Case Report - Ophthalmology Case Reports (2023) Volume 7, Issue 4
An aggressive case of von hippel-lindau disease: Case report and review of outcomes.
Bruno B Ribeiro1*, Catarina S Castro1, Miguel R Lume1, Maria J Furtado1,21Department of Ophthalmology, University Hospital Center of Santo Antonio, Oporto, Portugal
2ICBAS – School of Medicine and Biomedical Sciences, University of Porto, Oporto, Portugal
- *Corresponding Author:
- Bruno B Ribeiro
Department of Ophthalmology
University Hospital Center of Santo Antonio
Oporto, Portugal
E-mail: brunot.barbosaribeiro@gmail.com
Received: 24-Jun-2023, Manuscript No. OER-23-103811; Editor assigned: 26-Jun-2023, Pre QC No. OER-23-103811(PQ); Reviewed: 10-Jul-2023, QC No. OER-23-103811; Revised: 26-Jul-2023, Manuscript No. OER-23-103811(R); Published: 02-Aug-2023, DOI: 10.35841/2591-7846-7.4.162
Citation: Ribeiro BB, Castro CS, Lume MR, et al. An aggressive case of von hippel-lindau disease: Case report and review of outcomes. Am J Ophthalmol 2023;7(4):162.
Abstract
Purpose: To report a case of exudative retinal detachment secondary to Retinal Capillary Hemangioblastomas (RCH) in a patient with severe Von-Hippel Lindau (VHL) disease. Methods: We conducted a retrospective review of the patient’s clinical records. Informed consent was obtained. Results: We present the case of a 46-year-old female diagnosed with VHL syndrome in 1998. Past medical history is relevant for several neurosurgical interventions due to cerebellar hemangioblastomas. Past ophthalmic history is relevant for Left Eye (LE) evisceration due to RCH with secondary exudative retinal detachment and neovascular glaucoma. Over the course of 10 years, the patient developed multiple Right Eye (RE) RCH, successfully treated and controlled with laser photocoagulation and transscleral cryotherapy. In December 2021, new multiple cerebellar hemangioblastomas were detected on Magnetic Resonance Imaging (MRI) and a pancreatic neuroendocrine tumor was diagnosed. She also experienced rapid growth of new RCH complicated with secondary inferior exudative retinal detachment, treated with laser photocoagulation combined with intravitreal anti-VEGF, with good response and complete resolution of sub retinal fluid. Best corrected visual acuity has been stable throughout follow-up. Conclusion: VHL syndrome is a rare, multisystem disease with high morbidity and retinal capillary hemangioblastoma is the hallmark of ocular manifestations. Although laser photocoagulation and transscleral cryotherapy has been the mainstay of treatment, anti-VEGF therapy may be a valuable adjuvant for controlling exudative complications.
Keywords
Hemangioblastoma, Anti-VEGF, Retinal detachment, Von-Hippel Lindau, Retinal capillary hemangioblastomas.
Summary Statement
We report a case of severe manifestations of VHL disease, with multiple and progressive retinal capillary hemangioblastomas treated with laser photocoagulation. The patient ultimately developed an exudative retinal detachment, which was successfully treated with laser photocoagulation combined with intravitreal injection of anti-VEGF (ranibizumab followed by aflibercept).
Introduction
Von Hippel-Lindau (VHL) syndrome is a potentially aggressive, autosomal dominant, multiorgan neoplastic disease that arises due to a mutation in the VHL tumor suppressor gene [1-3]. It typically manifests in the third to fourth decades of life and common manifestations include retinal and cerebellar hemangioblastomas, as well as renal cell carcinoma. Retinal Capillary Hemangioblastoma (RCH) is the ophthalmic hallmark, being one of the earliest and most common manifestations [2,4]. Severe cases may be complicated by exudative retinal detachment, with high-risk of vision loss. Despite lack of high quality scientific evidence, management includes thermal laser photocoagulation, transscleral cryotherapy and vitreoretinal surgery and intravitreal vascular endothelial growth factor (VEGF) antagonists [1,5-7].
