Review Article - Journal of Public Health and Nutrition (2018) Volume 1, Issue 3
Can diet alone control inflammation? A comprehensive narrative review of dietary foods and supplements and their effects on inflammation and pain.
Michael Sabia1*, Kingsuk Ganguly1, Robert G. Gessman1, Jill Kalariya1, Rajat Mathur2¹Cooper University Hospital, Camden, New Jersey, USA
²MedStar Georgetown University School of Medicine, Washington DC, USA
- *Corresponding Author:
- Sabia M
Cooper University Hospital
Camden, New Jersey, USA
Email: sabia-michael@cooperhealth.edu
Accepted date: June 18, 2018
Citation: Sabia M, Ganguly K, Gessman RG, et al. Can diet alone control inflammation? A comprehensive narrative review of dietary foods and supplements and their effects on inflammation and pain. J pub health catalog. 2018;1(3):1-8.
DOI: 10.35841/public-health-nutrition.1.3.57-64
Visit for more related articles at Journal of Public Health and NutritionAbstract
In most cases, the development of pain is due to an inflammatory etiology, regardless of the underlying etiology. There is a clear understanding of the inflammatory pathways in which there is a role for anti-inflammatory medications to alleviate the inflammation leading to pain relief. The use of prescription and non-prescription Non-Steroidal Anti-Inflammatory Drugs (NSAID) is still thought to be the first line treatment in treating pain arising from an inflammatory etiology. However, long-term usages of NSAIDs have safety concerns which often limit their use for chronic painful conditions. Understanding the inflammatory pathway, potentially dangerous side effects of NSAIDs and commonly used anti-inflammatory supplements may offer a safer and more effective, alternative treatment for an anti-inflammatory pain relief. This article is a narrative review of the current literature as such it lacks quantitative data synthesis and is not intended to be a systematic review. Further high quality randomized controlled trials are needed to substantiate the long term safety and efficacy of dietary foods and supplements on decreasing inflammation and pain.
Keywords
Anti-inflammatory diet, Inflammation, Natural anti-inflammatory, Pain, Inflammation pathway
Introduction
We really are what we eat. Our society and medical practices currently undervalue the relationship between nutrition and our daily lives. Whether it is immunomodulation via the enteric system, anti-inflammatory nutrients, or obesity, what we eat is increasingly being found to have correlation to our world and how our patients perceive and experience pain. It has even been suggested that “you change your body chemistry every time you eat” [1]. Obesity has become an epidemic worldwide; not only does it play a role in metabolic disorders and cardiovascular comorbidities, but it also has a high prevalence in patients with chronic pain. A significant relationship has been demonstrated between pain and hemoglobin A1C levels in mainly the African American population [2].
Inflammation Overview
Inflammation is common to chronic diseases including chronic pain. Activation of the immune system causes release of cytokines, which can be either proinflammatory or antiinflammatory. Patients with chronic pain may have increased proinflammatory cytokine levels and/or decreased antiinflammatory cytokine levels.
Our immune systems are comprised of two parts: the adaptive and the innate immune systems. Both are involved in acute and chronic pain. The adaptive immune system uses antibodies, T cells, and B cells as a form of immunological memory from previous exposure to pathogens and is able to mount a response to infection on subsequent exposure. More specifically, Th1 proinflammatory cells and Th2 anti-inflammatory cells release respective cytokines and work together to maintain balance [3].
The innate immune system is comprised of various cell types that express cell surface receptors (commonly toll-like receptors, or TLR) to recognize bacterial components, become activated, and mount an immediate response by releasing proinflammatory cytokines. In this way, more commonly encountered bacteria - or rather its components- can be recognized immediately and reacted to without the need for antibody development. The innate immune system also recruits the adaptive immune system to help balance with anti-inflammatory cytokines.
Proinflammatory cytokines of the innate immune system like interleukin 1 (IL-1) and interleukin 6 (IL-6) cause C-reactive protein (CRP) to be synthesized during times of inflammation; CRP can be measured in blood and hence be used as a marker of inflammation. Increased CRP levels are found in various disease states including some with chronic pain states like low back pain and fibromyalgia and even in obesity.
Obesity involves increased adipose tissue, which releases a hormone called leptin. Leptin is involved in hunger regulation, but it also causes release of proinflammatory cytokines. The higher the adipose tissue accumulation, the higher will be the levels of leptin and its effects. The obese population may therefore experience this continuous proinflammatory state and activation of the immune system. On the other hand, weight loss has been shown to reduce CRP and inflammatory cytokine levels [4].
Effect of Diet on Pain and Inflammation
Diet plays a large role in modulating our immune systems. About 80% of the immune system lies adjacent to the GI tract and therefore both intake and inflammation of the GI tract may have an effect on pain. The location of excess body fat accumulation determines whether or not obesity can lead to acceleration of chronic diseases [5].
