Brief Report - Journal of Anesthetics and Anesthesiology (2022) Volume 4, Issue 2
A clinical audit on standards for grading for risk assessment & prophylactic management of postoperative nausea and vomiting.
Yilkal Tadesse Desta*
Department of Anaesthesia, Bahirdar University, Ethiopia
- Corresponding Author:
- Yilkal Tadesse Desta
Department of Anaesthesia
Bahirdar University, Ethiopia
Tel: +251918727806
E-mail: yilkaltadesse@yahoo.com
Received: 19-Feb-2022, Manuscript No. AAAA-22-54938; Editor assigned: 21-Feb-2022, PreQC No. AAAA-22-54938(PQ); Reviewed: 07-Mar-2022, QC No. AAAA-22-54938; Revised: 23-Apr-2022, Manuscript No. AAAA-22-54938(R); Published: 30-Apr-2022, DOI:10.35841/aaaa-4.2.110
Citation: Desta YT. A clinical audit on standards for grading for risk assessment & prophylactic management of postoperative nausea and vomiting. J Anesthetic Anesthesiol. 2022;4(2):110
Keywords
Post-operative nausea and vomiting, Anesthesia, Surgery.
Introduction
The most common and distressing symptoms, which follow anaesthesia and surgery are pain and emesis. The consequences of Postoperative Nausea and Vomiting (PONV) are physical, surgical and anaesthetic complications. It is not just only for patients but also do have financial implications for the hospitals or institutions providing the service [1]. Anesthetic techniques has become considerably safe and changed over time, hence currently anti-emetic is considered as an important part of ‘triads of anesthesia’. Even though the prevalence of PONV was found to be 36.6%, as reported on a study done in this area, prevention and optimal management of PONV remain neglected in the routine anaesthetic part of anesthetic management [2].
There are several international accepted standards recommended for prevention and management of PONV. Consensus guidelines, produced in 2019 suggest treating only higher risk patients with prophylactic anti-emetics which can be estimated based on assessment of four risk factors the guideline does not apply to pregnant women [3]. Treating according to risk will result in better treatment and cost reduction, therefore; this audit is important to identify areas of good practice and gaps where improvements need to be done based on the standards.
Aim
To assess the extent of adaption and application of international consensus guidelines regarding risk assessment and prophylactic management of PONV; whereby to identify the gap and used to improve safe and quality practice of anaesthetic services [4,5].
Objectives
• To identify the number of responsible clinical practitioners who aware of the optimal approach for prevention and therapy of PONV in various patient populations.
• To determine the amount of responsible practitioners who know and use any method to assess risk factors for PONV.
• To describe the ratio of responsible practitioners who used to manage PONV with prophylaxis anti-emetics for high risk patients.
• To find out relative amount of responsible practitioners who adopt with best regimen choice and timing of antiemetic administration.
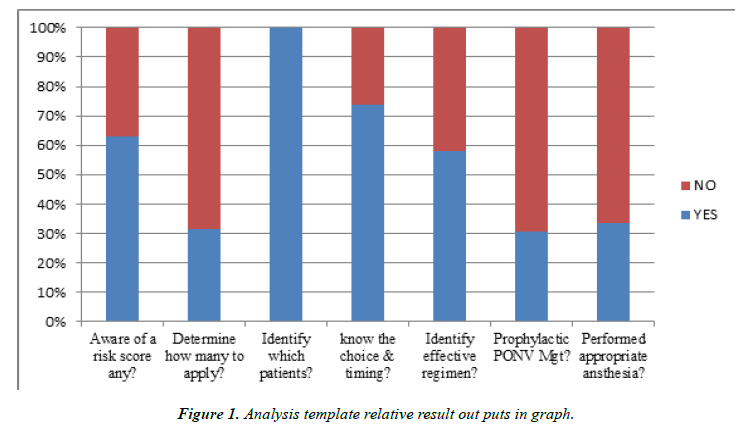
• To determine the ratio of anesthetists who had just used the optimal approach and anesthetic intervention options to reduce the baseline risks for PONV Figure 1.
• To improve comprehensive post-anaesthesia care outcomes for patients who just had anaesthesia, sedation or analgesia care Table 1.
| Criteria | Exceptions | Standards | Source of evidences | Where data will be found |
|---|---|---|---|---|
| International consensus outlined the following guidelines of conduct which define the essentials of honorable adoption for the practitioner:- | ||||
| A clinical practitioner shall recognize that for all surgical patients, a PONV risk score should be calculated. | pregnant women | 100 % | NHSUK consensus clinical guideline | Asking for responsible clinical practitioners |
| A clinical practitioner shall determine how many of the risk factors apply to each patient. | II | 100 % | II | II |
| A clinical practitioner shall identify which patients should receive anti-emetics prophylactically during surgery | II | 100 % | II | II |
| A clinical practitioner shall determine the optimal choice and timing of antiemetic administration. | NONE | 100 % | IARS consensus clinical guideline | II |
| A Clinical practitioner shall use prophylaxis anti-emetics to manage PONV for high risk patients when indicated. | NONE | 100 % | NHSUK consensus clinical guideline | Reterospective chart review |
| Anaesthesia practitioner shall perform the optimal approach and anesthetic interventions to reduce the baseline risks for PONV in high risk patients. | NONE | 100 % | IARS consensus clinical guideline | II |
| A clinical practitioner shall identify the most effective antiemetic monotherapy and combination therapy regimens. | NONE | 100 % | II | Asking for responsible clinical practitioners |
Table 1. Standards.
Audit Methodology
Audit population
Volunteer anesthetists, residents and interns, who found in the peri- operative area within period of data collection Table 2.
| A Clinical Audit on Risk Assessment and Prophylactic Management of PONV | Source of forms- IARS & NHSUK Guidelines |
Audit No- -- |
||
|---|---|---|---|---|
| St.No | Standards | Yes | No | NA |
| 1 | Is he/she aware of any PONV risk assessment tool or method → Assessing number of risk factors (Afpels Risk Stratification) or based on anticipated duration of anesthesia or depending on type of surgery.) | |||
| 2 | Could he/she determine how many of the risk factors apply to each patient →≥ 2 (Female gender, Non-smoker, Hx of PONV/motion sickness, Long-acting opioid premedication or duration of anesthesia > 30 min) or regardless of risk factors one of factors in some specialities (hiatal surgery, Ophthalmic/Middle ear procedures, Neurosurgery) | |||
| 3 | Could he /she identify which patients need to receive anti-emetics prophylactically during surgery → ≥ 2risk factors or ≥ Medium(40%) (Low risk (10-20%), Medium(40%),High(60%) and Very high(80%). | |||
| 4 | Does he /she know the optimal choice and timing of antiemetic administration→ Antihistamines alone or Antihistamines with dexamethasone when best combined& 10’ before induction. | |||
| 5 | Does he /she recognize and identify the most effective antiemetic monotherapy and combination therapy regimens→ monotherapy (promethiazine25 mg/cyclizine50 mg IV) for medium and combination therapy (cyclizine50 mg & dexamethasone 4mg IV ) for high & very high risk factors. | |||
| 6 | Has he /she provided or ordered prophylaxis anti-emetics peri-operatively for a patient with medium or high/ very high risk of PONV→ asking and chart review post operatively. | |||
| 7 | Did he /she perform the appropriate approach and anesthetic induction preference to reduce the baseline risks for PONV in high risk patients → asking and chart review post operatively. | |||
Table 2. A clinical audit data collection tool regarding Risk Assessment and Prophylactic Management of PONV Standards To mark/ √ /on a specified box for the questions from the standard and filled subjectively/ direct interviews or chart reviews.
Audit sample
An institutionally-based, quantitative and descriptive audit performance assessment conducted in the main operation theatre Table 3.
| Audit Ref No | Source of form | Aware of a risk score any? Y/N/NA | Determine how many to apply? Y/N NA | Identify which patients? Y/N/NA | know the choice & timing ? Y/N/NA | Identify effective regimen? Y/N/NA | Prophy PONV Mgt? Y/N/NA | Performed appropriate ansthesia? Y/N/NA |
|---|---|---|---|---|---|---|---|---|
| 1 | R1 | Yes | No | Yes | Yes | No | N/A | N/A |
| 2 | Anst | No | No | Yes | Yes | Yes | No | No |
| 3 | Anst | Yes | No | Yes | Yes | No | Yes | No |
| 4 | R1 | Yes | Yes | Yes | Yes | No | N/A | N/A |
| 5 | R2 | Yes | No | Yes | Yes | Yes | Yes | N/A |
| 6 | Intrn | Yes | Yes | Yes | No | Yes | No | N/A |
| 7 | Intrn | No | No | Yes | Yes | No | No | N/A |
| 8 | R2 | Yes | No | Yes | No | Yes | N/A | N/A |
| 9 | R1 | No | No | Yes | No | No | N/A | N/A |
| 10 | Anst | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 11 | Anst | Yes | No | Yes | Yes | Yes | No | No |
| 12 | Intrn | No | No | Yes | Yes | No | No | N/A |
| 13 | Anst | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 14 | Intrn | Yes | Yes | Yes | Yes | Yes | No | N/A |
| 15 | R2 | Yes | No | Yes | Yes | No | No | N/A |
| 16 | Intrn | No | No | Yes | No | Yes | N/A | N/A |
| 17 | Intrn | No | No | Yes | Yes | No | N/A | N/A |
| 18 | Anst | Yes | No | Yes | No | Yes | No | Yes |
| 19 | R2 | Yes | Yes | Yes | Yes | Yes | No | N/A |
Table 3. A clinical Audit data set for Risk Assessment and Prophylactic Management of PONV standards sample forms.
Data collection method
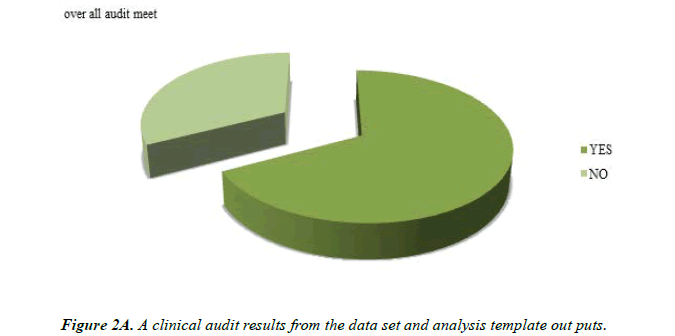
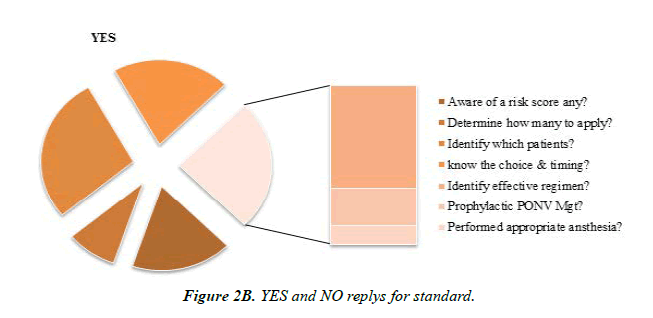
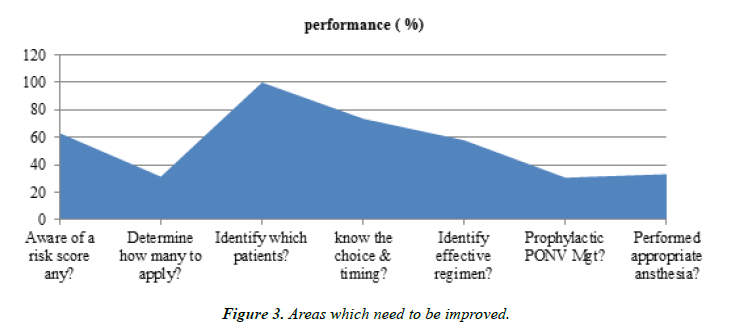
Prospective data collection done through subjective sampling and retrospective chart review based on the structured qualitative data collection tool with yes or no interpretation for descriptive analysis (Figure 2A and Figure 2B). Re-audit should also be considered for bringing good progress of implementation and for better patient satisfaction by which; safe Figure 3. Quality and comprehensive anaesthetic services will be improved in the hospital.
Areas of good practice
For all observations of the data set regarding to practitioners need to identify which patients should receive prophylactic anti-emetics during surgery; it has shown significant positive replies, even though it’s not being applied as seen with other standards [5]. Good audit performance results have seen also on guidelines that a clinician shall recognize that for all surgical patients. A PONV risk score should be calculated and one should know determine the optimal choice and timing of antiemetic administration Table 4.
| St NO | No of sample forms/tools from to whom the standard applies. | No of sample forms/tools which meet the audit standard. | No of sample forms/tools which meet the exception criteria. | No and % of sample forms/tools which meet the standard. | |
|---|---|---|---|---|---|
| Standards | |||||
| 1 | Aware of a risk score any? | 19 | 12 | 0 | 12/19 X 100=63.1 % |
| 2 | Determine how many to apply? | 19 | 6 | 0 | 6/19 X 100= 31.5 % |
| 3 | Identify which patients? | 19 | 19 | 0 | 19/19 X 100=100 % |
| 4 | Know the choice & timing? | 19 | 14 | 0 | 14/19 X 100=73.6 % |
| 5 | Identify effective regimen? | 19 | 11 | 0 | 11/19 X 100=57.9 % |
| 6 | Prophylactic PONV Mgt? | 13 | 4 | 6 | 4/13 X 100 = 30.7 % |
| 7 | Performed appropriate ansthesia? | 6 | 2 | 13 | 2/6 X 100=33.3 % |
Table 4. Analysis Template for the audit data set performance.
Conclusion
Again satisfactory percent of positive reply meets to the guideline in regard to identifying the most effective antiemetic monotherapy and combination therapy regimens to be best given. There are significantly high gap and markedly less audit performance mainly for three standards set. Which are regarding; one on adoption with how many of the risk factors considered for identifying high risk groups, and the other on the option and practice of optimal anaesthetic approaches in concern with baseline main risk factors. Moreover, considerable gap for a guideline in regard with the routine use prophylaxis anti-emetics to prevent and best manage PONV for high risk patients when indicated.
References
- Apfel CC, Laara E, Koivuranta M, et al. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. The Journal of the American Society of Anesthesiologists. 1999;91(3):693-700.
- Kazemi KF, Henzi I, Tramèr MR. Treatment of established postoperative nausea and vomiting: a quantitative systematic review. BMC anesthesiol. 2001;1(1):1-1.
- Gan TJ, Meyer T, Apfel CC, et al. Consensus guidelines for managing postoperative nausea and vomiting.Anesth Analg. 2003;97(1):62-71.
- Carlisle J, Stevenson CA. Drugs for preventing postoperative nausea and vomiting.Cochrane database of systematic reviews. 2006(3).
- Tramèr MR. Systematic reviews in PONV therapy.In Evidence Based Resource in Anaesthesia and Analgesia 2000; (157-178). BMJ Books, London.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref