Research Article - Archives of General Internal Medicine (2017) Volume 1, Issue 2
Clinical Analysis of Secondary Acquired Cholesteatoma
Takashi Yamatodani1*, Kunihiro Mizuta2, Shiori Endo1, Hiroshi Nakanishi1, Goro Takahashi3, Kiyoshi Misawa1, Seiji Hosokawa1 and Hiroyuki Mineta1
1Department of Otorhinolaryngology/Head & Neck Surgery, Hamamatsu University School of Medicine, Hamamatsu 431-3292, Japan
2Hamamatsu Medical Center, Hamamatsu 432-8580, Japan
3Yamahoshi ENT Clinic, Hamamatsu 432-8069, Japan
- *Corresponding Author:
- Takashi Yamatodani
Department of Otorhinolaryngology/Head and Neck Surgery
1-20-1 Handayama, Higashi-ku
Hamamatsu 431-3192, Japan
E-mail: ty@hama-med.ac.jp
Accepted on May 12, 2017
Citation: Yamatodani T, Mizuta K, Endo S, et al. Clinical analysis of secondary acquired cholesteatoma. Arch Gen Intern Med. 2017;1(2):12-16
Abstract
Objectives: To retrospectively analyse the clinical features of secondary acquired cholesteatoma.
Methods: Seventeen patients (17 ears) who underwent surgery for secondary acquired cholesteatoma between January 2009 and December 2013 were studied. The parameters examined included the sex and age of the patients and the size of the tympanic membrane perforation.
Results: There was a significant correlation between secondary acquired cholesteatoma and sex (18% men, 82% women). Patients with secondary acquired cholesteatoma (average, 56 years) were significantly older than those with other acquired cholesteatomas (average, 42 years). There was a trend toward lower likelihood of improvement in older patients after surgery.
Conclusion: Secondary acquired cholesteatomas differ from other acquired cholesteatomas in terms of patient sex and age. Improvements in postoperative hearing are more likely in younger patients. In some cases, secondary acquired cholesteatoma was diagnosed during surgery for chronic otitis media; therefore, it is very important to consider this possibility.
Keywords
Cholesteatoma, Epithelial invasion, Hearing improvement, Female predominance
Introduction
Most acquired middle ear cholesteatomas are thought to result from retraction or adhesion of the tympanic membrane. However, in some cholesteatomas, termed secondary acquired cholesteatomas, the epithelium of the tympanic membrane extends into the middle ear cavity through a perforation in the membrane. Owing to differences in aetiology, secondary acquired cholesteatomas may have clinical features distinct from those of other acquired cholesteatomas. In this study, we retrospectively analysed the clinical features of secondary acquired cholesteatomas.
Materials and Methods
There are no definitive diagnostic criteria for secondary acquired cholesteatoma. In this study, we used the following criteria: Perforation of the pars tensa without retraction or adhesion of the tympanic membrane [1]; Invasion of the epidermis of the tympanic membrane into the tympanic cavity at the edge of the perforation in the membrane [2]; and Requirement for surgery to remove the cholesteatoma from the tympanic cavity [3]. Between January 2009 and December 2013, 17 patients (17 ears) underwent surgery for secondary acquired cholesteatoma of the middle ear in our institution. The 17 secondary acquired cholesteatomas represented 12.7% of all acquired cholesteatomas primarily treated surgically during this period at this department. The ages of the 17 patients in our study ranged from 8 to 75 years (average, 56 years). Five patients were aged less than 49 years; 7, 50 to 65 years; and 5, more than 65 years. Follow-up examinations occurred over a period of 14 to 76 months (average, 31.7 months). There was no recurrence in any of the patients.
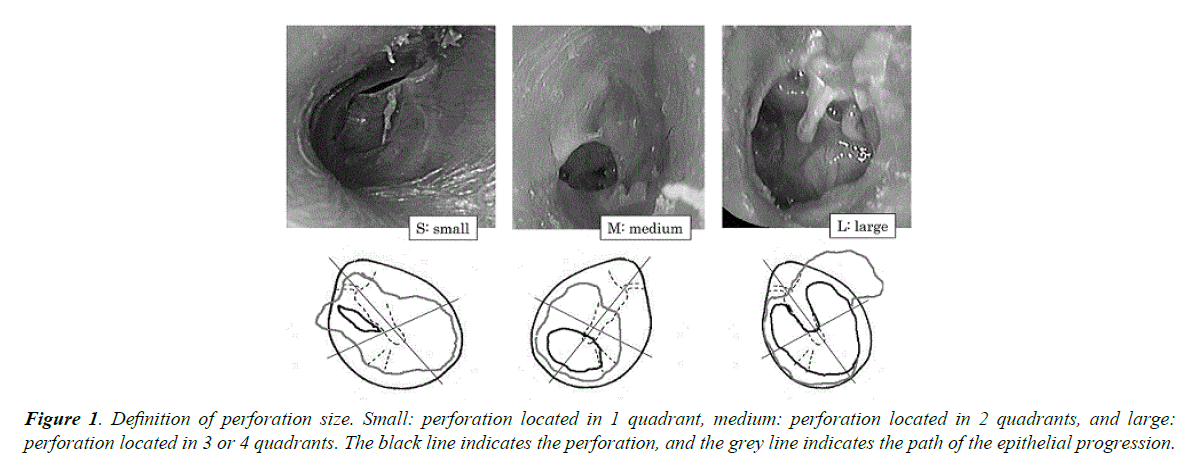
The size of the perforation in the tympanic membrane was defined as small (limited to 1 quadrant), medium (located in 2 quadrants), or large (located in 3 or 4 quadrants) (Figure 1). The hearing level was determined by measuring the pure tones at 3 frequencies (0.5, 1, and 2 KHz); the average value was recorded. Hearing was considered improved if 1 or more of the following criteria was fulfilled: Postoperative air-bone gap ≤ 15 dB [1], Preoperative to postoperative hearing gain ≥ 15 dB [2], or Postoperative air conduction level ≤ 30 dB [3]. The details of all 17 cases are summarized in Table 1. We examined the clinical features of secondary acquired cholesteatomas and compared them with the features of other acquired cholesteatomas and chronic otitis media. Statistical analysis was performed by using StatMateIV® software (ATMS, Tokyo, Japan). This research was approved by the institutional review board, and written informed consent was obtained from all participants prior to enrolment.
| Case | Age | Sex | Operation | Canal wall | Mastoidectomy/atticotomy | Size of Perforation | Ottorhea | MRSA | Success/Failure |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 46 | M | IIIc | Canal up | Mastoidectomy | S | Success | ||
| 2 | 35 | F | IIIc | S | Success | ||||
| 3 | 30 | F | I | M | ⁺ | Success | |||
| 4 | 62 | F | IIIc | L | ⁺ | ⁺ | Success | ||
| 5 | 65 | M | wo | Canal down | Mastoidectomy | L | ⁺ | ⁺ | Success |
| 6 | 67 | F | IIIc | L | Failure | ||||
| 7 | 74 | F | IIIc | Canal up | Mastoidectomy | L | ⁺ | ⁺ | Success |
| 8 | 65 | F | I | L | ⁺ | Failure | |||
| 9 | 8 | F | I | S | Success | ||||
| 10 | 75 | F | IIIc | Canal down | Mastoidectomy | L | Failure | ||
| 11 | 33 | M | I | M | Success | ||||
| 12 | 65 | F | IIIc | Canal down | Mastoidectomy | M | Success | ||
| 13 | 62 | F | IIIc | S | ⁺ | Success | |||
| 14 | 68 | F | IIIc | M | Failure | ||||
| 15 | 74 | F | IIIc | Mastoidectomy | L | Success | |||
| 16 | 65 | F | IIIc | Mastoidectomy | L | ⁺ | Success | ||
| 17 | 62 | F | IIIc | M | Success |
Table 1. Clinical characteristics. S: Small; M: Medium; L: Large; MRSA: Methicillin-Resistant Staphylococcus aureus.
Results
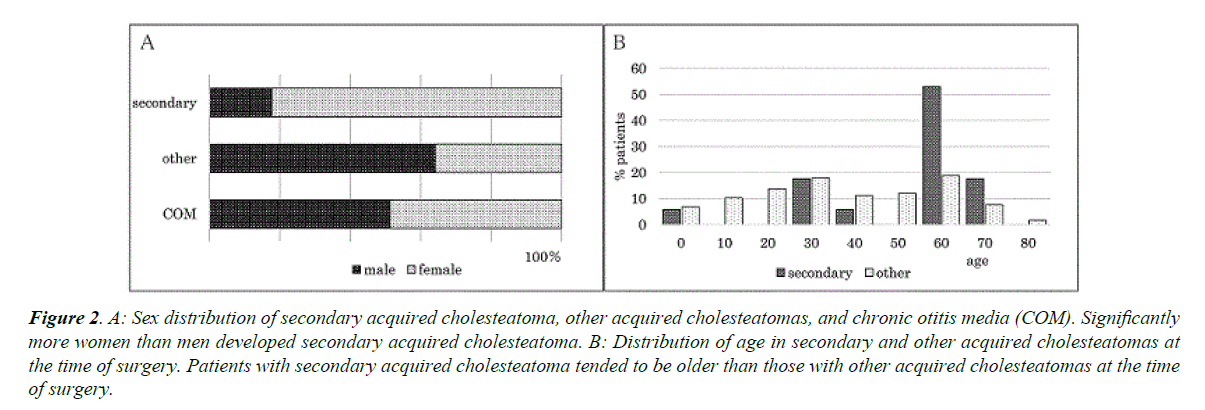
Four patients were diagnosed with chronic otitis media preoperatively. They were diagnosed intraoperatively with secondary acquired cholesteatoma owing to the presence of apparent epithelial debris in the middle ear cavity. All 17 secondary acquired cholesteatomas in our study were unilateral (right, 8 cases; left, 9 cases), with no significant laterality. Secondary acquired cholesteatomas were more prevalent in women (n=14, 82%) than in men (n=3) (p ≤ 0.05, Fisher’s exact test) (Figure 2A). This was not the case for patients with other acquired cholesteatomas (men 75; women, 42) or chronic otitis media (men, 40; women 38) that were surgically treated at our department during the same period.
Figure 2. A: Sex distribution of secondary acquired cholesteatoma, other acquired cholesteatomas, and chronic otitis media (COM). Significantly more women than men developed secondary acquired cholesteatoma. B: Distribution of age in secondary and other acquired cholesteatomas at the time of surgery. Patients with secondary acquired cholesteatoma tended to be older than those with other acquired cholesteatomas at the time of surgery.
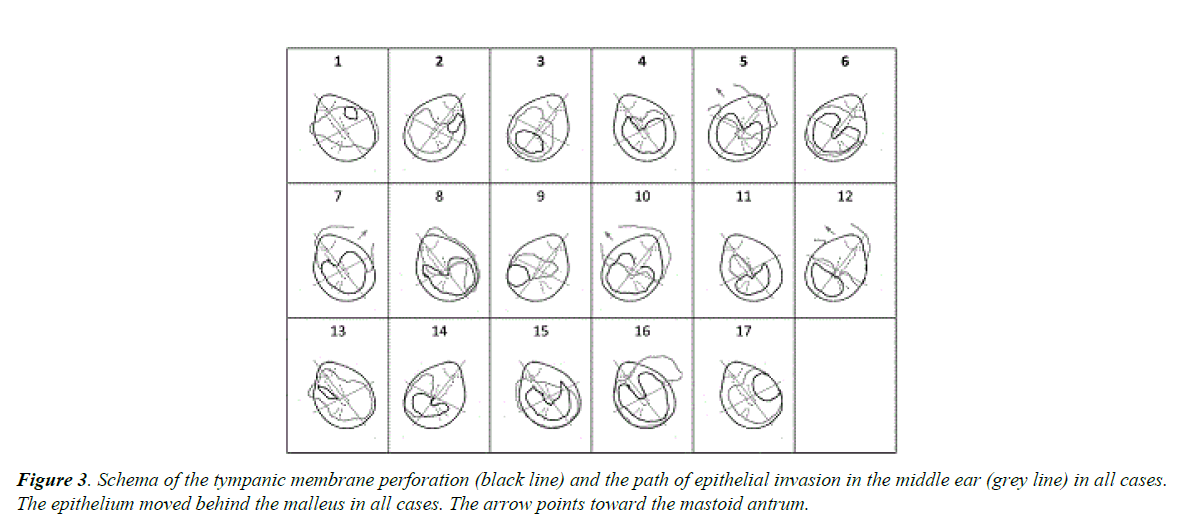
Patients with secondary acquired cholesteatoma were older (8-75 years; average, 56 years) than those with other types of acquired cholesteatomas (average, 42 years) (p ≤ 0.05, Wilcoxon rank sum test) (Figure 2B). Otorrhoea was observed in 7 (41.2%) of the 17 ears preoperatively; 4 of the 7 were infected with Methicillin-Resistant Staphylococcus Aureus (MRSA) as detected via culturing. The size of the perforation in the tympanic membrane was large in 8 (47.1%) of the 17 ears, medium in 5 (29.4%), and small in 4 (23.5%). In 9 (52.9%) of the 17 ears, the perforation was located in the posterior quadrants of the tympanic membrane. The epithelium extended into the middle ear behind the malleus in all cases and up to the mastoid antrum in 4 (23.5%) patients (Figure 3).
The types of surgery performed were as follows: canal up tympanoplasty with mastoidectomy, 2 (11.8%) ears; tympanoplasty with canal down mastoidectomy, 3 (17.6%) ears; and tympanoplasty with transcanal atticotomy, 2 (11.8%) ears. In the 10 (58.8%) cases in which the cholesteatoma was located in the middle ear cavity, tympanoplasty without atticotomy or mastoidectomy was performed. Other procedures included ossiculoplasty, 16 (94.1%) ears; Wullstein type I methods, 4 (25%) of 16 ears; and modified type III with columella, 12 (75%) ears.
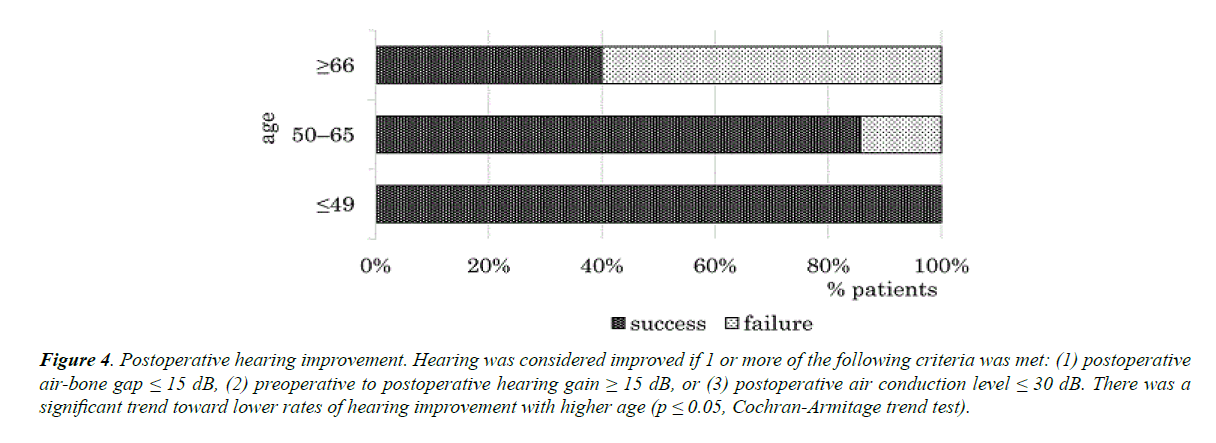
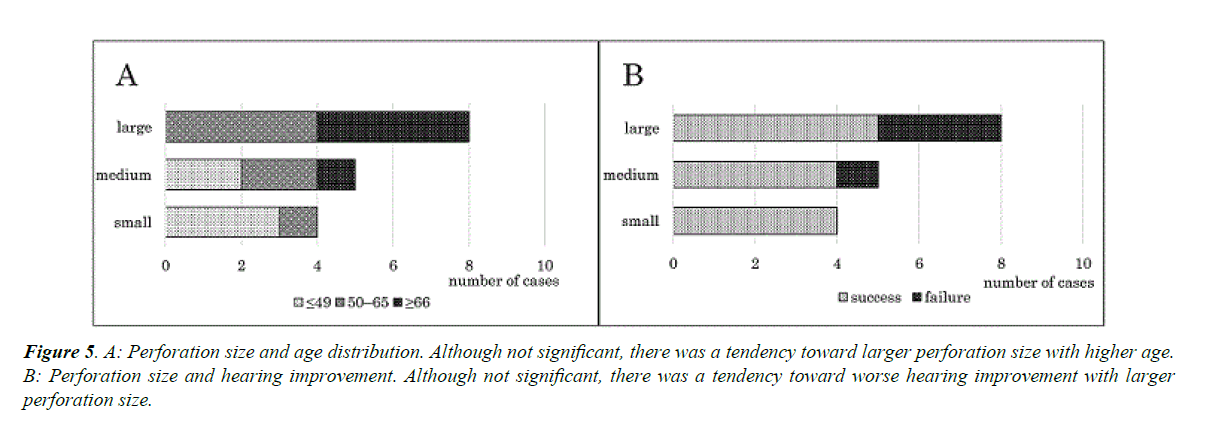
Postoperative hearing improvement was observed in 13 (76.5%) ears. There was a significant correlation between age and postoperative hearing improvement, specifically, a trend toward lower likelihood of improvement with advanced age (p ≤ 0.05, Cochran-Armitage trend test) (Figure 4). In contrast, there was no significant correlation between hearing improvement and otorrhoea, MRSA infection, mastoidectomy, or the location of the perforation. Although not significant, a tendency toward larger perforation sizes in older patients (Figure 5A) and patients without hearing improvement (Figure 5B) was observed. Cholesteatoma did not recur in any of the 17 ears.
Figure 4. Postoperative hearing improvement. Hearing was considered improved if 1 or more of the following criteria was met: (1) postoperative air-bone gap ≤ 15 dB, (2) preoperative to postoperative hearing gain ≥ 15 dB, or (3) postoperative air conduction level ≤ 30 dB. There was a significant trend toward lower rates of hearing improvement with higher age (p ≤ 0.05, Cochran-Armitage trend test).
Figure 5. A: Perforation size and age distribution. Although not significant, there was a tendency toward larger perforation size with higher age. B: Perforation size and hearing improvement. Although not significant, there was a tendency toward worse hearing improvement with larger perforation size.
Discussion
Most acquired cholesteatomas develop from retraction of the pars flaccida or pars tensa of the tympanic membrane. However, there are a few reported cases in which the epidermis of a perforated tympanic membrane invades the middle ear cavity at the edge of the perforation, resulting in the formation of debris and/or epidermal cysts. This rare phenomenon has been termed secondary acquired cholesteatoma [1,2]. Owing to their different mechanisms of development compared with acquired cholesteatomas originating in the retraction pocket, secondary acquired cholesteatomas have distinct features.
Epithelial invasion of the middle ear occurs in about 30% of tympanic membrane perforation cases [3,4] and is almost always accompanied by chronic otitis media, which should be borne in mind. Other causes of cholesteatoma include injury of the tympanic membrane and ventilation tube insertion. Children aged less than 5 years who have tubes inserted frequently or for more than 12 months or have experienced repeated otorrhoea [5] are at risk of cholesteatoma, and 1.1% of ventilation tube insertions result in cholesteatoma.
Cytokines produced in response to inflammation in the area surrounding the perforation in the tympanic membrane are thought to promote the growth of the tympanic membrane epithelium [6-8]. Following inflammation, further invasion of the epithelium into the middle ear cavity occurs. Consequently, full development of secondary acquired cholesteatomas requires longer times than does development of other acquired cholesteatomas, and patients undergoing surgery for secondary acquired cholesteatoma are usually older [2,9]. Similarly, in our study, the age distribution at the time of surgery was higher in patients with secondary acquired cholesteatomas than in those with other acquired cholesteatomas. There was also a tendency toward poor hearing improvement in older patients with secondary acquired cholesteatoma, perhaps in part because long-term inflammation causes fixation of the ossicular chain.