A Western diet is one consisting of high intake of red meat, refined sugars, processed food, and saturated fats and is linked to obesity and metabolic disorders [6,7]. Veronese et al. and Sanchez et al. demonstrated that a better quality of life and decreased pain was achieved with adherence to a Mediterranean diet, which consists of nuts, fish, unrefined carbohydrates, and olive oil. Inflammatory serum markers IL-6 and CRP were reduced after adherence to a Mediterranean diet (Mena et al.). The Mediterranean diet may also decrease pain and aid in weight loss. Classic vegetarian or vegan diets consisting of fruits, vegetables, and legumes, all of which are anti-inflammatory, have been shown to decrease chronic pain from various causes. Different diets alter the inflammatory state within the body, but addition or elimination of particular foods can be helpful in improving inflammation and pain also. For example, a study performed on obese mice using olive oil as a supplement to their diet demonstrated lower levels of inflammation and weight loss [8]. The amount of overlap that exists between the antiinflammatory diet and cancer prevention diet is enough to realize the detrimental role inflammation has on our gene expression and cell physiology.
Plant-food supplements have anti-inflammatory effects. Fruits that are high in anthocyanins have shown to be antiinflammatory. Carotenoids, found in red, yellow, and orange vegetables work via reducing proinflammatory pathways and causing a reduction in pain. Other vegetables, including broccoli, cauliflower, cabbage, and bok choy have various amount of a component that also reduces inflammatory pathways and reduces pain. Studies done on green tea extract show that it has strong anti-inflammatory properties. Soy causes suppression of proinflammatory cytokines also. Both ginger and turmeric also work through multiple anti-inflammatory pathways and decrease pain. The proinflammatory effect of caffeine might suggest a negative effect on pain, but clinical studies have shown that using caffeine as an adjuvant in some types of headaches helps to improve this type of pain.
Anti-Inflammatory Drugs and Common Side Effects
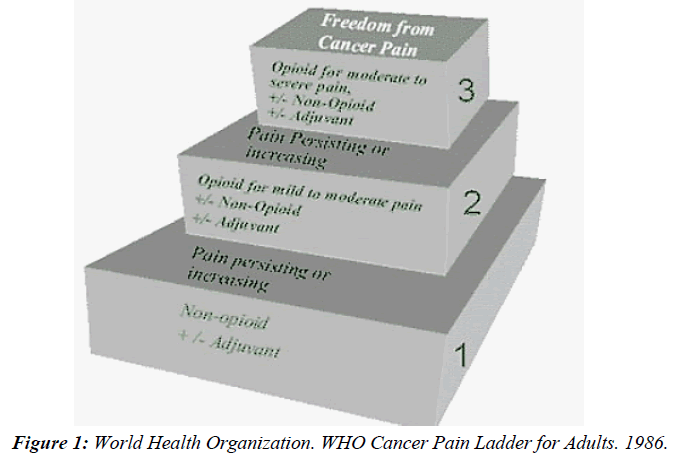
Anti-inflammatory medications such as acetaminophen, NSAIDS (Non-Steroidal Anti-Inflammatory Drugs), and selective COX-2 (Cyclooxygenase-2) inhibitors are considered to be first-line analgesics for acute and chronic pain by the Center for Disease Control. A Cochrane Review on treatments for cancer pain failed to demonstrate superiority of opioid therapy or combination opioid/NSAID therapy compared to NSAID therapy alone [9]. Similarly, a randomized control study of naproxen for non-radicular acute low back pain failed to show superiority if combined with low dose opioids at one week [10]. Additionally, the World Health Organization cancer pain treatment ladder shown in Figure 1 recommends these same non-opioid anti-inflammatory medications as first line therapy for cancer pain.
With the continuing mortality and morbidity associated with opioid use in the United States there is a growing body of research being dedicated to non-pharmacologic and pharmacologic nonopioid interventions for acute and chronic pain syndromes. However, not all patients are candidates for NSAID therapy due to well-documented cardiac, gastrointestinal, and renal adverse effects of these medications in some populations. In fact the FDA and CDC warn that NSAIDs increase risk for heart attack, stroke, gastritis, peptic ulcer disease, gastric perforation, and GI bleed with increasing risk with higher dose or longer duration of use. Among NSAIDs naproxen is considered to have the safest cardiovascular risk profile while the COX-2 selective medications such as celecoxib is considered to have one of the safest GI risk profiles while being the only NSAID that does not appear to inhibit platelet function [11,12]. It has been estimated that NSAID-related mortality among patients with osteoarthritis or rheumatoid arthritis in the United States is a staggering 16,500 deaths per year [13]. As with opioid prescribing the lowest effective dose of NSAIDs is recommended for the shortest time necessary to avoid adverse effects.
Natural Compounds for Inflammation
Natural compounds have been used in traditional medicine due to a variety of pharmacological properties. Inflammation as mentioned above is the body's reaction to a toxin, allergen, or lesion, and reactive oxygen species (ROS) are created as a by-product. Antioxidants are needed to help clear these ROS. Natural compounds have the ability to cause an inhibitory effect on this inflammation and improve oxidative stress from ROS. Flavonoids and phenol compounds have been studied numerous times and have demonstrated antioxidant activities [14]. The NF-kB pathway is a signalling pathway which plays a role in producing proinflammatory mediators.
Medicinal plants that actvia this pathway to reduce inflammation include Acanthopanax senticosus Harms, Actinidia arguta, Hibiscus sabdariffa, Angelica keiskei, and Artemisiae annuae Herba [15]. Many plant derivatives also include the benefit of being more affordable and having minimal to no side effects, though this should always be reviewed prior to using. On the other hands, all of these derivatives don't always have clinical studies or mechanisms of actions known.
An example of a plant-based phenol compound is resveratrol, derived from the Japanese Knot weed or Polygonum cuspidatum. While this compound helps to protect the plant and acts as a defense on its skin, it has been shown to have anti-inflammatory actions when ingested [16]. In particular, studies have shown its help in arthritis, including a study by Elmali et al. which used intra-articular injections to help knee osteoarthritis [17]. Two compounds, Cortex Phellodendri and Humulus japonicus, were studied by Yeonsu et al. in their effectiveness as alternative treatment options for PID in mice due to their anti-inflammatory effects. Clinical signs of inflammation and cytokine expression were both reduced, indicating that these herbs can potentially be alternative treatments for PID [18].
ATP-gated ion channels called the P2X subfamily play an important role in inflammation and pain signaling. These are being used as targets for the development of new pharmacological agents in the treatment of pain [19]. Molecules from natural products, including emodin, amentoflavone, ligustrazine and puerarin have a role in antagonizing P2X receptors, thereby decreasing inflammation and pain. Further investigation and studies in the role of these compounds needs still to be done but may play a role in future treatment options for pain and inflammation.
Anti-Inflammation Nutrition: The Anti- Inflammatory Nature of Fruits and Vegetables
Over two millennia ago Hippocrates suggested “Let food be thy medicine and medicine be thy food.” Despite the lack of emphasis on nutrition in traditional medical education curriculum, research is now growing, demonstrating that Hippocrates’ approach remains valid in modern medicine as well. Studies on the influence of diet on inflammatory markers support diets high in fiber, healthy oils, fruits, and vegetables while low in sugars, starchy carbohydrates, meat and unhealthy oils can reduce inflammation to mitigate a wide array of chronic diseases including pain syndromes [20-25]. Fruits and vegetables can be a source of vital micronutrients such as vitamins, minerals, and antioxidants that cannot otherwise be produced by the human body. In comparison with pharmaceuticals that are foreign to the human body and often have relatively rapid and dramatic effects, natural micronutrients tend to have more gradual effects (Table 1).
| Dietary Supplement | Support | Opposition |
|---|---|---|
| Fish Oil | Some evidence for benefit in cardiovascular disease and osteoarthritis. Provides Omega-3 and Omega-6. | widely varying components and dosages and often unknown amounts of toxic heavy metals such as mercury |
| Turmeric (Curcumin) | Some evidence for benefit in osteoarthritis, rheumatoid arthritis, inflammatory bowel disease, multiple types of malignancies, and neurodegenerative disease. less adverse events than ibuprofen as anti-inflammatory in some studies | Iron deficiency anemia rarely with doses >12g daily High dosing requirements due to rapid metabolism |
| Green Tea | Some evidence for benefit in cancer, obesity, diabetes, cardiovascular disease, and neurodegenerative diseases | Possible liver toxicity at doses >10mg/kg/day in those predisposed |
| Willow Bark | Some evidence for benefit in osteoarthritis and rheumatic arthritis, moderate evidence for low back pain | Possible contraindication in patients allergic to salicylates |
| Cayenne | Some evidence for benefit in low back pain, post-herpetic neuralgia, peripheral neuropathies, chronic musculoskeletal pain | Uncomfortable and undesirable burning sensation when it is applied to the skin |
| Noni | Some evidence for benefit in low arthritis, ligament injuries, tendinosis and also other non-inflammatory painful diseases such as dysmenorrhea | Possible liver toxicity at high doses in those predisposed. Due to high potassium content in Noni fruit this may be a contraindication for those with severe kidney disease. |
| Blueberries | Some evidence for benefit in reducing risk of coronary artery disease | High Vitamin K content can decrease effectiveness of blood thinners such as warfarin Possible contraindication in patients allergic to salicylates |
Table 1: Summary of support and opposition for utilization of dietary supplements for treatment of inflammation and pain.
Of course not all fruits and vegetables have the same beneficial effects. Despite the lack of funding to research the benefits of naturally occurring chemicals, many compounds from fruits and vegetables have been identified that show promise in reducing inflammation including the following: PUFAs (polyunsaturated fatty acids) from fish oil, Pycnogenol from willow bark, capsaicin from cayenne peppers, scopoletin from Noni, anthocyanins from blueberries, GSPE (grape seed proanthocyanidin) from grape seeds, EGCG (epigallocatechin gallate) from green tea, the isothiocyanate sulforaphane (SULF) from cruciferous vegetables, β-carotene from carrots, lycopene from tomatoes, and curcumin from turmeric.
Many cultures have varieties of fruits and vegetables that are indigenous to the region and many areas have fruit only during some seasons. Other regions must import all fruits and vegetables contributing to wide variation in regional cost and popularity of fruit and vegetable consumption. For this reason daily dietary intake can be supplemented with naturally found components to improve quality of life and prevent or mitigate chronic disease.
This section will summarize evidence for and quality concerns with some naturally derived fruits, vegetables, plants, and other products that have shown benefit for inflammation and pain.
Fish oil (Omega-3 EFAs)
PUFAs are fatty acids commonly found in fish oil and include essential Omega-3 and Omega-6 fatty acids which cannot be produced by the human body without supplementation and are essential to normal growth and development. While Omega-6 PUFAs are a precursor to arachidonic acid and the proinflammatory pathway of prostaglandin production, Omega-3 PUFAs can be substituted for Omega-6 PUFAs in cell membranes and inhibit the inflammatory process. Specifically, eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) have been identified as Omega-3 subtypes that offer the most anti-inflammatory benefit.
Unlike the potential adverse cardiovascular effects of NSAID, research suggests Omega-3 fatty acids may prevent cardiovascular disease but further research is needed to confirm this [26]. EPA and DHA has been shown to reduce proinflammatory mediators and increase joint lubrication in laboratory and canine studies but human studies have been less consistent to show benefit for joint disease [27]. The Multicenter Osteoarthritis Study in 2012, an observational study of Omega-3 and Omega-6 plasma levels, found that knee patellofemoral cartilage loss was inversely associated with Omega-3 plasma levels [28]. Daily dosing of 2700 mg of Omega-3 PUFAs is suggested for anti-inflammatory effect noting benefits may be delayed up to 3-4 months [29,30]. Some commercially sold single-serving mackerel cans are advertised to contain 3500 mg of Omega-3 PUFA per serving whereas fish oil supplements have widely varying components and dosages and often unknown amounts of toxic heavy metals such as mercury.
Turmeric (Curcumin)
Curcumin is considered the active element providing benefit from the Turmeric root and is one of the most commonly prescribed anti-inflammatory phytotherapies utilized by herbalists. There is growing evidence to suggest the anti-inflammatory effects of curcumin may benefit numerous conditions such as osteoarthritis, rheumatoid arthritis, inflammatory bowel disease, multiple types of malignancies, and neurodegenerative disease [31,32]. In vitro and animal studies hold promise that curcumin acts as a potent anti-inflammatory mediator of numerous mediators such as NO, PGE2, TNF, IL-1, IL-6, IL-8, and matrix metalloproteinase-3 (MMP-3) [33,34].
Multiple randomized controlled trials spanning 4 to 8 weeks have compared curcumin at doses of 1200 mg-2 g daily in 3 divided doses compared to 800 to 1200 mg daily ibuprofen with comparable efficacy in pain and physical function yet less adverse events with curcumin than ibuprofen [35-37]. Curcumin has even been found to be effective as an immunosuppressant adjuvant to cyclosporine to prevent rejection and improve renal function after renal transplant [38,39]. Unlike the adverse renal and cardiac effects of NSAIDS, curcumin has been suggested as a cost-effective treatment for chronic kidney disease [40]. Adverse effects of curcumin such as iron deficiency anemia are generally rare and typically dose dependent with some studies trialing doses as high as 12 g daily [41]. Further research is needed to optimize the dosing and identify a solution to the limited bioavailability of curcumin requiring multiple and repetitive dosing but initial research is promising.
Green Tea
Black, green, oolong, yellow and white teas are derived from leaves of the Camellia sinensis plant using different growing and treatment processes [42]. Epigallocatechin gallate (EGCG), a major component of Green tea, is polyphenol (a type of catechins) responsible for antioxidant and anti-inflammatory effects that may benefit a variety of conditions including cancer, obesity, diabetes, cardiovascular disease, and neurodegenerative diseases. EGCG health benefits are mediated by reduction of NF-kappa B and AP-1 activity and reactive oxygen species [43-45]. While dosage of EGCG varies widely based upon species of tea, steeping time, oxidizing time while being processed, a cup of green tea typically contains approximately 50 mg of EGCG while supplement forms may contain much higher concentrations. While green tea is noted to have no severe adverse effects, dosage greater than 10 mg/kg/day can cause hepatic injury in those who are predisposed [46,47].
Willow bark (Pycnogenol)
Willow bark, or Salix alba, has been used for its anti-inflammatory and analgesic properties for thousands of years [48]. It contains salicin, which is chemically related to salicylic acid and is attributed to some- but not all- of its analgesic properties. Willow bark also contains flavonoids, and polyphenolics, which also contribute to its beneficial effects. Studies performed to explain the effects of willow bark show significant anti-inflammatory action via inhibition of proinflammatory cytokines TNFα, COX-2, and transcription factor NF-κB [49].
Willow barks use has been shown to improve pain from musculoskeletal disorders including rheumatic pain in both short term and long term clinical trials [50]. On the other hand, a study by Biegert et al. investigated the efficacy or willow bark in patients with osteoarthritis and rheumatic arthritis via two randomized double-blind controlled trials and reported no efficacy in either trial [51]. A literature review performed by Vlachojannis JE et al. looked at studies in which willow bark extracts were used for low back pain using daily doses up to 240 mg salicin over a time frame of up to six weeks and reported moderate evidence of effectiveness. Finally, a Cochrane review on willow bark extract for low back pain reported moderate quality evidence that daily doses containing 120 mg or 240 mg salicin are probably better than placebo for short term improvement in pain and rescue medication [52] .
Salicin does not appear to have the same side effects as salicylates such as abdominal pain, and studies reported minimal to no adverse effects, including minimal effect on platelet thrombosis. People with allergies to salicylic acid should avoid willow bark.
Cayenne pepper
A Cochrane review of herbal medicines for low back pain done by Oltean et al. showed that cayenne in plaster form reduced pain more than placebo [52]. The cayenne pepper is a type of capsicium and is now grown throughout the world. Capsaicin generates selective regional anesthesia by causing deterioration of capsaicin-sensitive nociceptive nerve endings. This results in significant and long-lasting extension in nociception [53]. Capsaicin activates the main receptor for nociception, called the transient receptor potential vanilloid 1 and also inhibits the NF-kB, resulting in its anti-inflammatory effect [54]. Capsaicin when used may cause a uncomfortable and undesirable burning sensation when it is applied to the skin. The topical formulation is available to treat post-herpetic neuralgia and has been mixed with other natural anti-arthritic preparations to be used for peripheral neuropathies and chronic musculoskeletal pain.
Noni (Morinda citrifolia L.)
Morinda citrifolia (also known as noni) is a tropical fruit which has medicinal use in the Polynesia islands, South East Asia, and Australia. It is commonly used for treatment of inflammatory conditions such as arthritis, ligament injuries, tendinosis and also other non-inflammatory painful diseases such as dysmenorrhea [55]. The fruit contains major anti-inflammatory constituents such as ursolic acid, scopeletin, and quercetin. Ursolic acid is known to have anti-inflammatory properties. Scopoletin mainly inhibited the synthesis of myeloperoxidase and PGE-2, quercetin has properties which suppresses the effect of IL-6 production. Both of these constituents showed moderate inhibition on IL-1β production [56].
Blueberries
Blueberries, which fall under the Genus Vaccinium, are a popular fruit in North America. Vaccinium corymbosum, also known as the northern high bush blueberry, has been studied for its anti-inflammatory and antinociceptive properties. The bioactive compounds belonging to the classes of proanthocyanidin and anthocyanin are thought to carry antioxidant, anti-inflammatory, and anticarcinogenic properties [57]. Blueberries carry these compounds in a large amount, thus giving them their hue. The effects of anthocyanin have also been studied in neuroscience and cardiology models. Their protective effects may reduce the risk of coronary artery disease [58]. They have been shown to inhibit platelet aggregation [59].
In one study, rat paw edema was induced by injecting carrageenan or histamine, substances known to cause inflammation. Neutrophil infiltration was then studied indirectly by measuring myeloperoxidase activity at 6 and 24 hour time points while being exposed to blueberry extract [60]. Reductions in edema activity were similar when compared to indomethacin and hydroxyzine, common pharmaceutical anti-inflammatory agents, thus displaying the fruit’s capabilities of having antiinflammatory and antihistamine properties.
Quality Assurance
With so many products on the market, it can seem overwhelming as to what is the right choice. What makes things more challenging is that most products are not tested or regulated by the FDA directly. There is always the risk of side effects from the supplements themselves, as well as the supplements interacting with prescription medications and other products. A reassuring fact for supplements however is that multiple studies have shown the relative safety, or lack of significant adverse events, with supplements when used responsibly. When compared to FDA regulated prescription medications, there is significantly less morbidity and mortality associated with supplements [61]. The 2010 report from the National Poison Data System did not report any deaths due to vitamins or other dietary supplements [62].
For the average consumer, however, it remains an enigma when it comes to knowing which “fish oil” or “turmeric tablet” at the local store is the right one for them. Although the FDA is not involved in the safety and efficacy of these products, other safety organizations have arisen to provide seals of approval. These bodies include NSF International, U.S. Pharmacopeia, ConsumerLab.com, and UL. Products containing one of these organizations’ seals verify the correct ingredients listed on the label. They also provide reassurance to the consumer that the product does not contain hazardous substances. It is common practice for these manufacturers to pay for their products to be tested.
One of the organizations listed above, NSF International, has three levels of compliance and certification standards. Manufacturers of supplement products must comply with Current Good Manufacturing Practices (CGMP). These standards are clearly stated by the FDA in 21 CFR Part 111 [63]. Extensive analysis of the site, the employees, and handling of substances is done to ensure the quality and composition of ingredients. Furthermore, manufacturers can have their products certified to the NSF/ANSI 173: Dietary Supplements. Both the FDA’s 21 CFR Part 111 and the NSF/ANSI 173: Dietary Supplements are derived from the Dietary Supplement Health and Education Act of 1994 [64]. The NSF/ANSI 173: Dietary Supplements has become the American National Standard for dietary supplement products [65]. This involves verifying claims listed on the label, testing for contaminants, and being subject to routine auditing. Specifically, the NSF clearly delineates the limits of toxic substances, for example, stating that mercury content shall not exceed 0.2 ppm in raw materials and 0.02 mg/d in finished products.
Their stringent guidelines have led them to expand into sports as well. The use of dietary supplements has increased among athletes, as well as the unintended consequences of testing positive for banned substances unbeknownst to them. The NSF Certified for Sport Program expands even further, testing for banned substances listed by the World Anti-Doping Agency, NFL, and other professional leagues. The existence of these certification organizations, using guidance regulations from the FDA, provides a crucial avenue for consumers to know what they are purchasing for their personal health.
Conclusion
Majority of painful and degenerative conditions have similar underlying biochemical etiologies, typically associated with a diet-induced proinflammatory state. Through homeostasis, the body’s natural response to injury results in the activation of the inflammatory cascade to induce pain, swelling and erythema. Pain reduction is usually effective with agents such as nonsteroidal anti-inflammatory medications which act on multiple inflammatory pathways, although often have unavoidable side effects such as gastric ulceration, hypertension, stroke and myocardial infarction.
Nutritional modification with anti-inflammatory diet supplementation has been used for many centuries to decrease the inflammatory process and provide synergistic effects to medications. Many pathological conditions require specific treatments such as chemotherapy for cancer, interventions for pain, antihypertensives for high blood pressure, a diet modification treatment program should regularly be included to reduce the systemic proinflammatory state. There should be continued high quality randomized control trials to support further systematic review to provide stronger scientific data for dietary anti-inflammatory compounds to reduce pain, inflammation and improve wellness. To date there remains a need for additional studies on the combination of dietary supplements with commonly prescribed pharmaceuticals to determine safety and efficacy.
References
- Tick H. Holistic Pain Relief, Novato (CA): New World Library;2013 Nov 1.
- Herbert MS, Varley AL, Andreae SJ, et al. Association of pain with HbA1c in a predominantly black population of community-dwelling adults with diabetes: A cross-sectional analysis. Diabetic Med. 2013 Dec 1;30(12):1466-71.
- Totsch SK, Waite ME, Sorge RE. Dietary influence on pain via the immune system. Prog Mol Biol Transl Sci. 2015;131:435-69.
- You T, Nicklas BJ. Chronic Inflammation: Role of Adipose Tissue and Modulation by Weight Loss. Curr Diabetes Rev. 2006;2(1):29-37.
- Karelis AD, Faraj M, Bastard JP, et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J Clin Endocrinol Metab. 2005 Jul 1;90(7):4145-50.