Case Report
We present the case of a 46-year-old Caucasian female diagnosed with VHL disease in 1998. Past medical history is relevant for several neurosurgical interventions due to cerebellar hemangioblastomas. Past ophthalmic history is relevant for Left Eye (LE) evisceration in 2006 due to RCH with secondary exudative retinal detachment and neovascular glaucoma. Over the course of 10 years, the patient developed several Right Eye (RE) RCH, which were treated and controlled with laser photocoagulation and transscleral cryotherapy (Figure 1).
In December 2021, the disease showed increased activity, with growth of multiple cerebellar hemangioblastomas and diagnosis of a pancreatic neuroendocrine tumor. She also experienced rapid growth of new RCH, which presented initially as cherry-red capillary telangiectasia on the retinal surface with subsequent growth of the feeding artery and draining veins.
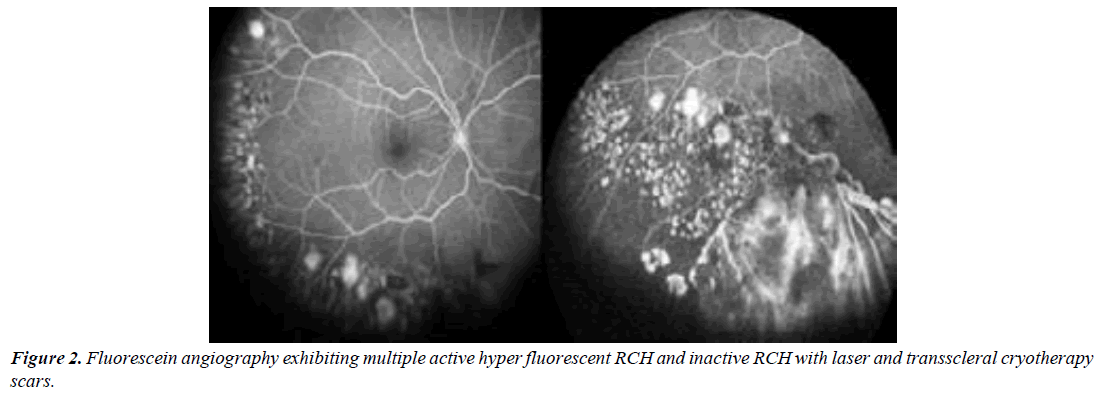
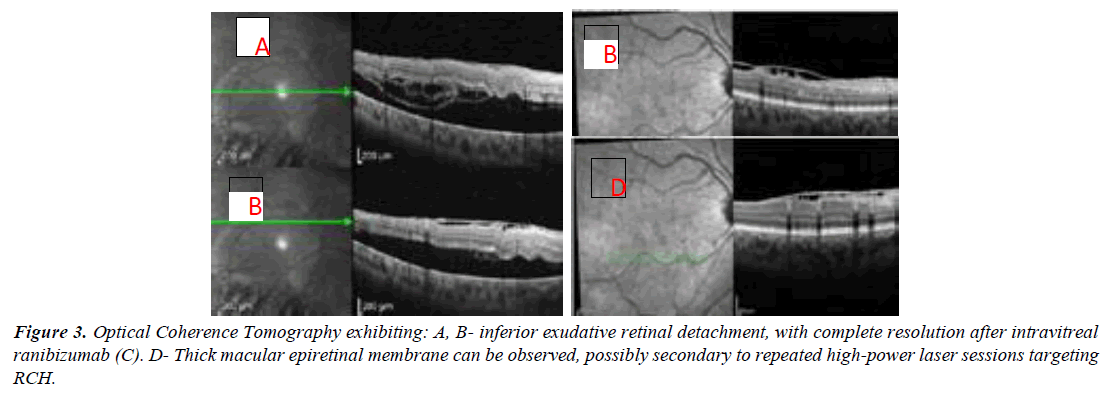
Spectral Domain Optical Coherence Tomography (SD-OCT) of the vascular tumour showed hyper-reflective thickening of the inner retina and early hyperfluorescence and late leakage were documented in fluorescein angiography at the tumour level (Figure 2). An inferior exudative retinal detachment extending to the inferior temporal vascular arcade was detected in the course of disease progression (Figure 3).
