- Biomedical Research (2016) Volume 27, Issue 3
Effect of nasopharyngeal snorkel on respiratory function in patients with stroke.
Xuehua Pu, Xiaofeng Chen, Jilu Ye*
Department of Intensive Care Unit, Taizhou People’s Hospital, Taizhou 225300, China
- Corresponding Author:
- Jilu Ye
Department of Intensive Care Unit
Taizhou People’s Hospital, China
Tel: +27219593229/2190
Fax: +278615107002
E-mail: ombamalu@uwc.ac.za
Accepted Date: March 16, 2016
Abstract
Stroke causes significant mortality and morbidity. The clinical value of the nasopharyngeal snorkel was investigated in stroke patients with disorders of consciousness. A total of 155 stroke patients were randomly divided into two groups: a nasopharyngeal snorkel was used in the treatment group (n=78) and an oropharyngeal snorkel was used in the control group (n=77). The PaO2 and PCO2 of both groups improved 30 minutes after placement of the nasopharyngeal or oropharyngeal snorkel, with a reduction of systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR). The improvements in PCO2 was significant in the nasopharyngeal snorkel group (40.9 ± 3.3) compared with oropharyngeal snorkel group (47.8 ± 5.3) (P<0.05). Tracheal intubation was carried out in 15 (19.2%) patients in the nasopharyngeal snorkel group compared with 31 (40.3%) patients in the oropharyngeal snorkel group. Pulmonary infection occurred in 11 (14.1%) patients in the nasopharyngeal snorkel group and 19 (24.7%) patients in the oropharyngeal snorkel group. The incidence of tracheal intubation and pulmonary infection were significantly lower in the nasopharyngeal group (P<0.05). The placement of a nasopharyngeal snorkel was an effective treatment for upper airway obstruction in stroke patients.
Keywords
Nasopharyngeal snorkel, Oropharyngeal snorkel, Tracheal intubationm, Pulmonary infection
Introduction
Stroke is a disease with a high mortality rate and high morbidity [1-3]. Stroke patients are often hospitalized for multiple complications [4-6], which may extend the length of stay, increase healthcare costs, and increase mortality rates [7]. Severe stroke patients often experience disorders of consciousness, such as muscle relaxation of the throat and tongue, which may block the airway. Then they will have hypoxia and carbon dioxide retention, and even acute respiratory failure. Also they may be unable to expectorate sputum independently, resulting in drainage issues, thereby causing pulmonary infection. Pulmonary infection is the most common complication of acute stroke [8]. Traditional methods have employed tracheotomy in the vast majority of stroke patients with disorders of consciousness [9,10], but this method increases the risk of lung infection, and prolongs the need for mechanical ventilation and intensive care unit (ICU) stay [11]. Therefore, our attention is focused on providing care to acute stroke patients without the use of artificial airways. Improving the airway management of these patients can reduce the tracheal intubation (tracheotomy) rate and incidence of lung infection.
Numerous studies have shown that the use of a nasopharyngeal snorkel can relieve upper airway obstruction and allow air to flow smoothly in patients with sleep apnea [12,13]. The proportion of patients with sleep-disordered breathing is significantly higher after a stroke compared with the healthy population [14,15]. However, the clinical role and value of the nasopharyngeal snorkel for stroke patients remains unclear. We hypothesize the placement of nasopharyngeal snorkels can relieve airway obstruction in stroke patients. Besides, it is convenient for sputum suction through nasopharyngeal snorkel. This study investigated the use of nasopharyngeal and oropharyngeal snorkels in stroke patients without the use of an artificial airway. These two methods of pipe placement were compared in terms of efficacy, and relative advantages and disadvantages.
Methods
Clinical data
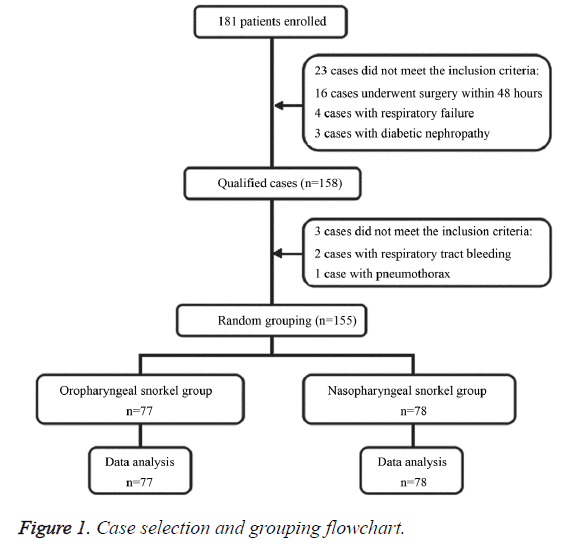
This study included 155 stroke patients without respiratory failure or tracheal intubation who were admitted to Intensive Care Unit (ICU) of Taizhou people’s hospital between May 2011 and May 2013. Individuals comprised 88 males and 67 females, aged 30 to 95 years with a mean age of 73 years, an APACHE II score of between 5 and 13, and a Glasgow Coma score (GCS) of between 7 and 13. The inclusion criteria consisted of: stroke patients without artificial airways or respiratory failure who stayed in the ICU for 12 hours; disorders of consciousness of sleepiness, drowsiness, or light coma, each one had a GCS score of between 7 and 13; aged 18 to 98 years old. We excluded patients undergoing neurosurgery within 48 hours; patients with other serious organ damage or dysfunction; patients with central respiratory failure. The medical staff involved in the study received training on randomization techniques. Patients were randomly divided into either the nasopharyngeal snorkel group (n=78) or the oropharyngeal snorkel group (n=77). Age, sex, APACHE II score, GCS, history of chronic obstructive pulmonary disease, disease classification, and other patients characteristics were comparable between the two groups (Figure 1). This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Taizhou People’s Hospital. Written informed consent was obtained from all participants.
Treatment
Each patient in two groups received oxygen therapy using a high-flow humidification oxygen system (Fisher & Paykel MR850 humidification, Fisher & Paykel Healthcare, New Zealand). A nasopharyngeal snorkel was placed on individuals in the treatment group, with the model type based on patients’ height and weight. The length of the nasopharyngeal snorkel was based on the distance between the patient's nose and the earlobe, plus 3 cm. The snorkel was coated with sterilized paraffin oil prior to placement, the exposed latex tubes were fixed with tape, and the surface of the nasal mucosa was sprayed with ephedrine hydrochloride. The nasopharyngeal snorkel was replaced daily to prevent the development of a mucus plug. Suctioning was performed with a silicone rubber suction tube that went through the nose/mouth or through the nasopharyngeal snorkel. An oropharyngeal snorkel was placed on individuals in the control group, with model size based on patients' height and weight. Suctioning was performed with a silicone rubber suction tube that went through the nose/mouth or through the oropharyngeal snorkel. The technical line is shown in figure 2. The medical staff involved in the study received training on nasopharyngeal and oropharyngeal snorkel placement. The negative pressure of suction for patients in both groups maintained at -30 to ~ -50 mmHg, with suction performed by experienced nurses. The indications for immediate tracheal intubation were [16]: worsening neurological status; deterioration of respiratory function; respiratory rate >35 breaths/min or significant accessory muscle activity and paradoxical abdominal motion; by increased oxygen inhalation, SpO2 <92% or PaO2 <65 mmHg; pH <7.3 and progressive increases in PaCO2 > 50 mmHg or PaCO2; loop instability.
Measurement of clinical outcomes
The SBP, DBP, HR, SpO2, and PaCO2 of patients in both groups were measured prior to placement of the snorkel (T0), and 10 min (T10), 20 min (T20), and 30 min (T30) after placement of the snorkel. Spontaneous ventilation and the intubation rate, and the incidence of lung infection, according to the diagnostic criteria of lung infection, were recorded [17].
Statistical analysis
Statistical analysis of the data was carried out using SPSS 19.0 (SPSS Inc, Chicago). Measurement data were expressed as mean ± standard deviation, and were statistically analyzed using t-test. The disaggregated data were compared using χ2 test, continuity correction χ2 test, or exact probabilities. A P value <0.05 was considered to be statistically significant.
Results
Patient characteristics
The nasopharyngeal snorkel group and the oropharyngeal snorkel group comprised 41 males and 37 females, and 40 males and 37 females, respectively. There were no significant differences between the two groups in terms of gender, age, weight, and GCS score (Table 1).
| Oropharyngeal snorkel group | Nasopharyngeal snorkel group | P value | |
|---|---|---|---|
| Gender (male/female) | 42/35 | 46/32 | 0.578 |
| Age (years) ± Mean (SD) | 63 ± 33 | 61 ± 34 | 0.711 |
| Weight (kg) ± Mean (SD) | 75.3 ± 17.2 | 79.2 ± 18.5 | 0.176 |
| Mean GCS score | 8.9 ± 1.5 | 9.1 ± 1.3 | 0.376 |
| Mean APACHEII mean (SD) | 23.5 ± 2.3 | 24.1 ± 2.5 | 0.122 |
| COPD history (cases) | 9 | 10 | 0.83 |
Table 1. General information of the two groups (x ± s).
Respiratory and circulatory changes
The PaO2 and PCO2 of the oropharyngeal snorkel group improved (P<0.05), while SBP, DBP, and HR decreased 30 minutes after placement of the oropharyngeal snorkel (P<0.05). The respiratory status of patients in the nasopharyngeal snorkel group was improved compared with the oropharyngeal snorkel group 30 minutes after placement of the snorkel, with significant improvements in PCO2, SBP, DBP, and HR (P<0.05) (Table 2).
| Indicators | Oropharyngeal snorkel group | Nasopharyngeal snorkel group | ||||||
|---|---|---|---|---|---|---|---|---|
| T0 | T10 | T20 | T30 | T0 | T10 | T20 | T30 | |
| SBP | 179.2±11.6 | 168.3±9.3a | 165.3±7.8a | 165.5±5.9a | 175.3±12.8 | 140.5±10.1ab | 150.5±9.2ab | 149.8±8.2ab |
| DBP | 113.5±7.3 | 101.5±9.3a | 100.5±8.3a | 100.3±7.3a | 110.2±7.2 | 90.2±10.2ab | 89.2±10.1ab | 88.1±9.9ab |
| HR | 91.4±5.2 | 85.4±5.9a | 84.4±5.5a | 84.7±5.8a | 86.9±6.1 | 76.9±8.1ab | 74.8±8.0ab | 74.3±7.7ab |
| RR | 18.9±3.5 | 17.9±4.9a | 16.8±4.7 | 16.9±5.1 | 19.3±4.1 | 15.3±6.1ab | 15.1±5.1ab | 14.7±5.3ab |
| PaO2 | 85.5±8.6 | 88.3±7.9a | 88.1±6.9a | 90.9±8.6a | 83.1±9.8 | 86.1±7.8a | 88.1±6.9a | 87.2±7.1a |
| PCO2 | 49.5±2.8 | 48.5±3.3a | 47.5±4.3a | 47.8±5.3a | 51.2±3.1 | 42.2±5.2ab | 41.3±3.2ab | 40.9±3.3ab |
Table 2. Comparison of breathing cycle indicator for patients in the two groups (x ± s).
There were 31 patients (40.3%) in the oropharyngeal snorkel group with tracheal intubation versus 15 patients (19.2%) in the nasopharyngeal snorkel group (P<0.05). There were 19 patients (24.7%) in the oropharyngeal snorkel group with pulmonary infection versus 11 (14.1%) patients in the nasopharyngeal snorkel group (P<0.05) (Table 3). The duration of ICU stay (20.5 days) was significantly shorter in the nasopharyngeal snorkel group compared with the oropharyngeal snorkel group (25.3 days) (P<0.05) (Table 3).
| Results | Oropharyngeal snorkel group (n=77) | Nasopharyngeal snorkel group (n=78) | P value |
|---|---|---|---|
| Pulmonary infection [Cases (%)] | 20 (26.0) | 10 (12.8)Δ | 0.038 |
| Tracheal intubation [Cases (%)] | 31 (40.3) | 15 (19.2)Δ | 0.004 |
| ICU stay (days) | 25.3 ± 2.3 | 20.5 ± 2.1Δ | 0.000 |
| Note: Compared with oropharyngeal snorkel group, ΔP<0.05. | |||
Table 3. Comparison of complications in the two groups.
Discussion
Airway patency is an important factor in the prognosis of patients with stroke. The masseter muscle and mandibular joint of comatose stroke patients are relaxed, which can often result in the tongue falling, thereby partially or completely blocking the airway. This is the main cause of airway obstruction in patients with acute stroke. Rofes et al. [18] believed that the stroke can cause damage to the medullary center (V, VII, IX, X cranial nerve, and the nucleus of the solitary tract), which in turn causes bulbar palsy or bilateral cortical brain stem damage. This results in limited mobility of the tongue and throat muscles, with closure of the laryngeal vestibule and prolonged opening of the esophageal sphincter. Airway obstruction can also lead to ventilatory dysfunction, which can cause dysphagia and an increased risk of aspiration, and therefore an increased risk of aspiration pneumonia. Generally, only timely holding of the patient's lower jaw in a forward and up position (Jackson bit, commonly known as "jaw hold up") can remove the upper airway obstruction caused by a fallen tongue [6]. However, this can only be used as a temporary measure to improve symptoms.
Potential measures to solve the problem of a fallen tongue include placement of an oropharyngeal or a nasopharyngeal snorkel. The oropharyngeal snorkel has a wide range of applications in clinical and theoretical research. Although the oropharyngeal snorkel is easy to place, rarely causes damage or bleeding, it becomes loose easily, is difficult to fix in position, the hard material stimulates the oropharyngeal mucous membrane, and awake or uncooperative patients often find the snorkel unacceptable [19]. The clinical advantages of a nasopharyngeal snorkel include easy placement; flexible material; well tolerated; a lower incidence of nausea, vomiting, and laryngospasm response in comparison with oropharyngeal snorkel; easy to fix in position; and the snorkel can be used for a prolonged period of time [20]. In addition to preventing upper airway obstruction in patients with acute stroke, the biggest advantage of a nasopharyngeal snorkel is that it will not affect any other type of medically assisted ventilation measures. Scholars Nahmias et al. [21] placed a 5 mm nasopharyngeal snorkel on the epiglottis for treatment of sleep apnea syndrome, with a treatment success rate of 66.7%, and without any significant complications arising. Huo et al. [22] reported similar results. There have been several studies reporting on the use of the nasopharyngeal snorkel to improve upper airway ventilation both in China and internationally [23,24]. Moreover, the suction tube can effectively remove oropharyngeal secretions through the nasopharyngeal snorkel for stroke patients with swallowing difficulties [25], and in whom oropharyngeal secretions cannot be cleared. Lung infections are a common complication of stroke patients, with an incidence of up to 10% [26]. A nasopharyngeal snorkel can help maintain airway patency, and also help prevent endotracheal intubation of patients. Therefore, reducing the incidence of lung infections and improving the prognosis of stroke.
The nasopharyngeal snorkel had two main functions. Firstly, it maintains the smooth flow of air. Stroke patients with consciousness disorders usually breathe through their mouth, have dyspnea, significant accessory muscle activity and contradictory chest abdominal movement, all of which are caused by upper airway obstruction as a result of a reduction in throat muscle tension and a fallen tongue. These features are particularly common in patients who are obese or those with a history of snoring. Secondly, the snorkel promotes mucus drainage. Stroke patients with consciousness disorders usually have poor swallowing function and are unable to clear oral secretions and secretions expelled from the airways to the mouth; however, these can be removed by suction using the nasopharyngeal snorkel.
Our study showed that the placement of a nasopharyngeal or an oropharyngeal snorkel can effectively improve ventilatory dysfunction of stroke patients, improve hypoxia and carbon dioxide retention, which means that can relieve upper airway obstruction and maintain a smooth flow of air. Also we saw cardiovascular changes following insertion of a nasopharyngeal or an oropharyngeal snorkel. But the effect of the nasopharyngeal snorkel group was more obvious. We also found the placement of a nasopharyngeal snorkel can reduce the risk of pulmonary infection and intubation by effectively reducing suction. These results indicate that insertion of a nasopharyngeal snorkel is an effective way of solving airway obstruction in patients with stroke.
Limitations of this study include that only a single ICU center was used to carry out the research, the sample size was too small, and the time points for sampling PaO2, PCO2, SBP, DBP and HR were limited, which may have affected the final results. Additionally, this study only provided evidence for the management of clinical breathing in patients with stroke. The value of the nasopharyngeal snorkel in patients with stroke requires further investigation.
Acknowledgments
Science and Technology Support Project of Taizhou City (TS201236).
Conflicts of interest
All of the authors declare that they have no conflicts of interest regarding this paper.
References
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 2013; 127: 143-152.
- Hong KS, Saver JL, Kang DW, Bae HJ, Yu KH, Koo J, Han MK, Cho YJ, Park JM, Lee BC. Years of optimum health lost due to complications after acute ischemic stroke: disability-adjusted life-years analysis. Stroke 2010; 41: 1758-1765.
- Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, Albers GW, Kaste M, Marler JR, Hamilton SA, Tilley BC, Davis SM, Donnan GA, Hacke W; ECASS, ATLANTIS, NINDS and EPITHET rt-PA Study Group, Allen K, Mau J, Meier D, del Zoppo G, De Silva DA, Butcher KS, Parsons MW, Barber PA, Levi C, Bladin C, Byrnes G. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010; 375: 1695.
- Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke 2011; 42: 3214-3218.
- Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol 2010; 9: 105-118.
- Tong X, Kuklina EV, Gillespie C, George MG. Medical complications among hospitalizations for ischemic stroke in the United States from 1998 to 2007. Stroke 2010; 41: 980-986.
- Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 2003; 60: 620-625.
- Ji R, Wang D, Shen H, Pan Y, Liu G, Wang P, Wang Y, Li H, Wang Y. Interrelationship among common medical complications after acute stroke, pneumonia plays an important role. Stroke 2013; 44: 3436-3444.
- Andriolo BN, Andriolo RB, Saconato H, Atallah ÁN, Valente O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev 2015; 1: CD007271.
- Walcott BP, Kamel H, Castro B, Kimberly WT, Sheth KN. Tracheostomy following severe ischemic stroke: a population based study. J Stroke Cerebrovasc Dis 2014; 23: 1024-1029.
- Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J RespirCrit Care Med 2000; 161: 1530-1536.
- Kumar AR, Guilleminault C, Certal V, Li D, Capasso R, Camacho M. Nasopharyngeal airway stenting devices for obstructive sleep apnoea: a systematic review and meta-analysis. J LaryngolOtol 2014; 129: 2-10.
- Li SH, Wu DH, Bao JM, Shi HJ. Outcomes of upper airway reconstructive surgery for obstructive sleep apnea syndrome based on polysomnography after nasopharyngeal tube insertion. Chin Med J (Engl) 2013; 126: 4674-4678.
- Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med 2010; 6: 131-137.
- Sacchetti ML, Della Marca G. Are stroke cases affected by sleep disordered breathings all the same? Med Hypotheses 2014; 83: 217-223.
- Navalesi P, Frigerio P, Moretti MP, Sommariva M, Vesconi S, Baiardi P, Levati A. Rate of reintubation in mechanically ventilated neurosurgical and neurologic patients: evaluation of a systematic approach to weaning and extubation. Crit Care Med 2008; 36: 2986-2992.
- Chinese Thoracic Society. Guidelines for the diagnosis and treatment of community-acquired pneumonia. ZhonghuaJie He He Hu Xi ZaZhi 2006; 29: 651-655.
- Rofes L, Arreola V, Almirall J, Cabré M, Campins L, García-Peris P, Speyer R, Clavé P. Diagnosis and management of oropharyngeal Dysphagia and its nutritional and respiratory complication in the elderly. Gastroenterol Res Pract 2011; 2011: 818979.
- Buckley FP, Martay K. Anesthesia and obesity and gastrointestinal disorders. In: Barash PG, Cullen BF, Stoelting RK. Clinical Anesthesia.4th ed. Philadelphia: Lippincott Williams &Wikins 2001: 1035-1104.
- Fell D. The practical conduct of anesthesia. In: Aitkenhead AR, Rowbotham DJ, Smith G. Textbook of anesthesia. 4th ed. Edinburgh: Churchill Livingstone 2001: 464.
- Nahmias JS, Karetzky MS. Treatment of the obstructive sleepapnea syndrome using a nasopharyngeal tube. Chest 1988; 94: 1142-1147.
- Huo H, Li WY, Shen P, Liu JH. One night treatment of obstructive sleepapnea and hypopnea syndrome with nasopharyngeal airway. ZhonghuaEr Bi Yan HouTou Jing WaiKeZaZhi 2010; 45: 382-386.
- Jenkins K, Wang DT, Correa R. Management choices for the difficult airway by anesthesiologists in Canada. Can J Anesth 2002; 49: 850-856.
- Shakib K, Heliotis M, Gillhooly M. The nasopharyngeal airway: reliable and effective tool for marsupialisation. Br J Oral MaxillofacSurg 2010; 48: 386-387.
- Yeh SJ, Huang KY, Wang TG, Chen YC, Chen CH, Tang SC, Tsai LK, Yip PK, Jeng JS. Dysphagia screening decreases pneumonia in acute stroke patients admitted to the stroke intensive care unit. J NeurolSci 2011; 306: 38-41.
- Westendorp WF, Nederkoorn PJ, Vermeij JD, Dijkgraaf MG, van de Beek D. Post-stroke infection: a systematic review and meta-analysis. BMC Neurol 2011; 11: 110.