Case Report - Journal of Gastroenterology and Digestive Diseases (2018) Volume 3, Issue 2
Comparison of outcomes of two methods of surgery (J-pouch and ileorectal anastomosis) in children with total colonic aganglionosis, Hirschsprung?s disease
Ashjaei Bahar* and Nahvi Hedayatollal
Department of Pediatric Surgery, Tehran University of Medical Sciences, Iran
- *Corresponding Author:
- Ashjaei Bahar
Department of Pediatric Surgery
Tehran University of Medical Sciences, Iran
Tel: +989123805401; +989213805401
E-mail: Ashjaei@tums.ac.ir
Accepted on March 26, 2018
Citation: Bahar A, Hedayatollal N. Comparison of outcomes of two methods of surgery (J-pouch and ileorectal anastomosis) in children with total colonic aganglionosis, Hirschsprung’s disease. J Gastroenterol Dig Dis. 2018;3(2):34-37.
Abstract
Background and objectives: Hirschsprung disease is commonly diagnosed in early childhood by aganglion areas in rectal biopsy. Diagnosed infants usually undergo a primary procedure and the definitive surgical treatment is usually performed several months later. Different surgical methods have been proposed for its treatment, but the detailed outcome of each method should be further investigated. Thus, we aimed to retrospectively assess the outcomes between two surgical methods for consistency of intestinal continuity, including J-Pouch and ileorectal anastomosis, in total colectomy procedure, in patients with total colon aganglionosis in our center.
Materials and methods: In this study, we retrospectively assessed all children undergoing total colectomy after primary ileostomy in Children’s Medical Center Hospital, from 1994 to 2016. In this center, intestinal continuity was provided by J-pouch procedure from 1994 to 2003, and by ileorectal anastomosis from 2003 to 2016. In the second method, 0.2 mg/kg loperamide was started after the first surgery (ileostomy) and was increased until the skin around ileostomy was just like the intact skin around colostomy with no significant inflammation. Data including demographic characteristics, need for re-ileostomy, duration of hospitalization, duration of NPO after surgery, and amount of loperamide were recorded, and compared between the two groups. Postoperative short-term complications were also recorded and compared. During the three-year follow-up period, all patients were assessed for soiling and fecal continence.
Results: Among 37 patients undergoing total colectomy due to total colon aganglionosis, 48.6% underwent J-pouch procedure (group 1) and 51.4% ileorectal anastomosis (group 2). In general, 54.1% were female and 45.9% were male. Mean hospitalization time was significantly lower in the second group (P=0.000). Mean NPO time was 7.06 ± 2.55 days in the first group and 3.63 ± 0.49 days in the second group (P=0.000). The rate of enterocolitis and mean surgical duration were significantly higher in the first group (P=0.001, and 0.000). None of the patients reported any fecal incontinence or constipation after surgery in both groups. Other postoperative complications had no statistically difference regarding leak, peri-anal inflammation, number of defecations, soiling, anastomosis stricture, need for re-ileostomy, pelvic abscess, peritonitis, and adhesion band.
Conclusion: As the results of the present study indicated, the surgical method of ileorectal anastomosis has significant advantages to J-pouch procedure, including less hospitalization time, surgical duration and NPO duration, no cases of enterocolitis, fecal incontinence or constipation, which, in general, indicates that ileorectal anastomosis is a better method than J-pouch.
Keywords
Hirschsprung disease, Surgical procedures, Operative procedures.
Introduction
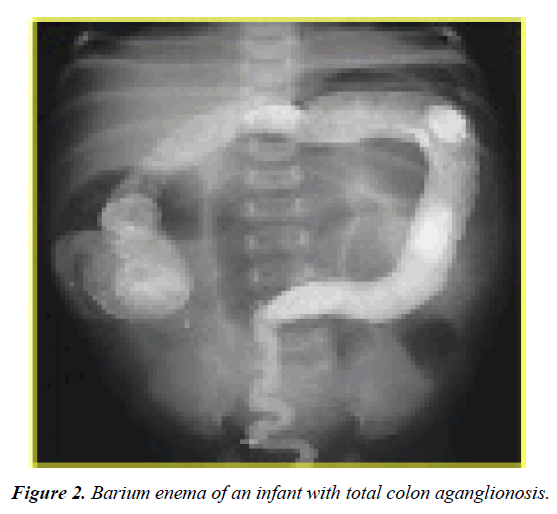
Hirschsprung disease, also known as aganglion megacolon, is a congenital disorder affecting around 1/5000 live births with a male -female ratio of 3:1 [1]. It is mostly diagnosed by rectal biopsies, which indicates absent ganglion cells in submucosal and myenteric plexuses [2]. Moreover, several other diagnostic approaches have been proposed for its diagnosis, including imaging techniques, barium enema, manometry, and different biopsy approaches [3]. The common symptoms include constipation, abdominal distension, vomiting, failure to thrive (FTT) and neonatal enterocolitis [4].
The treatment is dominantly surgical, but infants may undergo a primary surgery before definitive surgery. Various surgical methods have been proposed, such as Swenson, Soave and Duhamel procedures, laparoscopic and transanal pull-through techniques, etc. [4]. Early and late postoperative complications include enterocolitis, incontinence, fecal fistula, wound infection and dehiscence, obstruction, recurrence and mortality [5-7], which varies among different procedures [1,8,9]. Laparoscopic-assisted surgery was found to be associated with less blood loss, hospitalization, and first bowel movement [10]. Yet, the long-term outcomes of each surgical procedure should be precisely determined in order to define the gold standard treatment.
Thus, we aimed to retrospectively assess the outcomes between two surgical methods for consistency of intestinal continuity, including J-Pouch and ileorectal anastomosis, in total colectomy, in patients with total colon aganglionosis, in our center.
Materials and Methods
Study design
In this study, we retrospectively assessed all children undergoing total colectomy due to total colon aganglionosis, in Children’s Medical Center Hospital, from 1994 to 2016. Diagnosis of the disease was made by contrast enema and biopsy, then all patients underwent a primary ileostomy and after several months, when the child could tolerate a gross surgery, they underwent total colectomy. In this center, intestinal continuity during this procedure was provided by J-pouch procedure from 1994 to 2003, and by ileorectal anastomosis from 2003 to 2016. The classic J-pouch procedure was performed through the first group and in the second method; ileum was directly attached above dentate line by direct anastomosis. In order to reduce the number of defecations, increase the absorption time, and reduce inflammation, 0.2 mg/kg loperamide was started after the first surgery (ileostomy) and the dose was increased until the skin around ileostomy was just like the intact skin around colostomy with no significant inflammation.
All children with established Hirschsprung disease, who underwent total colectomy due to total colon aganglionosis, were enrolled into the study and patients who had other accompanying diseases, such as syndromic patients were excluded from the study. In addition, any patient with involvement of ileum or proximal parts of the intestine was not included in the study.
Data including gender, age at ileostomy and at definitive surgery, type and duration of the definitive surgery, need for re-ileostomy, duration of hospitalization, duration of NPO after surgery, and amount of loperamide were recorded, and then compared between groups. Postoperative short-term complications were recorded as well, including anastomosis leak and stricture, peri-anal inflammation, pelvic abscess, peritonitis, constipation, enterocolitis, adhesive bands, and long-term complications, included soiling, manometric results, and fecal incontinence.
Statistical analysis
Continuous variables are presented as mean ± standard deviation and qualitative variables are reported as frequencies (percentage). Comparison of variables between the two groups was performed by chi-square and one-way ANOVA tests. Statistical analysis was performed using SPSS 20.0 software (SPSS Inc., Chicago, IL, USA). P-values less than 0.05 were considered statistically significant in all tests.
Results
A total of 37 patients underwent total colectomy during the study period, among which 48.6% underwent J-pouch procedure (Group 1) and 51.4% underwent ileorectal anastomosis (Group 2). In general, 54.1% were female and 45.9% were male patients. The sex distribution of patients was not significantly different between the two groups (p=0.56). Mean age of patients at ileostomy was 19.83 ± 29.14 months in the first group and 21.74 ± 47.76 months in the second group (P=0.885). Mean age of patients at definitive surgery was 13.17 ± 3.2 months in the first group and 17.47 ± 3.7 months in the second group (P=0.001).
Mean hospitalization time was significantly lower in the second group compared with the first group (4.95 ± 0.7 vs. 9.11 ± 3.37 days, P=0.000). Besides, mean NPO time was remarkably lower in the second group as well (3.63 ± 0.49 vs. 7.06 ± 2.55 days, P=0.000). Mean amount of loperamide, which was only administered in the second group, was 2.68 ± 0.885 mg.
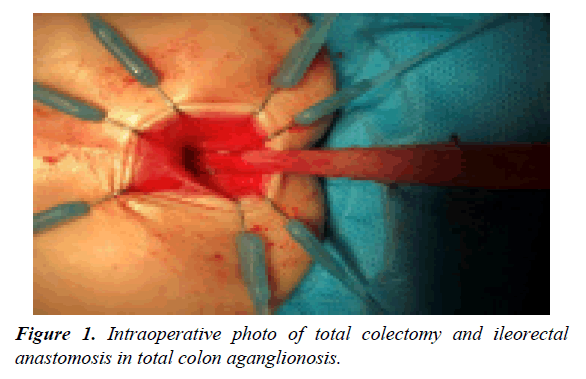
Postoperative complications are summarized in Table 1, which indicates no statistically difference regarding leak, peri-anal inflammation, number of defecations, soiling, anastomosis stricture, need for re-ileostomy, pelvic abscess, peritonitis, and adhesion band. Surprisingly, although 8 patients in the first group experienced enterocolitis, no case of enterocolitis was recorded in the second group which was statistically significant (P=0.001) Mean surgical duration was 227.78 ± 26.69 minutes in the first group and 88.42 ± 13.54 minutes in the second group (P=0.000) (Figures 1 and 2).
| Variables | Group 1 | Group 2 | P-value | |
|---|---|---|---|---|
| Leak | Positive | 3 | 0 | 0.105 |
| Negative | 15 | 19 | ||
| peri-anal inflammation | Positive | 1 | 4 | 0.187 |
| Negative | 17 | 15 | ||
| Number of defecations | Once | 4 | 3 | 0.382 |
| Twice | 4 | 7 | ||
| Three times | 2 | 8 | ||
| Four times | 0 | 1 | ||
| Soiling | Positive | 1 | 2 | 0.521 |
| Negative | 17 | 17 | ||
| Anastomosis stricture | Positive | 5 | 4 | 0.462 |
| Negative | 13 | 15 | ||
| Need for re- ileostomy | Positive | 2 | 0 | 0.23 |
| Negative | 16 | 19 | ||
| Pelvic abscess | Positive | 2 | 0 | 0.23 |
| Negative | 16 | 19 | ||
| Peritonitis | Positive | 1 | 0 | 0.48 |
| Negative | 17 | 19 | ||
| Enterocolitis | Positive | 8 | 0 | 0.001 |
| Negative | 10 | 19 | ||
| Adhesion band | Positive | 1 | 0 | 0.48 |
| Negative | 17 | 19 |
Table 1. Comparison of post-operative complications between two groups.
None of the patients in both groups reported any fecal incontinence or constipation after surgery.
Discussion
As the results of the present study indicated, the surgical methods of ileorectal anastomosis (group 2) had some priorities to J-pouch procedure (group 1), including less hospitalization time, NPO duration and surgical duration (P=0.000), and lower rate of enterocolitis and (P=0.001). None of the patients in both groups reported any fecal incontinence or constipation after surgery and the rest of complications was not statistically different between the groups.
Importantly, the proposed ileorectal anastomosis procedure is associated with higher patients’ comfort as the result of lower hospitalization and post-operative NPO duration. Besides, the procedure is a more feasible and simpler one that the J-pouch method as the significant lower duration of surgery, which is a considerable determinant in surgery and anesthegiology of pediatric patients.
Several studies reported postsurgical complications after surgery for Hirschsprung. Levitt et al. considered fecal incontinence a serious problem after operative management of Hirschsprung disease and attributed it to the surgical technique [11]. In addition, a very recent systematic review indicated higher rate of Fortunately, none of the studied groups in the present study were complicated with fecal incontinence during the three-years follow-up period. Keshtgar and colleagues evaluated 19 children with fecal incontinence and/or constipation undergoing Duhamel, Rehbein, and Soave operations and reported that the median time of referral after operation was 5 years [12]. Accordingly, the three-year follow-up period in the present study might not be sufficient enough for evaluation of fecal incontinence or constipation.
Hirschsprung-related enterocolitis is an important postsurgical complication as it causes morbidity and mortality [13]. Martínez- Criado et al. evaluated 73 patients undergoing transanal endorectal descent procedure for treatment of Hirschsprung and reported a 10% prevalence of postoperative enterocolitis, which was not associated with length of aganglionic segment [14]. Elhalaby and colleagues also reported 21.4% postoperative enterocolitis [15] and Hackam et al. reported a prevalence of 32% with no cases of mortality, which was associated with mechanical factors related to anastomotic complications and intestinal obstruction [16]. In the study by Marty et al, all cases of Hirschsprung-related death were due to postoperative enterocolitis [8], which indicates the significance of this postoperative complication. Carneiro et al. have also reported less postoperative enterocolitis after Duhamel procedure, compared to pull-through procedure and mentioned that it was associated with patient’s sex and family history of Hirschsprung disease [17]. Yet, the results of the present study indicated no cases of postoperative enterocolitis in ileorectal anastomosis, compared to 44.4% in J-pouch procedure, which was not associated with patient’s sex. Although different procedures have reported different rates of postoperative enterocolitis, none of the studies have reported zero cases for this complication, which was reported by the present study in the ileorectal anastomosis method (Table 1).
Marty and colleagues reported severe soiling as a common problem (12.6%) after surgical procedures, including endorectal pull-through, modified Duhamel and long side-to-side anastomosis for total colonic aganglionosis [8], which was 5-10% and statistically not different between the two procedures of the current study. A meta-analysis of studies compared the outcomes between laparoscopically-assisted and totally trans anal endorectal pull-through procedures in 405 patients, which documented no mortality rate with no statistically significant difference in fecal incontinence, constipation, and enterocolitis between the procedures [18].
The strengths of present study included comparing various complications between two procedures, in order to give physicians and researchers a broad overview on different postsurgical complications. However, the limitations of current study included small sample size and short follow-up, which was due to the low incidence of the disease. Therefore, it is suggested that multicentric studies provide larger sample sizes. In addition, future randomized controlled trials are recommended in order to provide a powerful evidence on the efficacy of each therapeutic procedure.
Conclusion
In conclusion, as the results of current study indicated, the surgical method of ileorectal anastomosis had priorities to J-pouch procedure, in patients with total colon aganglionosis, including less hospitalization time, surgical duration and NPO duration, no cases of enterocolitis, fecal incontinence or constipation, which, in general, proposes that ileorectal anastomosis is a more efficient method than J-pouch.
References
- Ikeda K, Goto S. Diagnosis and treatment of Hirschsprung's disease in Japan. An analysis of 1628 patients. Ann Surg. 1984;199(4):400.
- Sergi C. Hirschsprung’s disease: Historical notes and pathological diagnosis on the occasion of the 100th anniversary of Dr. Harald Hirschsprung’s death. World J Clin Pediatr. 2015;4(4):120.
- Szylberg Ł, Marszałek A. Diagnosis of Hirschsprung's disease with particular emphasis on histopathology. A systematic review of current literature. Przeglad gastroenterologiczny. 2014;9(5):264.
- Amiel J, Sproat-Emison E, Garcia-Barcelo M, et al. Hirschsprung disease, associated syndromes and genetics: A review. World J Med Genet. 2008;45(1):1-14.
- Teitelbaum DH, Cilley RE, Sherman NJ, et al. A decade of experience with the primary pull-through for Hirschsprung disease in the newborn period: A multicenter analysis of outcomes. Ann Surg. 2000;232(3):372-80.
- Tariq G, Brereton R, Wright V. Complications of endorectal pull-through for Hirschsprung's disease. J Pediatr Surg. 1991;26(10):1202-6.
- Dasgupta R, Langer JC. Evaluation and management of persistent problems after surgery for Hirschsprung disease in a child. J Pediatr Gastroenterol Nutr. 2008;46(1):13-9.
- Marty TL, Seo T, Matlak ME, et al. Gastrointestinal function after surgical correction of Hirschsprung's disease: long-term follow-up in 135 patients. J Pediatr Surg. 1995;30(5):655-8
- Minford J, Ram A, Turnock R, et al. Comparison of functional outcomes of Duhamel and transanal endorectal coloanal anastomosis for Hirschsprung’s disease. J Pediatr Surg. 2004;39(2):161-5.
- Zhang S, Li J, Wu Y, et al. Comparison of laparoscopic-assisted operations and laparotomy operations for the treatment of Hirschsprung disease: Evidence from a metaanalysis. Medicine. 2015;94(39).
- Levitt MA, Martin CA, Olesevich M, et al. Hirschsprung disease and fecal incontinence: diagnostic and management strategies. J Pediatr Surg. 2009;44(1):271-7
- Keshtgar A, Ward H, Clayden G, et al. Investigations for incontinence and constipation after surgery for Hirschsprung's disease in children. Pediatr Surg Int. 2003;19(1-2):4-8.
- Gosain A. Established and emerging concepts in Hirschsprung’s-associated enterocolitis. Pediatr Surg Int. 2016:1-8.
- Martínez-Criado Y, Cabrera R, Moya MJ, et al. Results of transanal endorrectal descent in Hirschsprung's disease. Cirugía Española (English Edition). 2015;93(9):561-6.
- Elhalaby EA, Coran AG, Blane CE, et al. Enterocolitis associated with Hirschsprung's disease: A clinical-radiological characterization based on 168 patients. J Pediatr Surg. 1995;30(1):76-3.
- Hackam DJ, Filler R, Pearl RH. Enterocolitis after the surgical treatment of Hirschsprung's disease: Risk factors and financial impact. J Pediatr Surg. 1998;33(6):830-3.
- Carneiro P, Brereton R, Drake D, et al. Enterocolitis in Hirschsprung's disease. Pediatr Surg Int. 1992;7(5):356-60.
- Thomson D, Allin B, Long AM, et al. Laparoscopic assistance for primary transanal pull-through in Hirschsprung's disease: A systematic review and meta-analysis. BMJ open. 2015;5(3):e006063.