Research Article - Journal of Bacteriology and Infectious Diseases (2018) Journal of Bacteriology and Infectious Diseases (Special issue 1-2018)
Evaluation of one step malaria Anti-P.f/P.v cassette test in detection of malaria parasite in febrile patients.
Khadiga Ahmed Ismail1,2*1Parasitology Department Faculty of Medicine, Ain-Shams University, Cairo, Egypt
2Laboratory Medicine Department, College of Applied Medical Sciences, Taif University, Taif, Saudi Arabia
- *Corresponding Author:
- Khadiga Ahmed Ismail
Ain-Shams University
Cairo,
Egypt
Tel: 009660507921103, 00201000225787
E-mail: khadigaahmed68@yahoo.com
Accepted Date: May 31, 2018
Citation: Ismail KA. Evaluation of one step malaria Anti-P.f/P.v cassette test in detection of malaria parasite in febrile patients. J Bacteriol Infec Dis. 2018;2(1):43-45
Abstract
Malaria in hypoendemic area like Saudi Arabia presents a diagnostic challenge to laboratories. As the effect of war population migration from endemic area contribute to presenting the laboratory with diagnostic problems for which it may have little expertise available. This study was aimed to compare the accuracy of malaria Rapid Diagnostic antibody Tests, One Step Malaria Anti-P.f/ P.v Cassette Test with the microscopic examination as the gold standard. Between January 2015 to January 2018 blood samples were collected from 100 patients, attending the internal medicine department at King Abdelaziz specialized hospital at Taif, Saudi Arabia. Microscopy and One Step Malaria Anti-P.f/P.v Cassette Test were done and the accuracy was evaluated. In this study detected 45 (45%) malaria positive slides, while 42 (42%) positive samples were detected with One Step Malaria Anti-P.f/P.v Cassette Test. One Step Malaria Anti-P.f/P.v Cassette Test sensitivity (85.1%), specificity (92.4%), positive predictive value (90.4%), negative predictive value (88.4%) and diagnostic accuracy (89.1%). One Step Malaria Anti-P.f/P.v Cassette Test is considered one of the options in health areas especially with limited laboratory services despite the problems related to their diagnostic accuracy. However, this study showed that the accuracy of One Step Malaria Anti-P.f/P.v Cassette Test is not always satisfactory when performed in clinical laboratories and must confirmed with other tests.
Introduction
Malaria is a serious, sometimes fatal, parasitic disease characterized by fever, chills, and anemia and is caused by a parasite that is transmitted from one human to another by the bite of infected Anopheles mosquitoes. There are four kinds of malaria that can infect humans: Plasmodium falciparum, P. vivax, P. ovale, and P. malariae. In human, the infective stage is called sporozoites migrate to the liver where they mature and release another form, the merozoites. The disease is a major health problem in much of the tropics and subtropics. More than 200 million people in the world have malaria [1].
At the present, malaria is diagnosed by looking for the parasites in a drop of blood. Blood will be put onto a microscope slide and stained so that the parasites will be visible under a microscope. At the most recent, clinical diagnostic issues related to malaria are the detection of malaria antibodies in human blood or serum by immunoassay. The ELISA format and immunochromatographic format (rapid test) to detect antibody of malaria are available recently. Rapid and accurate diagnosis is the key to effective management of malaria cases in order to start early thus reduce morbidity and mortality caused by delayed or poor management of patients [2].
Presumptive diagnosis of malaria is based upon the presence of fever alone which leads to the overuse of antimalarial drugs. Fever paroxysms, the hallmark of malaria, occur when infected RBCs rupture and release parasite-derived molecules that stimulate theproduction of pro-inflammatory cytokines by the host [3]. Under ideal circumstances, the clinical suspicion of malaria would be confirmed by a laboratory test that is simple to perform, rapid, sensitive, specific, and inexpensive. Hence traditional malaria diagnosis based on the examination of stained blood smears under light microscope remains the gold standard for malaria diagnosis. In addition it can routinely detect parasitaemia levels as low as 40 parasites/μl, and experienced microscopists can detect as low as 5-10 parasites/μl of blood [4]. However, it is labor-intensive, time-consuming, requires technical expertise and the availability of a good quality microscope. Therefore, several alternative methods have been developed for malaria diagnosis including immunochromatographic (ICT) assays and molecular amplification methods. Each of these methods has strengths and weaknesses in terms of test parameters, cost and technical complexity [5-7].
Malaria rapid antibody tests are commercially available; most of them are ICT dipstick assays, based on the detection of malaria antibodies in blood flowing along a membrane containing specific anti-malaria antigens. This assay was found to be accurate, rapid and easy to perform and interpret. Moreover, it can be a useful tool for the detection of malaria in countries where both plasmodial species are co-endemic and where laboratory support is limited. Its sensitivity has proved similar to the sensitivity of microscopy in both developing and developed countries so the aim of this study is to evaluate One Step Malaria Anti-P.f/P.v Cassette Test in diagnosis of malaria.
Subjects and Methods
Subjects
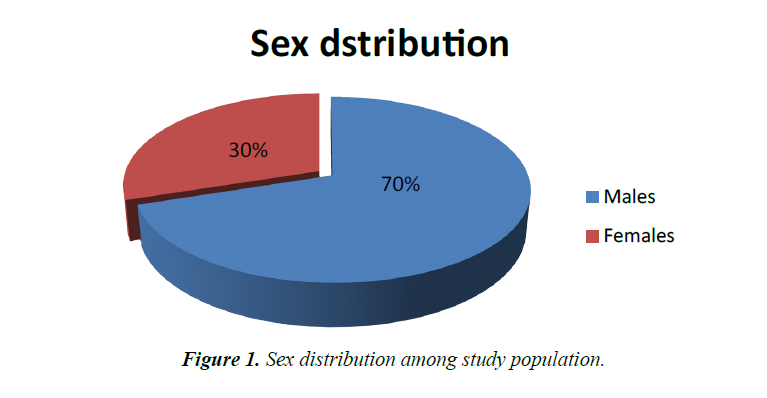
A total of 100 patients included in this study, presenting with fever > 38 °C, associated in some cases with shivering and body aches, were clinically diagnosed as malaria infection. The patients were 70 males and 30 females with an average age of 17-50 years, attending the internal medicine department at King Abdelaziz specialized hospital, Taif, KSA, in the period from January 2015 to January 2018. Finger-prick blood samples were collected and tested for the presence of Plasmodium parasites using microscopic examination of thick and thin blood films, and One Step Malaria Anti-P.f/P.v test.
Microscopic examination of blood smears
Thick and thin blood films were prepared, stained with fresh 10% Giemsa's solution and examined using X l000 oil immersion magnification. The slides were reported negative only when no parasites were detected in 200 fields of each thick film. Stained thin film preparations of positive thick films were examined to determine the species: P. oval. P. falciparum, P. vivax, P. malariae or mixed infection. Parasitemia was evaluated in 100 fields of thin films against the leucocytes counts taken from records of the patients, based on the equation: number of parasites/μl=total parasite count/WBC count X the total leucocyte count/μl.
One step malaria anti-P.f/P.v test
The rapid malaria test (SD, BIOLINE Inc., Germany) was performed according to the manufacturer’ instructions. Briefly, a 20 μl of blood was added to a sample well in a microtiter plate and mixed with two drops of assay diluent. The specimens were then allowed to migrate to the top of the strip. After ten minutes, read the test. Positive and negative control samples were included with each batch tested and results were visually interpreted immediately. A positive control line should always be present at the top of the strip to verify that the test strip is functional. If this is the only line that appears, the test is considered negative for malaria. Appearance of a second line, adjacent to the positive control line, indicates the presence of a non-P. falciparum malaria parasite antibodies (P. vivax, P. ovalae, or P. malariae). When a third line is also present, this indicates a positive response for P. falciparum infection antibodies.
Statistical analysis
Collected data were coded, tabulated and introduced to a PC using the Statistical Package for Social Science (SPSS) for windows version 19.
Ethical considerations
Ethical approval for this study was obtained from the Ethics Review Committee of the College of Applied Medical Sciences at Al-Taif University. Moreover, all patients included in the study were informed of the study objectives and a written signed consent was taken from each one of them.
Results and Discussion
Results are shown in Figure 1 and Tables 1 and 2. Clinical diagnosis of malaria is unreliable due to the non-specific nature of signs and symptoms of malaria leading to over-diagnosis and over-treatment [8]. Rapid diagnostic tests are recommended in situations exceeding microscopy capability, such as in an outbreak or in occupationally exposed groups [9].
Table 1.Validation of One step test for diagnosis of malaria using direct microscopy as gold standard.
| Applied tests | Direct microscopy | Sens. % | Spec. % | PPV % | NPV % | DA % | ||
|---|---|---|---|---|---|---|---|---|
| One Step Anti-P.f/P.v | +ve (%) | -ve (%) | Total (%) | 85.1 | 92.4 | 90.1 | 88.4 | 89.1 |
| +ve (%) | 38(38%) | 4 (4%) | 42(42%) | |||||
| -ve (%) | 7(7%) | 51(51%) | 58(58%) | |||||
| Total | 45(45%) | 55(55%) | 100(100%) | |||||
Note- Sens.% = Sensitivity%, Spec.% = Specificity%
One Step Malaria Anti-P.f/P.v versus direct microscopy.
Table 2.Results of microscopy for detection of malaria species.
| Direct microscopy | Malaria species | Total | |||
|---|---|---|---|---|---|
| P. vivax | P. falciparum | P. malariae | Mixed | ||
| Positive | 37(37%) | 5 (5%) | 2(2%) | 1(1%) | 45(45%) |
| Negative | 55(55%) | ||||
| Total | 100(100%) | ||||
Our results showed that the differences in detection rates of microscopy, and One step anti- P.f/P.v test (45% and 42%, respectively) in 100 clinically suspected cases, our findings are in agreement with another observational study [10], in which malaria was diagnosed in 46.9% among patients with undifferentiated fever; and in contrast to Azikiwe et al., [11] results that demonstrated the antibody based method showed good level of sensitivity but, very unspecific.
Species differentiation in the positive samples by blood film examination showed higher prevalence of P. vivax (37%), than P. falciparum (5%), and P. malariae (2%). Mixed infections by P. vivax and P. falciparum presented 1% with increase prevelance of P. vivax. This goes with MacLean et al [12] who reports on the high levels of P. vivax disease activity in Asia.
One step anti- P.f/P.v test showed 4 false-positive samples that were negative by microscopy and 7 false-negative samples that were positive by microscopy, which is compatible with results obtained from previous studies [13] In explanation of false positivity the postulated hypothesized that One step anti- P.f/P.v test positive cases missed by microscopy might be individuals who had been treated but in whom antibodies persists Other. False negative results of One step anti- P.f/P.v test have been attributed to possible genetic heterogeneity of HRP2 or LDH expression, deletion or mutation of HRP2 or LDH gene, presence of blocking antibodies, or immune-complex formation [14].
To these diverse findings include test kit storage conditions in the field (manufacturers usually recommend 4-30°C as the optimal temperature range. Based on the results of this study, One step anti- P.f/P.v test is complementary to microscopy because they help expand the coverage of parasite-based diagnosis and minimize exclusive clinical diagnosis.
References
- Perkins Susan L, Schall JJ. A molecular phylogeny of malarial parasites recovered from cytochrome b gene sequences. J Parasitol. 2002;88(2):972-8.
- Hawkes M, Kain KC. Advances in malaria diagnosis. Expert Rev Anti Infect Ther. 2007;5(3):485-95.
- Ferreira MU, Nunes MS, Wunderlich G. Antigenic diversity and immune evasion by malaria parasites. Clin Diagn Lab Immunol. 2004;11(6):987–95.
- World Health Organization. New Perspectives: Malaria Diagnosis, Report of a Joint WHO/USAID: Informal Consultation held on 25-27 October 1999. Geneva, Switzerland, World Health Organization. 2000:4-48.
- Moody A, Hunt-Cooke A, Gabbett E, et al. Performance of the OptiMAL antigen capture dipstick for malaria diagnosis and treatment monitoring at the hospital for tropical diseases, London. Br J Haematol. 2000;109:891-4.
- Malik S, Khan S, Das A, et al. Plasmodium lactate dehydrogenase assay to detect malarial parasites. Natl Med J India. 2004;17(5):237-9.
- Johnston SP, Pieniazek NJ, Xayavong MV, et al. PCR as a confirmatory technique for laboratory diagnosis of malaria. J Clin Microbiol. 2006;44:1087-9.
- Reyburn H. New WHO guidelines for the treatment of malaria. BMJ. 2010;340:2637.
- WHO. The use of malaria diagnostic tests. Manila: WHO regional office for the western pacific (WPRO). 2004.
- Neuberger A, Zaolan O, Tenenboim S, et al. Malaria among patients and aid workers consulting a primary healthcare centre in Leogane, Haiti, November 2010 to February 2011: A prospective observational study. Euro Surveill. 2011;16(13):19829.
- Azikiwe CC, Ifezulike CC, Siminialayi IM, et al. A comparative laboratory diagnosis of malaria: microscopy versus rapid diagnostic test kits. Asian Pac J Trop Biomed. 2012;2(4):307-10.
- MacLean DJ, Demers AM, Ndao M, et al. Twenty years of malaria surveillance in Canada; epidemics missed, lessons learned. Emerg Infect Dis. 2004;10:1195-201.
- Iqbal J, Muneer A, Khalid N, et al. Performance of the OptiMAL test for malaria diagnosis among suspected malaria patients at the rural health centers. Am J Trop Med Hyg. 2003;68:624-8.
- Chaijaroenkul W, Wongchai T, Ruangweerayut R, et al. Evaluation of rapid diagnostics for Plasmodium falciparum and P. vivax in Mae Sot malaria endemic area, Thailand. Korean J Parasitol. 2011;49(1):33-8.