- Biomedical Research (2011) Volume 22, Issue 1
Measuring patient?s skin dose during total skin electron therapy using MOSFET
H. I. Al-Mohammed*
King Faisal Specialist Hospital and Research Centre, Department of Biomedical Physics, MBC # 03, POB 3354, Riyadh 11211, Saudi Arabia
- *Corresponding Author:
- H. I. Al-Mohammed
King Faisal Specialist Hospital & Research Centre
Dept of Biomedical Physics
MBC # 03, POB 3354
Riyadh 11211, Saudi Arabia
Accepted date: August 24 2010
Abstract
It is vital to measure the dose to the patient's skin during the treatment of total skin electron therapy (TSET). Purpose of the present study is to determine the benefits of using One-Dose MOSFET detectors in the treatment of mycosis fungiodes with TSET protocol. During the study six patients with advanced stage of (MF) were treated by (TSET) using a six dual-field Stanford technique. One-Dose MOSFET detectors (Metal oxide semiconductor field effect transistor) were used to obtain the real-time skin dose during the treatment and then com-pared it with the prescribed dose. The One-Dose MOSFET detectors results showed a rea-sonable agreement with prescribed doses especially in the flat areas of the body. One-Dose MOSFET detectors are prober detector to be used for TSET. They have the advantages of an immediate readout after irradiation, small size, and permanent storage of dose, wireless set-up and factory calibration.
Key words
Skin dose; Total skin electron therapy; One-Dose MOSFET; mycosis fungoides (MF); erythematous.
Introduction
Cutaneous T cell lymphomas (CTCL) represent a hetero-geneous group of T-cell malignancies that commonly ma-nifest in the skin, but can ultimately involve the lymph nodes, blood, and visceral organs [1,2]. By far the most common variant of CTCL is mycosis fungoides and its leukemic variant Sézary syndrome, which occurring in about 5% of all cases of mycosis fungoides (MF) [2]. MF is a malignant lymphoma that imposes a tremendous physical as well as psychological burden for patients be-cause of the highly visible nature of the disease and the lack of available curative therapy [2]. MF characterized by the infiltration of the skin with plaques and nodules composed of T-lymphocytes [2].
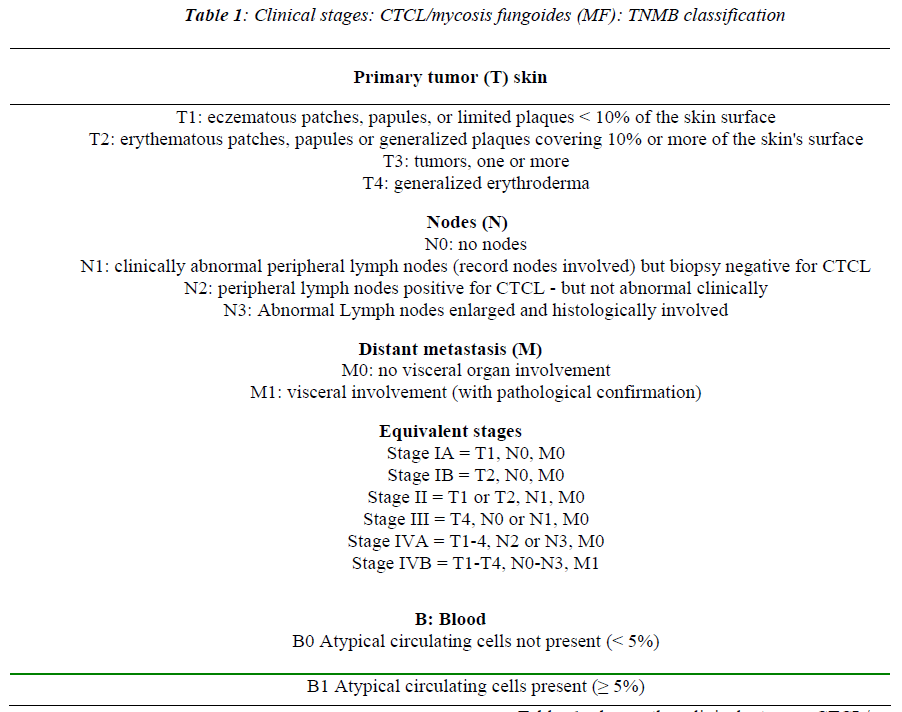
Occurrence of MF increases with age and it occurs more frequently in men than in women, it is approximately twice as common in men as in women and it is more common in blacks than in Caucasians, blacks have twice the incidence of whites, regardless of sex and age [3,4]. MF presents in early stages with patches and plaques that affect any area of the skin which then evolve into palpable plaques [5]. Later stages are characterized by the onset of tumors and erythroderma eventually with blood, lymph node and/or systemic involvement which then lead to in-fection as the skin turns into ulcerating, necrotic tumors [6,7]. Diagnostic of MF is considered to be challengeable and difficult due to the varied clinical and histological the disease [8]. However, the prognosis of MF is best esti-mated using the tumor-node-metastasis-blood (TNMB) staging criteria that shown in Table 1 [9].
The lesion is superficial with depth of 1 cm which means that the treatment has to cover the major portion of the body and has to be performed with electron beams of an average energy of 3–5 MeV [10].
The aim of this study is to determine an acceptable dose variation using One-Dose MOSFET detectors in the treatment of mycosis fungoides with total skin electron beam and compare it with the electron prescribed dose.
Materials and methods
Patient’s dosimetry
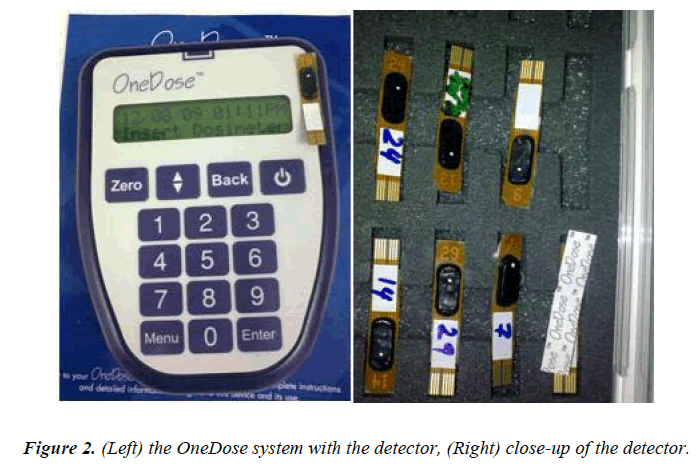
One-Dose MOSFET (Sicel Technologies,Inc, Morrisville, NC, USA distributed by MedTec, Orange City, IA,USA) detectors were used to obtain real-time dose measure-ments of skin does during the treatment of total skin electron therapy (TSET) and then compare it with the pre-scribed dose. The system is small with a measured area of 300 × 50 μm and it comprised of a wireless detector that is easy to use and is small in size, measuring 3.5 × 0.7 cm2. The accuracy of the detectors, as specified by the manufacturer, is ± 1.0 cGy for a dose of less than 20 cGy and ±5% for a dose of 20 to 500 cGy (Sicel Technologies Inc). The detectors are factory calibrated with a Co-60 beam with full build-up conditions. They are normalized to a 6-MV photon beam; each detector is valid for one used only [11].
TSET protocol
TSET is the treatment method based on Stanford tech-nique. It based on delivering twelve fields techniques; and divided into superior and inferior fields each one contains six fields. The superior fields are anterior, posterior, ante-rior, posterior, and four obliques. The inferior fields are anterior, posterior, and four obliques [12]. The total dose prescribed is 3000 cGy delivered in 20 fractions over a period of ten weeks [12], using 6 MeV of Varian Linac 2300 C/D linear accelerator (Varian Medical Systems, Inc., of Palo Alto, California, USA).
Each week a total of 300 cGy per fraction is delivered to the skin in four days treatment sessions, for prescription dose to each point 100 cGy. The treatment protocol is based on delivering of the treatment to only three fields in one session in order to make the treatment time shorter and then treating the other three fields in the next ses-sion[12]. The treatment accuracy and precisely were checked three times. First in the first day of the treat-ment, second, at the middle of the treatment session and finally at the end of the treatment by using One-Dose MOSFET detectors. All the twelve fields are treated with half of the dose per field. Areas of the skin that are known to receive a lower-than-prescribed dose are supplemented with additional electron boost fields later on after the treatment.
Patient treatment procedure
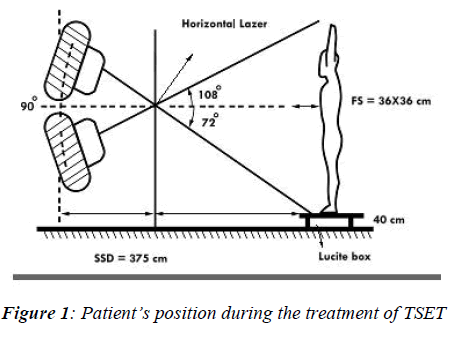
Six patients were selected for this study and the clinical and pathological characteristic of the patients are shown in Table 2. All patients were treated for their MF by the TSET protocol that used at King Faisal Specialist Hospi-tal and Research Center, Department of Radiation Oncol-ogy, Riyadh, Saudi Arabia. The protocol called for a standing position using dual angled fields in order to achieve the greatest dose uniformity along the patient's longitudinal axis (the height of the patient) as suggested by AAPM report 23 [1]. The treatment distance is an ex-tended source to skin distance (SSD) of (375 cm) with field-size 36 cm X 36 cm. A wooden frame with height of 40 cm was used to provide a mount for the large acrylic scattered. It is also used to raise the height of the patient’s feet, where under-dosing could occur during the treat-ment. Fixed foot patterns drawn on the wooden base to insure the position reproducibility of all the different standing positions and to assist in the treatment setup. A set of ropes drape down from the ceiling in the treatment room to provide support for the patient as one stands for treatment as shown in Figure 1. The collimator angle is zero where the gantry angles are one set 18 degrees above horizontal, and the other angled 18 degrees below horizontal, so that the dose distribution is uniform verti-cally from head to toe and that beam points above pa-tient’s head and below patient’s feet, respectively, in or-der to minimize contaminant x-ray dose. No degrader was used in front of the patient. We have used a normal dose rate of 400 Mu/min on a Varian Linac 2300 C/D linear accelerator. Shields are used for eyes, nails, and toes as prescribed.
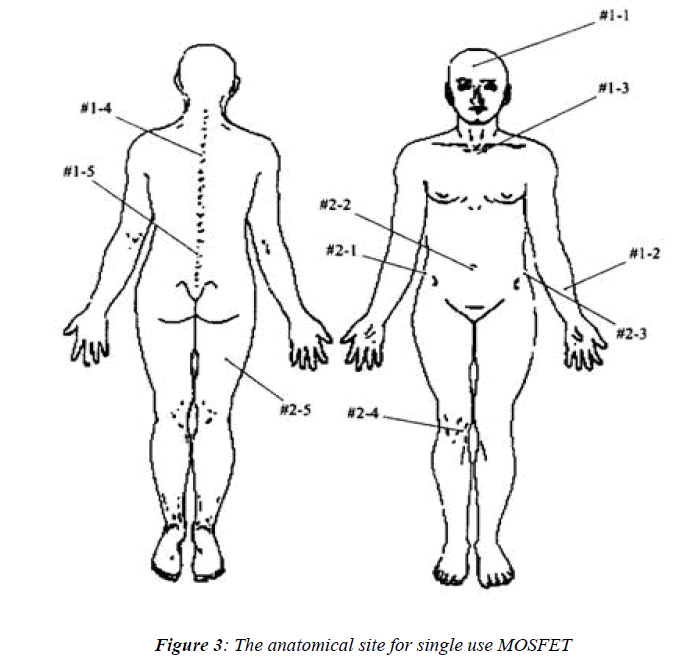
One-Dose MOSFET detectors which are shown in Figure 2, were first zeroed by the handheld reader and then were placed at ten selective anatomical points which are shown in Figure 3, for every patient. Following the treatment the detectors were collected and then each detector was placed in the handheld reader, and the measured doses were recorded.
Statistical analysis
Data from each sample were run in duplicate and ex-pressed as means ± SD (cGy, n = 6 patients). The results were compared using one-way ANOVA analysis fol-lowed by Tukey’s test for multiple comparison tests. Means were considered significantly if P < 0.05.
Results
Figure 1 shows the patient’s position during the treatment of TSET. Figure 2 shows the One-Dose MOSFET system (left) with the detector and close-up of the detector (right). Figure 3 shows the anatomical site for single use MOS-FET.
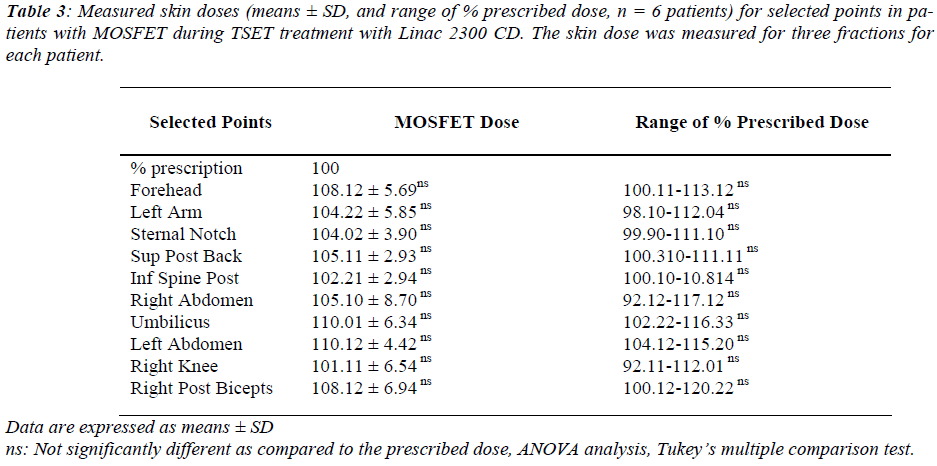
Table 1 shows the clinical stages: CTCL/mycosis fun-goides (MF): TNMB classification. Table 2 represents the clinical pathologic characteristics of the patients (n = 6) with cutaneous T-cell lymphoma (mycosis fungoides). Table 3 shows the measured skin doses (means ± SD, and range of % prescribed dose, n = 6 patients) for selected points in patients with MOSFET during TSET treatment with Linac 2300 CD. The skin dose was measured for three fractions for each patient.
Discussion
Total skin electron therapy (TSET) is a complex method of delivering superficial radiotherapy to entire skin sur-face. However, it remains one of the most effective modes of treatment for mycosis fungoides. The confined progno-sis of treatment considered to be good if the patients di-agnosed in the early stages [13] the most widely used TSET method is the dual six-field technique known as the Stanford method [12].
Using One-Dose MOSFET detectors is an immediate rea-dout after irradiation. It has the privileges of small size, permanent storage of dose, wireless set-up and factory calibration [14, 15]. It is simple to use with no modifica-tions to the unit is required and no sophisticated treatment apparatus is necessary , which thus make the One-Dose MOSFET detectors compliant and effective in evaluation of prescribed skin dose variation during total skin electron irradiation for treatment of mycosis fungoides [15].
The aim of this study is to determine an acceptable dose variation using One-Dose MOSFET detectors in the treatment of mycosis fungoides with total skin electron beam and compare it with the electron prescribed dose.
In our current study One-Dose MOSFET detectors showed that for all measured points there was variation in skin surface dose that varies of 102% to 110% when comparing the surface prescribed dose as summarizes in Table 3. Range of percentage MOSFET dose to the fore-head points was not significantly different with mean and stander deviation range between 108.45 ± 1.91 and 103.63 ± 2.32 for all selected anatomical points as shown in Table 3. When the measured skin dose compared to prescribed dose gave a range of 108.12 ± 5.69, where it showed the same effect to the left arm point with a range of 104.22 ± 5.85. For sternal notch it showed the range of 104.02 ± 3.90 sup post back point measured dose with single use MOSEFT showed a range of 105.11 ± 2.93.
The inferior spine post measured range dose was 102.21 ± 2.94. In the area of right abdomen showed the range of 105.10 ± 8.70. Umbilicus area range of measured dose by single use MOSFET was 110.01 ± 6.34. Left abdominal point area showed a range percentage of a measure dose of 110.12 ± 4.42. Right knee range of percentage meas-ured dose was 101.11 ± 6.54. The last point in the meas-urement was the right post biceps showed a range of 108.12 ± 6.94 as shown in Table 3.
Conclusions
The reproducibility of One-Dose MOSFET was found very well with a standard deviation of ± 5.51 % for all of the selected point’s measurements for all patients during the treatment of TSET. One-Dose MOSFET detectors results showed a reasonable agreement with prescribed doses with no significant different.
Acknowledgments
The author would like to thank our patients whom took a part of this study, and also the author would like to thank King Faisal Specialist Hospital and Research Center, Ri-yadh, Saudi Arabia for financially supporting this study.
References
- American Association of physicists in medicine task Group Report 23,”Total Skin Electron Therapy: Tech-nique and Dosimetry.” American Institute of physics (1988).
- Blasko J, Becker L, Griffin T, et al. Electron beam therapy of mycosis fungoides, Acta Radiol Oncol 1979; 18: 321-324.
- Parida D, Verma K, Chander S, et al. Total skin elec-tron irradiation therapy in mycosis fungoides using high-dose rate mode: a preliminary experience. Int J Dermatol 2005; 44 (10): 828-830.
- Anacaka Y, Aricana Z, Bar-Deromaa R, et al. Total skin electron irradiation: evaluation of dose uniformity throughout the skin surface. Med Dosim 2003; 28 (1): 31-34.
- Fink-Puches R, Cerroni L. Cutaneous T-cell lym-phoma and emerging therapies. Drug Discov To-day.2008; 5(1): e69:e79.
- Rajesh A Kinhikar et al. Clinical application of One-Dose™ MOSFET for skin dose measurements during internal mammary chain irradiation with high dose rate brachytherapy in carcinoma of the breast. Med. Biol. Phys. 2006; 51: N263-N268.
- Hoppe R, Fuks Z, Bagshaw M. Radiation therapy in the management of cutaneous T-cell lymphomas. Cancer Treat Rep. 1979; 63: 625-632.
- Briere T, Lii J, Prado K, et al. Single-use MOSFET radiation dosimeters for the quality assurance of mega-voltage photon beams. Phys Med Biol 2006; 51:1139-1144.
- Keehn C, Belongie I, Shistik G, et al. The diagnosis, staging, and treatment options for mycosis fungoides. Cancer Control 2007; 14 (2):102-111.
- Arulogun S, Prince H, Jonathan N, et al. Long-term outcomes of patients with advanced-stage cutaneous T-cell lymphoma and large cell transformation. Blood 2008; 11(8): 3082-3087.
- Bufacchi A, Carosi A, Adorante N, et al. In vivo EBT radiochromic film dosimetry of electron beam for total skin electron therapy (TSET). Physica Medica 2007; 23 (2): 67-72.
- Briere T, Lii j, Prado K, Gillin M, Beddar A. Single-use MOSFET radiation dosimeters for the quality as-surance of megavoltage photon beams. Phys Med Biol 2006; 51: 1139-1144.
- Page V, Gardner P, Karzmark A, et al. Patient do-simetry in the electron treatment of large superficial le-sions. Radiology 1970; 94 (3): 635-641.
- Theodore C, Lo M, Ferdinand A, et al. Dose considera-tions in total skin electron irradiation for mycosis fun-goides. Am J Roentgenol 1979; 132: 261-263.
- Al-Mohammed HI, Mahyoub FH, Moftah BA. Com-parative study on skin dose measurement using MOS-FET and TLD for pediatric patients with acute lym-phatic leukemia. Med Sci Monit 2010 (in press).