and dental practise. This publication covers the basics of COVID-19 and nosocomial infection in dental settings, as well as recommended management strategies for both institutional and private dentistry offices.
The three most common transmission routes [3] of novel CoV include:
✔ Direct transmission (through cough, sneeze, or droplet inhalation)
✔ Contact transmission (through oro‐nasal‐ocular route) and
✔ Aerosol transmission.
Asymptomatic carriers of the infection can transmit the virus just as symptomatic individuals [4]. The SARSCoV2 virus can be identified in aerosols up to 3 hours after surgery and can survive for long periods of time on surfaces. The virus's persistence is affected by the type of the surface. The virus can survive for up to 4 hours on copper surfaces, 24 hours on cardboard, and 2–3 days on plastic and stainless steel [5].
Many countries have encouraged/expected social distance as a primary method for slowing the transmission of infection and “flattening the curve” of affected people over time. The CDC in the United States is regularly updating other methods taken to decrease the doubling time and rate of infection, in addition to social distance. This reduces the risk of others contracting the disease from an infectious individual. For example, a recent analysis based on available data predicted that in the absence of social distancing, 260,000 people in the United Kingdom would die. In fact, for people above the age of 70, this paradigm prescribes not only social isolation but also self-isolation.
Social isolation, on the other hand, makes it difficult to provide dental care. Endodontists, in particular, are dental practitioners who play a key role in the treatment of dental emergencies such as symptomatic pulpitis, acute dental infections, and dental traumatic injuries. As a result, total shutdown of clinical practices/dental institutes is not advised. Dentists can also help with health education by disseminating information on preventive measures offered by their respective national governments and referring suspicious COVID19 patients to government-approved facilities. Our team has extensive knowledge and research experience that has translated into high quality publications [6-25].
This study analyses the average number of patients underwent root canal treatment during the COVID time.
Materials and Methods
The DIAS (Dental Information’s Archiving Software) data of patients who underwent root canal treatment during COVID time were collected by simple random sampling method. Cross verification of data was done. Incomplete and censored data were excluded. The analysis was done using SPSS version 19. Descriptive statistics were used to correlate between the age, Gender and anterior & posterior teeth. The data after importing to SPSS was performed with a Chi- square test. The type of analysis performed was correlation and association. The level of significance was set at 0.05.
Results
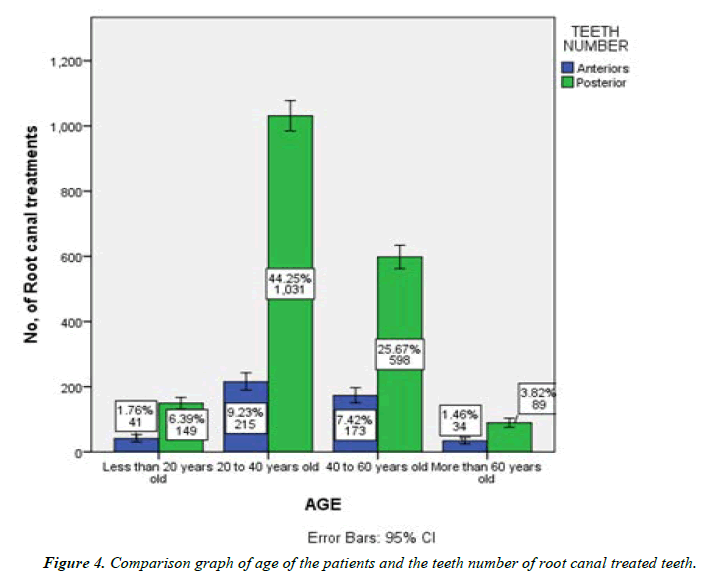
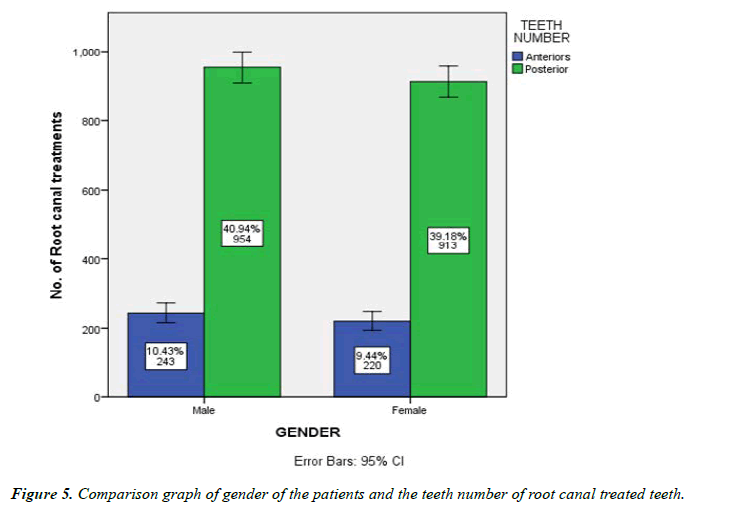
Among the total of 2330 patients, 8.2% were >20 years, 53.5% were 20 to 40 years old, 33.1% were 40 to 60 years old and 5.3% were <60 years old (Figure 1). Among the patients who underwent Root canal treatment, 51.4% were Male and 48.6% were Female (Figure 2). 20% of the root canal treatments were done in anterior teeth and 80% of the root canal treatments were done in Posterior teeth (Figure 3). Among the total samples, the majority of the root canals treatments were done to the patients of age between 20 to 40 years and Posterior teeth root canal treatment was the majority. The Gender ratio of the patients who underwent root canal treatment during COVID time was almost equal.
Discussion