Intravitreal ranibizumab (0.5 mg/0.05 mL) – two injections with 8 week interval - combined with laser photocoagulation targeting the vascular tumours induced complete regression of subretinal fluid, with maintenance of the best-corrected visual acuity in 20/25, without recurrence of exudative retinal detachment in the upcoming follow-up visits.
After 1 year of follow-up, fundoscopy and ultra wide field fluorescein angiography revealed asymptomatic new vascular tumours and focal growth of previously inactive RCH. Considering the presence of macular epiretinal membrane possibly secondary to repeated high-power LASER sessions, adjuvant intravitreal aflibercept injections (PRN – pro re nata – regimen) were also performed, in order to achieve a more effective control of tumour growth and prevent recurrence of exudative detachment.
Discussion
We report the case of a monocular young female with aggressive cerebellar and retinal manifestations of VHL disease. Over the course of 25 years, this patient has experienced bouts of outbreak and remission in multiorgan involvement typical of this aggressive, chronic disease with high morbidity. Current consensus states that patients with VHL disease should perform annual ophthalmic evaluation, starting in early childhood [2,4,8]. A systematic multimodal approach, which may include ultra wide-field color fundus photography and fluorescein angiography, can improve sensitivity for detection of even small lesions, particularly in uncooperative, younger patients [8]. RCH can arise in the retina near the optic disk (juxtapapillary) or elsewhere (extrapapillary), as in the reported patient. The goal of treatment for extrapapillary RCH is usually to destroy the tumor and prevent further growth, albeit observation can be reasonable in small lesions without signs of progression. However, patients should be followed closely and a low threshold for treatment should be adopted [1,2,5,8]. There is a role for thermal laser photocoagulation, transscleral cryotherapy, radiotherapy, verteporfin photodynamic therapy and intravitreal injection of VEGF antagonists in the management of RCH. Laser photocoagulation is probably the most used treatment modality, especially for extrapapillary RCH inferior to 1.5 mm. Some authors recommend the use of blue-green wavelength LASER immediately after infusion of intravenous fluorescein, in order to enhance energy uptake by the targeted vascular lesions [1,7]. Larger lesions are more difficult to destroy using thermal laser photocoagulation and cryotherapy may be used as the first-line therapy, depending on the preference and experience of each center. It should also be noted that effective laser photocoagulation of larger RCHs frequently requires high power and pulse duration, which pose increased risk of secondary epiretinal membrane as evident in our patient’s SD-OCT. and other complications.
Large RCHs (usually more than 1.5 mm in diameter) are difficult to completely photocoagulate, making their management and surveillance more challenging. Currently, the most reliable indicator of quiescence is the absence of growth over long-term follow-up, documented through fundus observation and fluorescein angiography. There is evidence stating that RCH growth may respond to intravitreal VEGF antagonists, since inactivated VHL protein function may increase Hypoxia-Inducible Factor (HIF) related angiogenesis through production of VEGF and Platelet-Derived Growth Factor (PDGF). Hence, VEGF antagonists may promote RCH shrinkage as well as reduction of vascular tortuosity and subretinal fluid [2,3,6,9]. Most works regarding the use of intravitreal anti-VEGF drugs in RCH are small case series and non-randomized clinical trials. Ranibizumab is a fragment of a recombinant, humanized IgG1 monoclonal antibody that neutralizes all active forms of VEGF-A [6]. Wong reported a series of 5 patients with refractory exudative RCHs treated with intravitreal ranibizumab, showing improvement in only one patient, which exhibited a small, peripheral RCH [6]. Chelala reported reduced vascularization and mild shrinkage of a juxtapapillary RCH after only one intravitreal injection of ranibizumab [9]. Aflibercept is a fusion protein that simultaneously blocks VEGF-B and placental growth factor (PIGF), with potential improved control of vascular lesions [10]. Konstantinou showed resolution of exudation following intravitreal aflibercept in two patients with large, far peripheral, treatment naïve RCH [10].
