Research Article - Journal of Primary Care and General Practice (2018) Volume 1, Issue 2
Comparison of the 2013 ACC/AHA guidelines, 2016 USPSTF recommendations and ATP III guidelines for the management of dyslipidaemia in a Macau SAR cohort.
In Wong*Sao Lourence Health Center, Health Bureau of Macau SAR, China
- *Corresponding Author:
- In Wong
Sao Lourence Health Centre, Health Bureau of Macau SAR, China
Tel: 00853-66861967
E-mail: michelle.wongin@gmail.com
Accepted on September 14, 2018
Abstract
Objective: Atherosclerotic cardiovascular disease is a major cause of death, and there are many published guidelines for the management of blood cholesterol. This study compared differences in the implementation of the National Cholesterol Education Program Adult Treatment Panel III (ATP III) guidelines, the 2013 American College of Cardiology and the American Heart Association (ACC/AHA) guidelines and the U.S. Preventive Services Task Force (USPSTF) 2016 recommendations for the management of dyslipidaemia in the Macau SAR population. Methods: In total, 896 patients fulfilled the inclusion criteria. Risk estimation was based on the patient lipid profiles and risk factors prior to initiating statins. The proportions of the study population who qualified for statin treatment under the above three guidelines were determined. Results: The comparison of the ATP III guidelines with the 2013 ACC/AHA guidelines showed that 154 (17.2%) additional patients were eligible for statins. The comparison of the USPSTF 2016 recommendations with the 2013 ACC/AHA guidelines revealed that the former resulted in 150 (16.7%) additional patients who were eligible for statins. When compared with the 2013 ACC/AHA guidelines and the USPSTF 2016 recommendations, the ATP III guidelines are more likely to recommend treatment for younger individuals, females, and those with higher total cholesterol and LDL-C. Conclusion: Application of various guidelines led to different populations who were eligible for statins. The 2013 ACC/AHA guidelines for lipid-lowering medications resulted in a significant increase in the population eligible for statins
Keywords
statins, cholesterol, ATP III, ACC/AHA, USPSTF.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is a major global cause of death [1,2] and the second leading cause of death in Macau SAR [3]. However, the prevention of this disorder remains suboptimal. Lifestyle and risk factor modification and pharmacological interventions are essential for reducing cardiovascular events. Statins play a key role in both primary and secondary prevention [4,5]. The American College of Cardiology and the American Heart Association (ACC/AHA) published new guidelines for the management of blood cholesterol in November 2013 [6] to replace the National Cholesterol Education Program Adult Treatment Panel III (ATP III) guidelines published over a decade ago [7]. The U.S. Preventive Services Task Force (USPSTF) also updated their recommendations in 2016 to influence clinical practice [8].
Risk prediction models should have good discriminatory power to be clinically meaningful. Numerous algorithms use combinations of conventional risk factors to identify individuals who are at a higher risk of cardiovascular disease (CVD) and most likely to benefit from preventive measures. These guidelines use varying approaches for the CVD risk estimation and implement different criteria for therapeutic recommendations. The ATP III guidelines use the 10-year coronary heart disease (CHD) risk estimated by the Framingham risk score (FRS) [9] and both the 2013 ACC/AHA guidelines and the USPSTF 2016 recommendations advocate the use of Pooled Cohort Equations to estimate the ASCVD risk [6,8].
The ATP III guidelines consider four classes of cardiovascular risk and recommend for the low-density lipoprotein cholesterol (LDL-C) levels to be maintained below 100 mg/dl (2.6 mmol/L) in high-risk patients, below 130 mg/dl (3.4 mmol/L) in moderate-risk patients and below 160 mg/dl (4.2 mmol/L) in low-risk patients Statin therapy should be recommended if the patient’s LDL-C is over the treatment target [7]. The 2013 ACC/ AHA guidelines abandon the previous paradigm of treating according to specific LDL-C targets. Instead, the new guidelines recommend statin therapy for patient groups for whom statin reduced the risk of ASCVD, including CHD and stroke, in randomized controlled trials. The 2013 ACC/AHA guidelines identify the following four patient groups as candidates for statin therapy: 1) patients with clinical ASCVD (acute coronary syndrome, myocardial infarction, stable angina, coronary or other arterial revascularization, stroke, transient ischaemic attack, and peripheral arterial disease of an atherosclerotic origin), 2) patients with LDL-C levels of 190 mg/dl (4.9 mmol/L) or more, 3) patients aged 40 to 75 years with diabetes and LDL-C levels of 70 to 189 mg/dl (1.8 to 4.9 mmol/L), and 4) patients aged 40 to 75 years without diabetes with LDL-C levels of 70 to 189 mg/dl (1.8 to 4.9 mmol/L) and a predicted 10-year ASCVD risk of 7.5% or more, as calculated by the new Pooled Cohort Equations published along with the guidelines [6]. In 2016, the USPSTF updated their recommendations for the primary prevention of CVD to include that adults without a history of CVD (i.e., symptomatic coronary artery disease or ischaemic stroke) should use a low- to moderate-dose statin for the prevention of CVD events and mortality if all the following criteria are met: 1. patients aged 40 to 75 years, 2. patients have 1 or more CVD risk factors (i.e., dyslipidaemia, diabetes, hypertension, or smoking), and 3. patients have a 10% or greater calculated 10-year risk of a cardiovascular event [8].
Following the publication of the new guidelines, many have criticized the new recommendations particularly because the new Pooled Cohort Equations may have poor calibration and lead to the overestimation of risk [10-14]. This potential overestimation, combined with the lower threshold for treatment, may lead to a significant increase in the population of individuals for whom statins could be recommended for primary prevention [15].
Different approaches to statin treatment translate into substantial differences in the population qualifying for treatment and the economic and health system burden. This study compared the differences among the ATP III guidelines, the 2013 ACC/ AHA guidelines and the USPSTF recommendations for the management of dyslipidaemia in the Macau SAR population.
Methods
This study was conducted using computerized clinical records from Sao Lourence Health Center, which is one of the eight health centers of the Macau Health Bureau, between 1 September 2017 and 31 December 2017. In total, 1200 patient records were systematically reviewed. The patient demographics, risk factors, physical measures, lipid profiles and concomitant medications were obtained by reviewing the medical records. Finally, 896 patients fulfilled the inclusion criteria.
The inclusion criteria were as follows: 1. patients aged ≥ 21 but ≤ 75 years regardless of gender with, 2. a lipid profile record before the initiation of statin therapy, or 3. at least one lipid profile record within 3 years if the patient was not currently treated with a statin. All the selected cases fulfilled the three criteria above.
As recommended by the ACC/AHA and USPSTF, we used sexspecific Pooled Cohort Equations for each participant, and for the ATP III guidelines, we calculated the FRS using previously published equations modified as recommended by the ATP III [7]. The risk estimation was based on the patients’ lipid profiles and risk factors prior to initiating statins. Subsequently, we determined the proportions of the study population who qualified for statin treatment under the ATP III guidelines, the 2013 ACC/AHA guidelines and the USPSTF recommendations.
Statistical analysis
The continuous variables are expressed as the means ± SDs, and the categorical variables are expressed as proportions. Continuous variables in two groups were compared using independent t-tests, and categorical variables in different groups were compared using Chi-square tests. As applicable, P<0.05 was considered statistically significant. The percentages were calculated on the basis of the total responses.
All the statistical analyses were carried out using SPSS version 24 (IBM Corp., Armonk, New York).
Results
Overall patient cohort
In total, 896 patients were included in this study. The general characteristics of the cohort are summarized by sex in Table 1. The mean (± SD) age was 58.0 ± 10.1 years, and 44.4% of the patients were male. Hypertension was identified in 47.8% of the patients, and 10.5% of the patients were current smokers. Onefifth (21.5%) of the patients had diabetes, 10% suffered from low high-density lipoprotein cholesterol (HDL) (40 mg/dl or 1.03 mmol/L), and 1.6% reported having a family history of premature CHD.
| Characteristic | Overall (n=896) |
Male (n=398) |
Female (n=498) |
P-value |
|---|---|---|---|---|
| Age, years | 58 ± 10.1 | 58.5 ± 10.6 | 57.6 ± 9.6 | 0.158 |
| Current cigarette smoking, % | 10.5 | 19.3 | 3.4 | <0.0001 |
| Hypertension, %* | 47.8 | 53 | 43.6 | 0.005 |
| DM, % | 21.5 | 26.6 | 20.5 | 0.001 |
Table 1: General characteristics of the cohort by sex.
Among the entire study population, 394 (44%), 544 (60.2%) and 390 (43.5%) patients qualified for lipid-lowering therapy based on the ATP III guidelines, the 2013 ACC/AHA guidelines and the USPSTF 2016 recommendations, respectively. In total, 89.5% of the 390 patients who qualified for lipid-lowering treatment by the ATP III guidelines and 100% of the 394 patients who qualified for statin therapy by the USPSTF recommendations also qualified under the ACC/AHA recommendations.
The most frequently dispensed regimen (for either primary or secondary prevention) was simvastatin at 80.3% (mean dose ± SD, 18.87 ± 5.95 mg), followed by atorvastatin at 12.3% (mean dose ± SD, 20.43 ± 7.79 mg) and rosuvastatin at 7.2% (mean dose ± SD, 9.37 ± 3.87 mg).
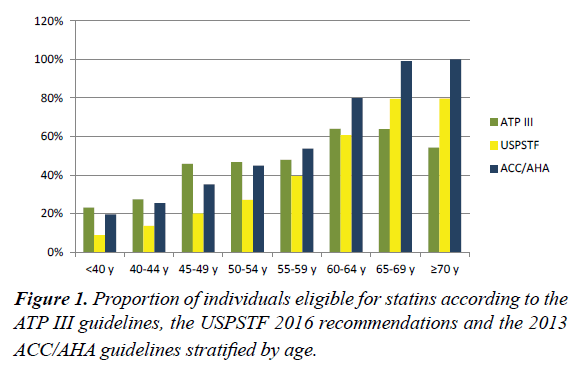
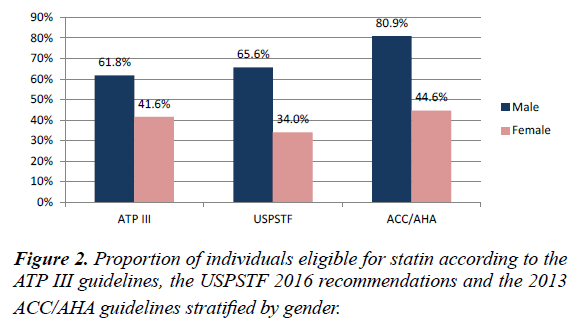
ATP III vs ACC/AHA
Most newly eligible people were aged 55 to 75 years and were male (Figures 1 and 2), and the main eligibility criterion is a predicted 10-year ASCVD risk of 7.5% or more. Among the patients currently treated with statins, many patients were not receiving a statin with the appropriate intensity recommended by the 2013 ACC/AHA guidelines. In our sample, only 1.9% of the patients on statins aged 75 years or younger were receiving a high-intensity regimen as recommended by the guidelines. Moreover, 16.8% of the patients on statins were receiving lowintensity regimens, which are not recommended by the 2013 ACC/AHA guidelines. We examined the LDL-C levels in the patients newly eligible for statins to determine the proportion of patients with LDL-C levels below the cut-off for which treatment is recommended by the ATP III guidelines. In the patients newly eligible for statin treatment for secondary prevention, the mean LDL-C level was 91.33 ± 34.44 mg/dl (2.36 ± 0.89 mmol/L), and 44.4% of the patients had an LDL-C level lower than the 100 mg/dl (2.6 mmol/L) target recommended by the ATP III guidelines for secondary prevention [7]. In the diabetic patients newly eligible for statin treatment for primary prevention, the mean LDL-C level was 83.98 ± 16.25 mg/dl (2.17 ± 0.42 mmol/L), and 88.9% of the patients had an LDL-C level lower than the 100 mg/dl (2.6 mmol/L) target recommended by the ATP III guidelines for primary prevention in diabetic patients [7]. In the non-diabetic patients newly eligible for statin treatment for primary prevention, the mean LDL-C level was 109.52 ± 16.25 mg/dl (2.83 ± 0.42 mmol/L), and 100% of the patients’ LDL-C levels were lower than the 130 mg/dl (3.4 mmol/L) target recommended by the ATP III guidelines for primary prevention among patients in the intermediaterisk category (2 or more risk factors and a 10-year risk<20%). However, this change in the population eligible for statin was highly dependent on age and sex. Although applying the recommendations of the new guidelines resulted in fewer individuals eligible for statin therapy until approximately age 55 using the 7.5% cut-off, the difference in the proportion of individuals eligible for statins steadily increased among the older individuals, and most participants qualifying by the age of 60 years according to the 2013 ACC/AHA guidelines (Figure 1). Additionally, applying the 2013 ACC/AHA guidelines resulted in a large increase in the number of males eligible for statins, whereas the changes among the females were largely dependent on the risk cut-off used. This difference between the sexes was mainly driven by the larger discrepancy in the risk estimation between the FRS and ASCVD risk scores in women than that in men. Compared with the population for whom the guidelines were concordant that statins should not be used, the population for whom both guidelines were concordant regarding eligibility for statin therapy was older and had more risk factors and higher risk scores on both the FRS and ASCVD. Comparing the discordant samples, the current ATP III guidelines are more likely to recommend treatment for younger individuals; females; individuals with a higher total cholesterol and LDL-C, lower HDL and higher triglycerides; individuals who are less likely to have hypertension or be a current smoker; and individuals with lower FRS and ASCVD scores (Table 2).
| Concordant recommendations | Discordant recommendations | |||
|---|---|---|---|---|
| Both recommend statin, n=349 | Both do not recommend statin, n=311 | ATP III recommends statin, but ACC/AHA does not, n=41 | ACC/AHA recommends statin, but ATP III does not, n=195 | |
| Male sex (%) | 202(57.9) | 67(21.5) | 9(22) | 120(61.5) |
| Age, years | 62.12±8.01 | 50.47±9.15 | 55.12±8.55 | 63.23±7.3 |
| Lipids | ||||
| TC*, mg/dl (mmol/L) | 246.91±146.29 (6.38±3.78) |
202.4±34.44 (5.23±0.89) |
240.33±32.51 (6.21±0.84) |
198.14±38.7 (5.12±1.00) |
| HDL*, mg/dl (mmol/L) | 53.02±13.55 (1.37±0.35) |
66.95±17.8 (1.73±0.46) |
55.34±18.19 (1.43±0.47) |
62.31±20.51 (1.61±0.53) |
| LDL-C*, mg/dl (mmol/L) | 150.93±38.7 (3.9±1.0) |
116.87±38.31 (3.02±0.99) |
149.38±32.12 (3.86±0.83) |
111.07±31.35 (2.87±0.81) |
| TG*, mg/dl (mmol/L) | 85.53±104.1 (2.21±2.69) |
43.73±21.67 (1.13±0.56) |
88.62±73.92 (2.29±1.91) |
54.95±57.28 (1.42±1.48) |
| Hypertension, (%) | 233(66.8) | 81(26) | 26(63.4) | 88(45.1) |
| DM, (%) | 155 (44.4) | 1(0.3) | 2 (4.9) | 35 (17.9) |
| Smoking, (%) | 69(19.8) | 9(2.9) | 0(0) | 16(8.2) |
| FRS 10-year risk | 25.46±13.96 | 6.24±3.26 | 10.46±6.13 | 17.23±9.08 |
| ASCVD 10-year risk | 14.93±9.4 | 2.29±1.38 | 3.74±3.81 | 12.2±7.28 |
*TC total=total cholesterol; HDL=high-density lipoprotein; LDL-C=low-density lipoprotein cholesterol; TG=triglycerides; FRS=Framingham risk scores; ASCVD=atherosclerotic cardiovascular disease
Table 2: Agreement in statin indication between the ATP III guidelines and the 2013 ACC/AHA guidelines.
ATP III vs USPSTF
Compared with the patients who were eligible for statin therapy based on the ATP III guidelines, most newly eligible people were aged 65 to 75 years and men (Figure 2). Among the patients currently treated with statins, many patients were receiving a statin with the appropriate intensity recommended by the USPSTF recommendations.
We examined the results of the LDL-C tests in the patients newly eligible for statins to determine the proportion of patients with LDL-C levels below the cut-off at which treatment is recommended by the ATP III guidelines. No diabetic patients were newly eligible for statin treatment for primary prevention. In total, 11 (1.2%) non-diabetic patients were newly eligible for statin treatment for primary prevention, the mean LDL-C level was 106.43 ± 18.96 mg/dl (2.75 ± 0.49 mmol/L), and 100% of the patients’ LDL-C levels were lower than the 130 mg/dl (3.4 mmol/L) target recommended by the ATP III guidelines for primary prevention in patients in the intermediate-risk category (2 or more risk factors and a 10- year risk<20%). Although applying the recommendations from the new guidelines resulted in fewer individuals eligible for statin therapy until approximately age 65 using the 10% cutoff, the difference in the proportion of individuals eligible for statins steadily increased among the older individuals, and most participants qualified by the age of 65 years according to the USPSTF recommendations (Figure 1). Similar to the results of the comparisons between the ATP III guidelines and the 2013 ACC/AHA guidelines, the population for whom both guidelines were concordant regarding the eligibility for statin therapy was older and had more risk factors and a higher risk score on both the FRS and ASCVD than those for whom the guidelines were concordant that statins should not be used (Table 3). Comparing the discordant samples, the current ATP III guidelines are more likely to recommend treatment for younger individuals; females; individuals with a higher total cholesterol and LDL-C, lower HDL, and higher triglycerides; individuals who are less likely to be a current smoker; and individuals who have lower FRS and ASCVD scores (Table 3).
| Concordant recommendations | Discordant recommendations | |||
|---|---|---|---|---|
| Both recommend statin, n=279 | Both do not recommend statin, n=389 | ATP III recommends statin, but USPSTF does not, n=112 | USPSTF recommends statin, but ATP III does not, n=116 | |
| Male sex (%) | 183(65.5) | 108(27.8) | 29(25.9) | 78(67.2) |
| Age, years | 63.43±7.26 | 52.78±9.97 | 56.29±8.69 | 64.05±7.12 |
| Lipids | ||||
| TC*, mg/dl (mmol/L) | 250.39±162.93 (6.47±4.21) |
201.63±34.83 (5.21±0.9) |
236.07±31.35 (6.1±0.81) |
197.37±97.91 (5.1±2.53) |
| HDL*, mg/dl (mmol/L) | 52.25±13.93 (1.35±0.36) |
65.79±18.19 (1.7±0.47) |
54.95±15.09 (1.42±0.39) |
62.69±21.29 (1.62±0.55) |
| LDL-C*, mg/dl (mmol/L) | 152.87±40.25 (3.95±1.04) |
116.10±36.77 (3.0±0.95) |
146.29±30.96 (3.78±0.8) |
109.52±31.35 (2.83±0.81) |
| TG*, mg/dl (mmol/L) | 87.46±113.00 (2.26±2.92) |
46.83±42.96 (1.21±1.11) |
81.66±63.47 (2.11±1.64) |
51.86±27.48 (1.34±0.71) |
| Hypertension, (%) | 199(71.6) | 106(27.2) | 60(53.6) | 63(54.3) |
| DM, (%) | 113 | 9 | 44 | 27 |
| Smoking, (%) | 66(23.7) | 11(2.8) | 3(2.7) | 14(12.1) |
| FRS 10-year risk | 28.19±14.03 | 7.62±4.43 | 12.95±6.48 | 19.97±10.48 |
| ASCVD 10-year risk | 17.09±9.06 | 3.75±3.78 | 5.2±4.05 | 14.5±7.76 |
*TC total=total cholesterol; HDL=high-density lipoprotein; LDL-C=low-density lipoprotein cholesterol; TG=triglycerides; FRS=Framingham risk scores; ASCVD=atherosclerotic cardiovascular disease
Table 3: Agreement in statin indication between the ATP III guidelines and the USPSTF 2016 recommendations.
ACC/AHA vs. USPSTF
Comparing the USPSTF 2016 recommendations with the 2013 ACC/AHA guidelines, all patients eligible for statins based on the USPSTF 2016 recommendations were eligible based on the 2013 ACC/AHA guidelines, but according to the 2013 ACC/ AHA guidelines, 150 (16.7%) additional patients were eligible for statins. The comparison results between the 2013 ACC/ AHA guidelines and the USPSTF 2016 recommendations are shown in Table 4.
| Concordant recommendations | Discordant recommendations | ||
|---|---|---|---|
| Both recommend statin, n=344 | Both do not recommend statin, n=387 | ACC/AHA recommends statin, but USPSTF does not, n=165 | |
| Male sex (%) | 74(21.5) | 259(66.9) | 65(39.4) |
| Age, years | 63.8±7.05 | 50.93±0.94 | 59.1±8.64 |
| Lipids | |||
| TC*, mg/dl (mmol/L) | 234.91±141.64 (6.07±3.66) |
206.66±36.38 (5.34±0.94) |
215.56±27.09 (5.57±0.7) |
| HDL*, mg/dl (mmol/L) | 54.95±16.64 (1.42±0.43) |
65.79±18.19 (1.7±0.47) |
59.21±17.80 (1.53±0.46) |
| LDL-C*, mg/dl (mmol/L) | 140.48±42.96 (3.63±1.11) |
120.36±39.09 (3.11±1.01) |
127.32±34.83 (3.29±0.9) |
| TG*, mg/dl (mmol/L) | 77.4±98.30 (2.00±2.54) |
48.76±35.22 (1.26±0.91) |
66.56±70.43 (1.72±1.82) |
| Hypertension, (%) | 221(64.2) | 105(30.5) | 102(38.2) |
| DM, (%) | 139 (40.4) | 2 (0.5) | 52 (31.5) |
| Smoking, (%) | 78(20.7) | 7(1.8) | 9(5.5) |
| ASCVD 10-year risk | 16.46±8.69 | 2.35±1.24 | 7.56±5.09 |
*TC total=total cholesterol; HDL=high-density lipoprotein; LDL-C=low-density lipoprotein cholesterol; TG=triglycerides; FRS=Framingham risk scores; ASCVD=atherosclerotic cardiovascular disease
Table 4: Agreement in statin indication between the 2013 ACC/AHA guidelines and the USPSTF 2016 recommendations.
Discussion
In this study, compared with the ATP III guidelines and the USPSTF 2016 recommendations, the 2013 ACC/AHA guidelines increased the number of individuals requiring statin treatment for the prevention of CVD. This pronounced increase in the population eligible for statin therapy has previously been demonstrated in both a US study and a European study [15,16].
For the prevention of cardiovascular diseases in high-risk populations, determining the 10-year CVD risk is essential and can help identify high-CVD-risk individuals without underestimating or overestimating the risk. Different risk prediction systems for the identification of patients at risk have been used in primary prevention. The most commonly used scoring systems include the risk scoring tools of the ACC/ AHA guidelines, the ATP III and the European Society of Cardiology (ESC) guideline SCORE risk system. For primary CVD prevention, based on the evidence from clinical trials investigating statin drugs, the new ACC/AHA guidelines modified clinical decision making and proposed recommending statin treatment solely based on a 10-year ASCVD risk greater than 7.5% [6]. This distinction from previous guidelines in the United States and the current ESC guidelines represents a fairly straightforward approach that deviates from the risk functions of the 10-year hard CHD or CVD mortality combined with blood concentrations of LDL-C [7,16,17].
The usability of a risk prediction system depends on a combination of its calibration and discrimination. The proper calibration of a risk prediction system is crucial in decision making regarding whether treatment is to be initiated. An inaccurate risk prediction system may not only fail to correctly identify the patients who are truly at risk but also lead to possible drug complications and unnecessary costs due to improper patient selection.
The Framingham risk score used for CV risk calculations tends to overestimate the CV risk by approximately 5% in UK men [18]. The ASCVD risk score tends to underestimate the 10-year and lifetime risk in persons from certain race/ethnic groups, especially American Indians, certain Asian Americans (e.g., South Asian ancestry), and certain Hispanics (e.g., Puerto Ricans), and may overestimate the risk in other groups, including certain Asian Americans (e.g., East Asian ancestry) and certain Hispanics (e.g., Mexican Americans) [6].
Both a large European cohort study and a large multi-ethnic American study reported that the new risk-stratification strategy overestimates the true event rate, but the overestimation may be more substantial in European populations [12,16,19]. Because the true benefit of statins is closely associated with the absolute risk of events, the overestimation may lead to treating some individuals who may not derive a net benefit from treatment, although they might be exposed to significant side effects and costs. Notably, however, overestimation is not exclusive to the new guidelines, and similar findings have been recently reported for virtually all currently recommended risk scores [12].
This study had several limitations. First, 99% of the study population is of Asian ancestry. Therefore, our findings should be cautiously extrapolated to other ethnicities. Second, only one health center in Macau SAR participated in the study. Selection bias cannot be excluded because the participating patients were older than the patients in the other health centers in Macau SAR. Therefore, these results may not be fully representative of the broader primary care population in Macau SAR. Finally, the current analysis did not evaluate the appropriateness or costeffectiveness of these strategies. We only provided an estimate of the magnitude of the potential impact.
Conclusion
Application of different guidelines led to different populations who were eligible for statins. The 2013 ACC/AHA guidelines for lipid-lowering medications resulted in a significant increase in the population eligible for statins. The populations eligible for statins using the USPSTF 2016 recommendations or ATP III guidelines were similar, but the ATP III guidelines were more likely to recommend treatment for younger individuals, females, and individuals with higher total cholesterol and LDL-C. Additional survival and cost-effectiveness analyses are needed to define the appropriateness of these three guidelines and determine the appropriate recommendations for the Macau SAR population.
Acknowledgement
I acknowledge the support provided by the director of the Sao Lourence Health Center and the GPs who participated in my research study.
Disclosure Statement
The authors declare that they have no conflict of interest.
References
- Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation. 2014; 129:399-410.
- Nichols M, Townsend N, Scarborough P, et al. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014; 35:2950-9.
- de Saúde S, da Região G. Administrativa especial de macau. Boletim estatístico. 2016.
- Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian simvastatin survival study. Lancet 1994; 344:1383-9.
- Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013.
- Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol 2014; 63:2889-934.
- National Institutes of Health, National Heart, Lung, and Blood Institute, National Cholesterol Education Program. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel III) final report. Circulation. 2002; 106:3143-421.
- Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Statin use for the primary prevention of cardiovascular disease in adults: US preventive services task force recommendation statement. Jama. 2016; 316:1997-2007.
- D'Agostino RB Sr., Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 2008; 117:743-53.
- Cook NR, Ridker PM. Response to comment on the reports of over-estimation of ASCVD risk using the 2013 AHA/ACC risk equation. Circulation 2014; 129:268-9.
- Yeboah J, Sillau S, Delaney JC, et al. Implications of the new American College of Cardiology/American Heart Association cholesterol guidelines for primary atherosclerotic cardiovascular disease event prevention in a multi ethnic cohort: multi-ethnic study of atherosclerosis (MESA). Am Heart J 2015; 169:387-95.
- DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med 2015; 162:266-75.
- Amin NP, Martin SS, Blaha MJ, et al. Headed in the right direction but at risk for miscalculation: a critical appraisal of the 2013 ACC/AHA risk assessment guidelines. J Am Coll Cardiol 2014; 63:2789-94.
- Toth PP, Thanassoulis G, Williams K, et al. The risk-benefit paradigm vs the causal exposure paradigm: LDL as a primary cause of vascular disease. J Clin Lipidol 2014; 8:594-605.
- Pencina MJ, Navar-Boggan AM, D'Agostino RB, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med 2014; 370:1422-31.
- Kavousi M, Leening MJ, Nanchen D, et al. Comparison of application of the ACC/AHA guidelines, adult treatment panel III guidelines, and European society of cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA 2014; 311:1416-23.
- Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 2016; 37:2999-3058.
- Tillin T, Hughes AD, Whincup P, et al. Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a U.K. tri-ethnic prospective cohort study (SABRE-Southall and Brent REvisited). Heart 2014; 100:60-7.
- Ton VK, Martin SS, Blumenthal RS, et al. Comparing the new European cardiovascular disease prevention guideline with prior American Heart Association guidelines: an editorial review. Clin Cardiol 2013; 36:E1-6.