Exceptional problems demand unprecedented solutions. Our major purpose as dental health care providers is to assist our patients in their time of need. However, the present pandemic has turned dentistry into a powerful disease-transmission vector in society. As a result, the current situation necessitates revised policy guidelines that clarify the scope of dental services that we can safely perform. This joint position statement from the IES, IFEA, and IDA is an attempt to provide a logical and effective clinical decision‐making process that enables us to effectively screen, protect, and serve our patients.
In this study, the male-to-female ratio for endodontic emergency patients (1.1:1) and total dental emergency patients (1.2:1) was practically the same (Figure 4), in contrast to other studies [26-30] that found a higher percentage of male patients presenting with dental emergencies. However, this disparity could be due to our patient population's larger proportion of endodontic emergency patients. In our study, the most common age group for endodontic crises was 20 to 40 years old (Figure 5). Importantly, COVID-19 prognosis is worsened with increasing age and the presence of underlying comorbidities [31-33]. Because patients older than 60 years represented approximately 5.3% of all patients, care should be exercised to avoid cross contamination. COVID-19 is now diagnosed using a mix of epidemiologic data, clinical symptoms; chest computed tomographic imaging findings, and laboratory investigations, such as RT-PCR on respiratory tract materials [31]. Sabino-Silva et al. [34] have highlighted serious concerns about the function of saliva in disease transmission between humans, particularly respiratory coronaviruses [35,36].
Endodontists should take appropriate measures to stay safe. The most prevalent endodontic emergency was symptomatic irreversible pulpitis. During the COVID-19 outbreak, treating endodontic emergencies was difficult because inhaling airborne particles and aerosols produced during dental operations on COVID-19 patients might possibly expose dentists to the virus [34], making them high-risk procedures. Reduced treatment time and exposure management are two approaches to lower the risk of infection during endodontic therapy. In cases of pulpitis, vital pulp therapy, such as pulpotomy or pulp capping, may be beneficial in terms of reducing treatment time. One day following therapy, pulpotomy has been shown to alleviate pain sensations in approximately 90% of dental emergency patients [37]. Partial pulpotomy with Mineral Trioxide Aggregate (MTA) had a good success rate (85%) over 3-year follow-ups in mature permanent teeth clinically diagnosed with irreversible pulpitis [38], and full pulpotomy with MTA had a 92.7% success rate in caries-exposed pulps in mature permanent molar teeth [39]. At 36 months, direct pulp capping with MTA had an 85 percent cumulative survival rate in adult molars with carious pulpal exposure [40]. Conebeam computed tomographic imaging and single-file systems were also considerably used for root canal treatment. A side from the benefits of detecting root canal placement and configuration [41], cone-beam computed tomographic examination could help patients avoid nausea or vomiting that can occur during intraoral x-ray examinations, as well as avoid exposure to the oral cavity [31]. Singlefile nickel-titanium systems could be employed during root canal preparation to save time and avoid the risk of sterilization [42]. Ather et al. [43] advised a number of preventative precautions for any therapy that produces droplets and/or aerosols, including the use of rubber dams. When rubber dams are used, it has been reported that up to 70% of airborne particles can be eliminated. Other than that, Regular UV sterilization of the dental instruments and the working area, Overnight disinfection of the working area and dental chair will and other clinical sterilization protocols are also recommended for the self-protection of Dentist as well as to reduce the contamination and spread.
Conclusion
In a COVID-19 high-risk location, endodontic emergencies account for a substantially larger percentage of dental emergencies than they would otherwise. During endodontic treatment, reducing treatment time and controlling exposure are two approaches to dramatically lower the risk of severe acute respiratory syndrome coronavirus transmission. Rubber dams, personal protective equipment, and patient screening all play a key role in keeping physicians safe. The advantage of vital pulp therapy is that it reduces treatment time. During the COVID-19 outbreak, rubber dams, personal protective equipment, and patient screening are critical in keeping physicians safe.
Acknowledgement
The authors would like to acknowledge the support rendered by the Department of Consevative Dentistry and Endodontic and Information technology of Sabetha dental college and hospitals and the management.
Funding
The present project is supported/funded/sponsored by Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University and the Kumaran TV center and Furnitures, Attur, Salem.
Conflict of Interest
The author has no conflict of interest.
References
- Wang Y, Zhou Y, Yang Z, et al. Clinical characteristics of patients with severe pneumonia caused by the 2019 novel coronavirus in Wuhan, China. Respiration. 2020; 1–9.
- Adhikari SP, Meng S, Wu Y-J, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty 2020; 9: 29.
- Lu C-W, Liu X-F, Jia Z-F. 2019-nCoV transmission through the ocular surface must not be ignored. The Lancet 2020; 395: e39.
- Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill; 25. Epub ahead of print February 2020.
- Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 2020; 382: 1564–1567.
- Muthukrishnan L. Imminent antimicrobial bioink deploying cellulose, alginate, EPS and synthetic polymers for 3D bioprinting of tissue constructs. Carbohydr Polym 2021; 260: 117774.
- Pradeep Kumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of Vertical Root Fractures by Cone-beam Computed Tomography in Root-filled Teeth with Confirmation by Direct Visualization: A Systematic Review and Meta-Analysis. J Endod 2021; 47: 1198–1214.
- Chakraborty T, Jamal RF, Battineni G, et al. A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management. Int J Environ Res Public Health; 18.10:5131
- Muthukrishnan L. Nanotechnology for cleaner leather production: a review. Environ Chem Lett 2021; 19: 2527–2549.
- Teja KV, Ramesh S. Is a filled lateral canal - A sign of superiority? J Dent Sci 2020; 15: 562–563.
- Narendran K, Jayalakshmi, Ms N, et al. Synthesis, characterization, free radical scavenging and cytotoxic activities of phenylvilangin, a substituted dimer of embelin. ijps; 82. Epub ahead of print 2020.
- Reddy P, Krithikadatta J, Srinivasan V, et al. Dental Caries Profile and Associated Risk Factors Among Adolescent School Children in an Urban South-Indian City. Oral Health Prev Dent 2020; 18: 379–386.
- Sawant K, Pawar AM, Banga KS, et al. Dentinal Microcracks after Root Canal Instrumentation Using Instruments Manufactured with Different NiTi Alloys and the SAF System: A Systematic Review. NATO Adv Sci Inst Ser E Appl Sci 2021; 11: 4984.
- Bhavikatti SK, Karobari MI, Zainuddin SLA, et al. Investigating the Antioxidant and Cytocompatibility of Mimusops elengi Linn Extract over Human Gingival Fibroblast Cells. Int J Environ Res Public Health; 18. Epub ahead of print 4 July 2021.
- Karobari MI, Basheer SN, Sayed FR, et al. An In Vitro Stereomicroscopic Evaluation of Bioactivity between Neo MTA Plus, Pro Root MTA, BIODENTINE & Glass Ionomer Cement Using Dye Penetration Method. Materials ; 14. Epub ahead of print 8 June 2021. DOI: 10.3390/ma14123159.
- Rohit Singh T, Ezhilarasan D. Ethanolic Extract of Lagerstroemia Speciosa (L.) Pers., Induces Apoptosis and Cell Cycle Arrest in HepG2 Cells. Nutr Cancer 2020; 72: 146–156.
- Ezhilarasan D. MicroRNA interplay between hepatic stellate cell quiescence and activation. Eur J Pharmacol 2020; 885: 173507.
- Romera A, Peredpaya S, Shparyk Y, et al. Bevacizumab biosimilar BEVZ92 versus reference bevacizumab in combination with FOLFOX or FOLFIRI as first-line treatment for metastatic colorectal cancer: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 2018; 3: 845–855.
- Raj R K, D E, S R. β-Sitosterol-assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Mater Res A 2020; 108: 1899–1908.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol 2019; 90: 1441–1448.
- Priyadharsini JV, Vijayashree Priyadharsini J, Smiline Girija AS, et al. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Archives of Oral Biology 2018; 94: 93–98.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res 2020; 34: e002.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the Maximum Occlusal Bite Force and its Relation to the Caries Spectrum of First Permanent Molars in Early Permanent Dentition. J Clin Pediatr Dent 2020; 44: 423–428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: a review and orthodontic implications. Br Dent J 2021; 230: 345–350.
- Kanniah P, Radhamani J, Chelliah P, et al. Green synthesis of multifaceted silver nanoparticles using the flower extract of Aerva lanata and evaluation of its biological and environmental applications. ChemistrySelect 2020; 5: 2322–2331.
- Huang J-Y, Yu H-C, Chen Y-T, et al. Analysis of emergency dental revisits in Taiwan (1999–2012) from Taiwanese National Health Insurance Research Database (NHIRD). Journal of Dental Sciences 2019; 14: 395–400.
- Currie CC, Stone SJ, Connolly J, et al. Dental pain in the medical emergency department: a cross-sectional study. J Oral Rehabil 2017; 44: 105–111.
- Quiñonez C. Self-reported emergency room visits for dental problems. Int J Dent Hyg 2011; 9: 17–20.
- Quiñonez C, Gibson D, Jokovic A, et al. Emergency department visits for dental care of nontraumatic origin. Community Dent Oral Epidemiol 2009; 37: 366–371.
- Verma S, Chambers I. Dental emergencies presenting to a general hospital emergency department in Hobart, Australia. Aust Dent J 2014; 59: 329–333.
- Meng L, Hua F, Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. Journal of Dental Research 2020; 99: 481–487.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–513.
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020; 323: 1061–1069.
- Sabino-Silva R, Jardim ACG, Siqueira WL. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Investig 2020; 24: 1619–1621.
- Lu B, Huang Y, Huang L, et al. Effect of mucosal and systemic immunization with virus-like particles of severe acute respiratory syndrome coronavirus in mice. Immunology 2010; 130: 254–261.
- Liu L, Wei Q, Alvarez X, et al. Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J Virol 2011; 85: 4025–4030.
- Hasselgren G, Reit C. Emergency pulpotomy: pain relieving effect with and without the use of sedative dressings. J Endod 1989; 15: 254–256.
- Taha NA, Khazali MA. Partial Pulpotomy in Mature Permanent Teeth with Clinical Signs Indicative of Irreversible Pulpitis: A Randomized Clinical Trial. J Endod 2017; 43: 1417–1421.
- Taha NA, Ahmad MB, Ghanim A. Assessment of Mineral Trioxide Aggregate pulpotomy in mature permanent teeth with carious exposures. Int Endod J 2017; 50: 117–125.
- Kundzina R, Stangvaltaite L, Eriksen HM, et al. Capping carious exposures in adults: a randomized controlled trial investigating mineral trioxide aggregate versus calcium hydroxide. Int Endod J 2017; 50: 924–932.
- Fan B, Ye W, Xie E, et al. Three-dimensional morphological analysis of C-shaped canals in mandibular first premolars in a Chinese population. Int Endod J 2012; 45: 1035–1041.
- Kuzekanani M. Nickel-Titanium Rotary Instruments: Development of the Single-File Systems. J Int Soc Prev Community Dent 2018; 8: 386–390.
- Ather A, Patel B, Ruparel NB, et al. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J Endod 2020; 46: 584–595.
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref
Index at, Google Scholar, Cross Ref