Therefore, it appears that anti-VEGF therapy may be useful in some patients, especially as adjuvant therapy for refractory RCH, as in our patient, or in large RCH in the far periphery with active exudation. It should also be noted that anti-VEGF may be the most appropriate option in juxtapapillary RCHs due to its location and limited treatment options. It seems reasonable that smaller RCH produce less amount of VEGF, which may render it less responsive to VEGF antagonists. Besides, as the driving mechanism is not fully suppressed with these drugs, absent or temporary efficacy may be justified in some cases. Until now, anatomical and functional biomarkers to predict the course and response to therapy of RCH have not been established. Further studies are needed and can provide information in the future about the best approach to RCH based in anatomical and functional biomarkers.
Conclusion
In summary, VHL disease is a multiorgan, progressive, neoplastic entity that arises due to a mutation in the VHL tumor suppressor gene. Retinal capillary hemangioblastoma is the ophthalmic hallmark and is associated with high morbidity and risk of vision loss. Thermal laser photocoagulation and transscleral cryotherapy have been the most used treatment modalities, albeit it’s suboptimal efficacy. Novel therapies, such as intravitreal injections of VEGF antagonists may play a significant role in refractory cases as well as in cases with significant secondary exudation. The presence of subretinal fluid may represent a novel anatomical biomarker that can predict a good response to intravitreal anti-VEGF drugs. There are few reported cases comparing treatment modalities and more evidence is needed to improve our knowledge on this disease.
Conflicts of Interest
The authors have no conflict of interest to declare. This work received no funding of any institution or organization.
References
- Chelala E, Dirani A, Fadlallah A. Intravitreal anti-VEGF injection for the treatment of progressive juxtapapillary retinal capillary hemangioma: a case report and mini review of the literature. Clin Ophthalmol. 2013;7:2143-2146.
- Chen X, Sanfilippo CJ, Nagiel A, et al. Early detection of retinal hemangioblastomas in Von Hippel-Lindau disease using ultra-widefield fluorescein angiography. Retina. 2018;38(4):748-754.
- Dollfus H, Massin P, Taupin P, et al. Retinal hemangioblastoma in von Hippel-Lindau disease: a clinical and molecular study. Invest Ophthalmol Vis Sci. 2002;43(9):3067-74.
- Konstantinou EK, Kodati S, Wiley HE, et al. Assessment of Retinal Changes Following Intravitreal Aflibercept in 2 Patients With Von Hippel-Lindau Disease-Related Retinal Capillary Hemangioblastoma. JAMA Ophthalmol. 2022;140(12):1243-4.
- Krivosic V, Kamami-Levy C, Jacob J, et al. Laser Photocoagulation for Peripheral Retinal Capillary Hemangioblastoma in von Hippel-Lindau Disease. Ophthalmol Retina. 2017;1(1):59-67.
- Latif F, Tory K, Gnarra J, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Sci.1993;260(5112):1317-20.
- Lonser RR, Glenn GM, Walther M, et al. von Hippel-Lindau disease. Lancet. 2003;361(9374):2059-67.
- Singh AD, Nouri M, Shields CL, et al. Treatment of retinal capillary hemangioma. Ophthalmol. 2002;109(10):1799-806.
- Wiley HE, Krivosic V, Gaudric A, et al. Management of retinal hemangioblastoma in von Hippel-Lindau disease. Retina (Philadelphia, Pa.). 2019;39(12):2254.
- Wong WT, Liang KJ, Hammel K, et al. Intravitreal ranibizumab therapy for retinal capillary hemangioblastoma related to von Hippel-Lindau disease. Ophthalmol. 2008;115(11):1957-1964.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref