Case Report - Journal of Clinical Dentistry and Oral Health (2018) Oral Medicine and Surgery- Vol II
Regenerative treatment of periodontitis using diode laser: Case study
Balsam Mirdan1*, Asseel Rashid2
1Ministry of Higher Education, College of Dentistry, University of Kirkuk, Iraq
2Al Eweah Specialized Centre for Dentistry, Ministry of Health, Iraq
- *Corresponding Author:
- Balsam M. Mirdan
College of Dentistry
University of Kirkuk
Iraq
E-mail: balsammmardam@gmail.com
Accepted on August 28, 2018
Citation: Mirdan B, Rashid A. Regenerative treatment of periodontitis using diode laser: Case study. J Oral Med Toxicol 2018;2(1):4-8.
Abstract
Introduction: Regenerative treatment aimed to restore tooth supporting structure and its functional attachment through regeneration of cementum, periodontal ligaments and surrounding alveolar bone. Diode laser 940 nm wavelength has the potential to act as antibacterial and enhances wound healing. Material and methods: Case one; 30 years old male having infra bony pocket about (10-13 mm depth) at 16, 17, 26, 27, 36, 37, 46 and 37. The treatment was done by using 940 nm wavelength diode lasers; the output power was 800 mw, 50% Duty cycle in pulsed mode. Energy was delivered through optical fibre 300 um in diameter for 20s exposure time at each site of the pocket. The treatment period was three months’ time with weekly recall. Case two; 39 year old male with tilted 36, 37 (a pocket depth of 13 mm at tooth number 36-37) was treated by the same previously method and dose parameter for one month weekly recall.
Results: Restoring the periodontal support of teeth was clear with the stimulation of bone formation surrounding each affected tooth clinically through the absence of the pain and bleeding on probing symptoms. Moreover there was decreasing of the pocket depth which was measured by pocket measuring probe, intraoral X-ray and Orthopantamogram was used pre and post treatment.
Conclusion: 940 nm wavelength diode lasers is an efficient tool to treat periodontal pocket and stimulates bone growth, and cementum formation when right parameters were applied.
Keywords
Periodontitis, 940 nm diode laser, Bone regeneration.
Introduction
Periodontitis is a progressive inflammation of the tooth supporting structures (gingiva, periodontal ligament and the surrounding bone).
It is usually irreversible inflammation but maybe arrested by treatment [1]. The major clinical signs are:
The presence of microbial plaque.
Periodontal inflammation manifested by redness and bleeding on probing.
Loss of attachment of alveolar bone [2].
The later causes bone destruction that forms the infrabony pocket which might be due to the squally of the inflammatory changes in the gingiva or due to trauma from occlusion or both [3].
The structural component of cranial bone whether cortical or compact consists of organic matrix and inorganic matrix. The major content of the inorganic matrix are calcium hydroxyapatite and osteocalcium phosphate. Calcium hydroxyapatite is responsible for the compressive strength of the bone. While the collagen, protein, blood cells and lipids are the component of the organic matrix.
58% of the bone is hydroxyapatite, 25% is collagen, 12% water and 5% is for carbohydrate contained [4].
The absorption coefficient of bone at 900-956 nm wavelength range is 0.15-0.21 cm-1 (± 0.02) respectively, while the reduced scattering coefficient at the same previously mentioned range of wavelength is 17.03-17.51 cm-1 (± 1.11) [5].
Several studies proved that Low Level Laser Therapy (LLLT) is sufficient tool to disinfect wound and stimulate healing [6].
It was concluded by Oliveira et al. that both red and infra-red laser phototherapy promote an enhancement of osteoblast Alkaline Phosphatase (ALP) and Matrix Metalloproteinase Protein (MMP’s) [7].
Stimulation or inhibition in cellular activities of any tissue through laser bio stimulation ruled by many factors. On the laser side; the incident wavelength, its power density, exposure time and mode of operation. While the targeted tissue; absorption coefficient and its refractive index at that incident wavelength in addition to the tissue temperature at time of treatment plus tissue contained, all have to be studied well before any operation. These case studies are trials to get the efficient laser parameter that enhances periodontal tissue regeneration without any surgical intervention to treat the infrabony pocket in human.
Material and Methods
Case one
Male patient 30 year old, non-smoking, presented in the private clinic, his chief complaint was pain on chewing and bleeding on molar region area for the maxilla and mandible. No relevant medical history was present. On clinical examination the patient had good oral hygiene and deep pockets Table 1 for the pocket depth at 15, 16, 17, 26, 27, 36, 37, 46 and 37 region.
| Region(tooth number) | Pocket depth(mm) |
|---|---|
| 25, 26 | 7 mm |
| 35, 36 | 7 mm |
| 36, 37 | 13 mm |
| 17, 16 | 13 mm |
| 16, 15 | 7 mm |
| 46, 47 | 7 mm |
| 46 buccal | 10 mm |
Table 1. Pocket depth for each region in case 1 before the treatment.
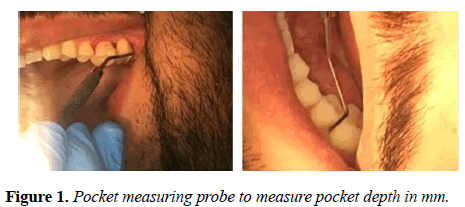
Pocket measuring probe was used to measure pocket depths and it was (7-13) mm depth and at some regions more than that as shown in Figure 1.
The case was diagnosed as localized periodontitis. Routine blood and X-ray investigation were performed.
Treatment started with general scaling and polishing for the upper, lower jaw due to the presence of calculus in addition to root planning (SRP) at the pocket region, oral hygiene instruction were given, too. Patient condition was assessed every one month by using pocket measuring probe to measure pocket depth and X-rays. In addition to one week recall to assess the oral hygiene maintenance by the patient, and a diode laser treatment was performed for each affected pocket.
The informed consent was signed by each patient in addition to the patient agreement to be treated by 940 nm laser according to the form as shown in Figure 2.
No local anaesthesia was given during treatment. No antimicrobial agent was prescribed no periodontal dressing was used.
Treatment took three month with one a week recall for laser treatment, Night guard was not used through the period of treatment.
Laser parameters
Laser biolase epic 940 nm wavelengths were used with an output power of 80 mw. In pulsed mode of 50% duty cycle the delivery system was an optical fibre of 300 um diameter, each surface of the pocket was irradiated for 20 second exposure time at each pocket. The treatment was repeated once a week.
Case two
39 old male, non-smoker with good oral hygiene. His chief complaint was pain on chewing in between tooth number 36, 37. He was treated previously by surgical excision to the lingual papilla between the previously mentioned teeth.
On x ray periapical view a deep pocket at 36, 37 regions was obvious due to vertical bone resorption. Pocket depth more than 13 mm was measured using pocket measuring probe. Root canal treatment was performed to tooth 36 due to the presence of deep filling with an obvious lamina dura on the mesial root of the tooth in addition to the dull pain that the patient was complaining of. Followed by laser treatment to the pocket region as previously mentioned case. There was an improvement with in the first month. The pocket depth was decreasing and no pain was present.
Results
No adverse effect was recorded in both cases postoperatively; no antibiotic or analgesic was prescribed post operatively.
First case
There was no pain or bleeding in the pocket region from the first visit in addition to the gradual reduction in the pocket depth according in between visits according to the Table 2.
| Date of visit | Tooth number with the pocket | The depth of the infrabony pocket |
|---|---|---|
| 4th Visit | 26, 27 | 4 mm, 6 mm |
| 36, 37 | 4 mm | |
| 5th Visit | 26 distally, 27mesially, 27 distally | 3 mm, 5 mm, 5 mm |
| 46 distally, 47mesially | 5 mm, 3 mm |
Table 2. Pocket depth at visit 4 and 5 using the pocket measuring probe.
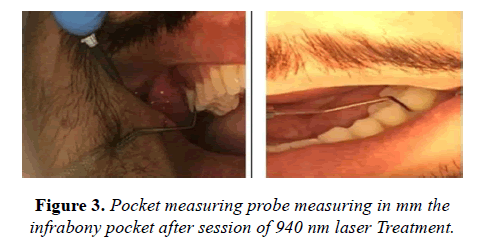
With the absence of bleeding during probing the gingival pockets through the pocket measuring probe during the routine examination was obvious as shown in Figure 3.
Radiographic examination (x-ray)
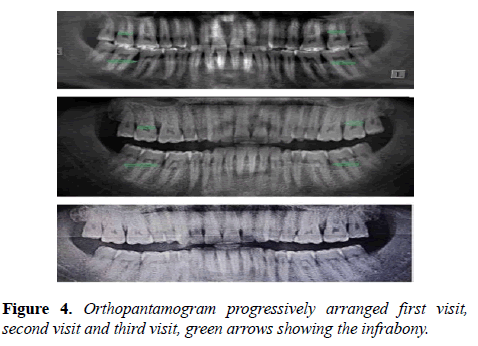
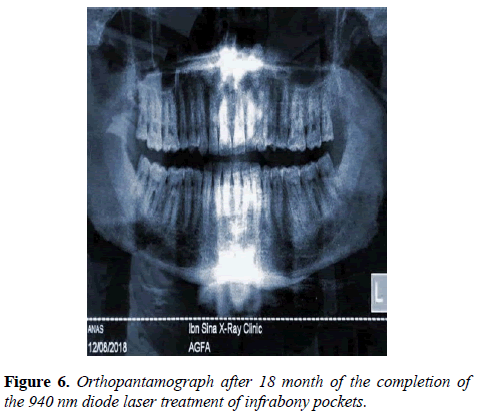
Orthopantamogram X ray (OPJ) was used once a month to assess the progress in the treatment Figure 4.
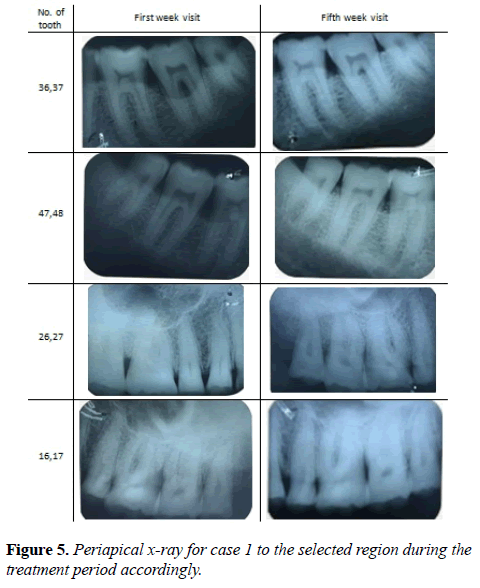
For more details in between visits periapical x ray was recommended Figure 5.
The OBJ was taken to the patient as shown in Figure 6 after 18 month of his last treatment visit. During the routine check-up there was 5 mm periodontal pocket at tooth number 26, 27. There was no complained by the patient of pain or bleeding from the periodontal ligament. The classical treatment of scaling and polishing was performed at the pocket site.
Second case
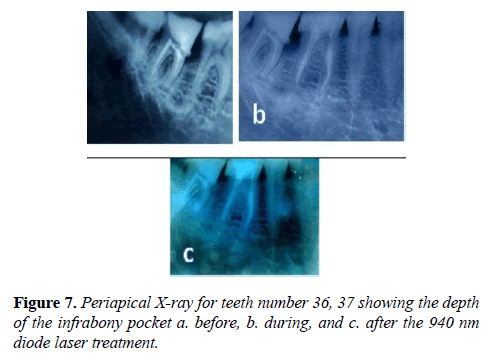
The same previously mentioned precautions were taken for the first treated case. Clinical examination, using the pocket measuring probe and Periapical X-ray were used since the case is locally present bone resorption due to tilted teeth 36, 37 as shown in Figure 7.
Discussion
Laser-tissue interaction (i.e. the behaviour of light in the tissue) is a sensitive process that depends on the incident wavelength, the incident power density, mode of operation and the exposure time. In addition to the tissue content and its optical property like refractive index and absorption coefficient.
There is no specific energy density at 940 nm used to stimulate acceleration of bone regeneration. The conflict may be due to the presence of variable type of bone in human body size as well as in volume. Jawad et al. in vitro study reported that 22.92, 45.85 and 91.79 J/cm2 energy densities for 3-6 min/day for 7 days were successful in stimulating osteoblast activity. He stated that cell proliferation increases with increasing laser power [8]. While Atasoy et al. reported that 5, 10, 20 J/cm2 energy densities at 940 wavelength were used. The increase in fibroblast activity was obvious at 10 J/cm2 energy density at week 4 [9].
Other studies by Mahmood et al. in vivo clinical study reported that 940 nm stimulate bone regeneration in dental socket after human tooth extraction using 11.9 W/cm2 power density without mentioning the exposure time [10].
Andreas et al. reported in his review of regenerative periodontal treatment that there is always a chance of tooth loss due to progressive bone resorption after conventional treatment for deep pocket ≥ 6 mm in depth and bifurcation involvement. Conventional non-surgical or surgical treatment has usually been associated with formation of long periodontal attachment on almost the entire periodontally exposed and instrumented root surface rather than periodontal regeneration [11].
In this work we used 940 nm wavelength lasers at 56 W/cm2 and the results were encouraging to regenerate the periodontal tooth supporting structure.
940 nm wavelengths have an absorption coefficient in blood about 0.25 mm-1 scattering coefficient about 0.64 mm-1 for an optical extension of 0.86 mm-1 [12]. If we cancel the reflected part of the laser beam which is 0.34 mm-1 [13] that occur at the first interface then the diffused laser beam through the variable refractive index of the clotted blood, the remaining power seem to be enough to regenerate the periodontal support of the tooth structure after sterilization of the area, this finding is in agreement with [10,12,14].
Recommendation
Laser treatment using 940 nm diode lasers to treat periodontitis and infrabony pockets service as adjunctive treatment to the conventional scaling and polishing. Laser treatment should be considered as alternative to surgical treatment to regenerate periodontal support to human teeth.
References
- Grant DA, Stern. IS, Everett. FG, Periodontics in the tradition of Orban and Gottlieb, Text Book Fifth edition, The C.V. Mosby Company, St. Louis. London 1979, Ch 14, page 280.
- Newman Mg, Takei H, Klollevold P, et al. Crranza’s Clinical Periodontology, 12th edition, Saunders Title, ISBN:978-0-32-18824-1, copy right 2015, Ch 16, Page 160.
- Barnard D. Essentials of periodontology and periodontics. Br J Oral Maxillofac Surg. 1976;13(3):295.
- Pifferi A, Torricelli A, Taroni P, et al. Optical biopsy of bone tissue: a step toward the diagnosis of bone pathologies. J Biomed Opt. 2004;9(3):474-80.
- Bashkatov AN, Genina EA, Kochubey VI, et al. Optical properties of human cranial bone in the spectral range from 800 to 2000 nm. InProc. SPIE. 2006; 6163:616310.
- Mileto TN, Azambuja FG. Low-intensity laser efficacy in postoperative extraction of third molars. RGO-Revista Gaúcha de Odontologia. 2017;65(1):13-9.
- Oliveira FA de, Matos AA, Matsuda SS, et al. Low level laser therapy modulates viability, alkaline phosphatase and matrix metalloproteinase-2 activities of osteoblasts. J Photochem Photobiol B. 2017;169:35-40.
- Jawad MM, Husein A, Azlina A, et al. Effect of 940 nm low-level laser therapy on osteogenesis in vitro. J Biomed Opt. 2013;18(12):128001.
- Atasoy KT, Korkmaz YT, Odaci E, et al. Therapy the efficacy of low-level 940 nm laser with different energy intensities on bone healing. Braz Oral Res. 2017;31:e7.
- Mahmood AS, Hammoodi NH. Clinical Assessment of Tissue Healing of Extracted Sockets Irradiated with 940 Nm Diode Laser. Iraqi dent j. 2015;37(3):124-8.
- Stavropoulos A, Sculean A. Current Status of Regenerative Periodontal Treatment. Curr Oral Health Rep. 2017;4(1):34-43.
- Vuylsteke M, Dorpe J Van, Roelens J, et al. Endovenous laser treatment: a morphological study in an animal model. Phlebology. 2009;(4):166-75.
- Cui W, Ostrander LE, Lee BY. In vivo reflectance of blood and tissue as a function of light wavelength. IEEE T BIO-MED ENG. 1990;37(6):632-9.
- Mirdan BM. A 980 nm Diode Laser Clot Formation of the Rabbit’s Dental Sockets after Teeth Extraction. Iraqi J Laser. 2012;11:37-42.