The preponderance of women compared with men with secondary acquired cholesteatoma has been reported [2] and this was also observed in our study. The reason for the female predominance is not known, although sex hormones are likely involved. As also shown in our study, the percentage of women with secondary acquired cholesteatomas was higher than the percentage of women with other cholesteatomas or chronic otitis media.
The epithelium grows from the centre of the tympanic membrane in the direction in which the tympanic membrane migrates; therefore, it easily extends from the malleus tip to behind and around the malleus handle and tensor tympanic tendon [9,10]. This pattern was observed in all cases in our study; therefore, operating around the tensor tympanic tendon is important. When cholesteatomas extend to the attic and/or mastoid cavity, atticotomy or mastoidectomy is required. Although it was expected that patients receiving these procedures would have worse hearing results than those receiving other procedures, this was not case (i.e., there was no significant correlation between the procedure used and hearing improvement). In addition, when the perforation is located in the posterior region of the tympanic membrane, it more easily impairs ossicular conduction. However, the location of the perforation did not affect hearing improvement. There was also no significant correlation between hearing improvement and preoperative otorrhoea or MRSA infection, despite their capacity to impede wound healing and ossicular conductive function. To clarify the effects of these clinical conditions on cholesteatoma, examination of more cases is necessary.
Conclusion
In this study, we retrospectively studied 17 cases of secondary acquired cholesteatoma. Secondary acquired cholesteatoma is a rare disease, and we show that it has features distinct from those of other acquired cholesteatomas. It was more prevalent in women than in men and usually treated (via surgery) in patients at a relatively advanced age. There was a tendency toward poor hearing improvement in such patients. Therefore, it is important to diagnose and surgically treat secondary acquired cholesteatoma as soon as possible. Cholesteatoma is sometimes found during surgery for chronic otitis media, and surgeons should be aware of this possibility. Future studies should carefully examine more cases of secondary acquired cholesteatoma.
References
- Isaacson G. Diagnosis of pediatric cholesteatoma. Pediatrics. 2007;120:603-8.
- Yamamoto K, Yaguchi Y, Kojima H. Clinical analysis of secondary cholesteatoma. Am J Otolaryngol. 2014;35:58-93.
- Somers TH, Houben V, Goovaerts G, et al. Histology of the perforated tympanic membrane and its muco-epithelial junction. Clin Otolaryngol Allied Sci. 1997;22:162-6.
- Oktay MF, Cureoglu S, Schachern PA, et al. Tympanic membrane changes in central tympanic membrane perforations. Am J Otolaryngol. 2005;26:393-7.
- Golz A, Goldenberg D, Netzer A, et al. Cholesteatomas associated with ventilation tube insertion. Arch Otolaryngol Head Neck Surg. 1999;125:754-7.
- Sudhoff H, Bujía J, Fisseler-Eckhoff A, et al. Expression of a cell-cycle-associated nuclear antigen (MIB1) in cholesteatoma and auditory meatal skin. Laryngoscope. 1995;105:1227-31.
- Kojima H, Matsuhisa A, Shiwa M, et al. Expression of messenger RNA for keratinocyte growth factor in human cholesteatoma. Arch Otolaryngol Head Neck Surg. 1996;122:157-60.
- Tanaka Y, Shiwa M, Kojima H, et al. A study on epidermal proliferation ability in cholesteatoma. Laryngoscope. 1998;108:537-42.
- Yamamoto Y, Takahashi K, Morita Y, et al. Clinical behavior and pathogenesis of secondary acquired cholesteatoma with a tympanic membrane perforation. Acta Otolaryngol. 2013;133:1035-9.
- Makino K, Amatsu M, Kinishi M, et al. Epithelial migration in the healing process of tympanic membrane perforations. Eur Arch Otorhinolaryngol. 1990;247:352-5.