- Deshmukh-Taskar PR, O?Neil CE, Nicklas TA, et al. Dietary patterns associated with metabolic syndrome, sociodemographic and lifestyle factors in young adults: the Bogalusa Heart Study. Public Health Nutr. 2009;12(12):2493-2503.
- Liese AD, Schulz M, Moore CG, et al. Dietary patterns, insulin sensitivity and adiposity in the multi-ethnic Insulin Resistance Atherosclerosis Study population. Br J Nutr 2004 Dec;92(6):973-84.
- Cintra DE, Ropelle ER, Moraes JC, et al. Unsaturated fatty acids revert diet-induced hypothalamic inflammation in obesity. PLoS One. 2012;7(1):e30571.
- McNicol E, Strassels SA, Goudas L, et al. NSAIDS or paracetamol, alone or combined with opioids, for cancer pain. Cochrane Database Syst Rev. 2005 Jan 1;1(1).
- Friedman BW, Dym AA, Davitt M, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: A randomized clinical trial. JAMA. 2015 Oct 20;314(15):1572-80.
- Kroenke K, Krebs EE, Bair MJ. Pharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviews. Gen Hosp Psychiatry. 2009 May 1;31(3):206-19.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1-49.
- Singh G. Gastrointestinal complications of prescription and over-the-counter nonsteroidal anti-inflammatory drugs: A view from the ARAMIS database. Arthritis, Rheumatism, and Aging Medical Information System. Am J Ther. 2000 Mar;7(2):115-21.
- Arulselvan P, Fard MT, Tan WS, et al. Role of Antioxidants and Natural Products in Inflammation. Oxid Med Cell Longev. 2016;2016.
- Latruffe N. Natural products and inflammation. Molecules. 2017;22:120.
- Maroon JC, Bost JW, Maroon A. Natural anti-inflammatory agents for pain relief. Surg Neurol Int. 2010;1:80.
- Elmali N, Baysal O, Harma A, et al. Effects of resveratrol in inflammatory arthritis. Inflammation. 2007;30:1-6.
- Oh Y, Kwon YS, Jung BD. Anti-inflammatory Effects of the Natural Compounds Cortex Phellodendri and Humulus japonicus on Pelvic Inflammatory Disease in Mice. Int J Med Sci. 2017;14(8):729-734.
- Soares-Bezerra, RJ, Calheiros AS, Ferreira NCdS, et al. Natural products as a source for new anti-inflammatory and analgesic compounds through the inhibition of purinergic P2X receptors. Pharmaceuticals (Basel). 2013 Apr 29;6:650-658.
- Hung HC, Joshipura KJ, Jiang R, et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004 Nov 3;96(21):1577-84.
- Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: A randomized, controlled, 74-wk clinical trial-. Am J Clin Nutr. 2009 Apr 1;89(5):1588S-96S.
- Berkow SE, Barnard ND, Saxe GA, et al. Diet and survival after prostate cancer diagnosis. Nutr Rev. 2007 Sep 1;65(9):391-403.
- Colantuoni C, Schwenker J, McCarthy J, et al. Excessive sugar intake alters binding to dopamine and mu-opioid receptors in the brain. Neuroreport. 2001 Nov 16;12(16):3549-52.
- Dietrich M, Jialal I. The effect of weight loss on a stable biomarker of inflammation, C-reactive protein. Nutr Rev. 2005 Jan 1;63(1):22-8.
- Ford ES, Bergmann MM, Kroger J, et al. Healthy living is the best revenge: findings from the European Prospective Investigation Into Cancer and Nutrition-Potsdam study. Arch Intern Med. 2009 Aug;169(15):1355-62.
- Hooper L, Harrison RA, Summerbell CD, et al. Omega 3 fatty acids for prevention and treatment of cardiovascular disease. Cochrane Database Syst Rev. 2004 Jan 1.
- Boe C, Vangsness CT. Fish Oil and Osteoarthritis: Current Evidence. Am J Orthop (Belle Mead, NJ). 2015 Jul;44(7):302-5.
- Baker KR, Matthan NR, Lichtenstein AH, et al. Association of plasma n-6 and n-3 polyunsaturated fatty acids with synovitis in the knee: the MOST study. Osteoarthritis Cartilage. 2012 May 1;20(5):382-7.
- Cleland LG, Caughey GE, James MJ, et al. Reduction of cardiovascular risk factors with longterm fish oil treatment in early rheumatoid arthritis. J Rheumatol 2006;33(10):1973-9.
- Kiecolt-Glaser JK, Belury MA, Andridge R, et al. Omega-3 supplementation lowers inflammation in healthy middle-aged and older adults: A randomized contro?lled trial. Brain Behav Immun. 2012;26(6):988-995.
- Fadus MC, Lau C, Bikhchandani J, et al. Curcumin: An age-old anti-inflammatory and anti-neoplastic agent. J Tradit Complement Med. 2017 Jul 1;7(3):339-46.
- Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res. 2012 Nov 1;26(11):1719-25.
- Mathy-Hartert M, Jacquemond-Collet I, Priem F, et al. Curcumin inhibits proinflammatory mediators and metalloproteinase-3 production by chondrocytes. J Inflamm Res. 2009;58:899-908.
- Haroyan A, Mukuchyan V, Mkrtchyan N, et al. Efficacy and safety of curcumin and its combination with boswellic acid in osteoarthritis: A comparative, randomized, double-blind, placebo-controlled study. BMC Complement Altern Med. 2018 Dec;18(1):7.
- Panahi Y, Rahimnia AR, Sharafi M, et al. Curcuminoid treatment for knee osteoarthritis: a randomized double-blind placebo-controlled trial. Phytother Res. 2014 Nov 1;28(11):1625-31.
- Kuptniratsaikul V, Dajpratham P, Taechaarpornkul W, et al. Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: A multicenter study. Clin Interv Aging. 2014;9:451.
- Kuptniratsaikul V, Thanakhumtorn S, Chinswangwatanakul P, et al. Efficacy and safety of Curcuma domestica extracts in patients with knee osteoarthritis. J Altern Complement Med. 2009 Aug 1;15(8):891-7.
- Gerrits JH, van de Wetering J, Weimar W, et al. T-cell reactivity during tapering of immunosuppression to low-dose monotherapy prednisolone in HLA-identical living-related renal transplant recipients. Transplantation. 2009 Mar 27;87(6):907-14.
- Bharti AC, Panigrahi A, Sharma PK, et al. Clinical relevance of curcumin-induced immunosuppression in living-related donor renal transplant: An in vitro analysis. Exp Clin Transplant. 2010 Jun 1;8(2):161-71.
- Ghosh SS, Gehr TW, Ghosh S. Curcumin and chronic kidney disease (CKD): major mode of action through stimulating endogenous intestinal alkaline phosphatase. Molecules. 2014 Dec 2;19(12):20139-56.
- Jiao Y, Wilkinson J, Di X, et al. Curcumin, a cancer chemopreventive and chemotherapeutic agent, is a biologically active iron chelator. Blood. 2009 Jan 8;113(2):462-9.
- C Tenore G, Daglia M, Ciampaglia R, et al. Exploring the nutraceutical potential of polyphenols from black, green and white tea infusions-an overview. Curr Pharm Biotechnol. 2015 Mar 1;16(3):265-71.
- Tipoe GL, Leung TM, Hung MW, et al. Green tea polyphenols as an anti-oxidant and anti-inflammatory agent for cardiovascular protection. Cardiovasc Hematol Disord Drug Targets 2007 Jun 1;7(2):135-44.
- Ohishi T, Goto S, Monira P, et al. Anti-inflammatory action of green tea. Antiinflamm Antiallergy Agents Med Chem 2016 Aug 1;15(2):74-90.
- Bonkovsky HL. Hepatotoxicity associated with supplements containing Chinese green tea (Camellia sinensis). Ann Intern Med 2006;144:68-71.
- Lambert JD, Sang S, Yang CS. Possible controversy over dietary polyphenols: Benefits vs risks. Chem Res Toxicol. 2007 Apr 16;20(4):583-5.
- Shara M, Stohs SJ Efficacy and Safety of White Willow Bark (Salix alba) Extracts. Phytother Res 2015;29:1112-6.
- Bonaterra GA. Anti-inflammatory effects of the willow bark extract STW 33-I (Proaktiv(®)) in LPS-activated human monocytes and differentiated macrophages. Phytomedicine, vol. 17, issue 14: 1106.
- Uehleke B, Müller J, Stange R, et al. Willow bark extract STW 33-i in the long-term treatment of outpatients with rheumatic pain mainly osteoarthritis or back pain. Phytomedicine. 2013 Aug 15;20(11):980-4.
- Biegert C, Wagner I, Ludtke R, et al. Efficacy and safety of willow bark extract in the treatment of osteoarthritis and rheumatoid arthritis: Results of 2 randomized double-blind controlled trials. J Rheumatol. 2004 Nov;31(11):2121-30.
- Oltean H, Robbins C, van Tulder MW, et al. Herbal medicine for low-back pain. Cochrane Database Syst Rev. 2014 Jan 1.
- Chung JM, Lee KH, Hori Y, et al. Effects of capsaicin applied to a peripheral nerve on the responses of primate spinothalamic tract cells. Brain Res. 1985;329:27-38.
- Holmes-McNary M, Baldwin AS, Jr Chemopreventive properties of trans-resveratrol are associated with inhibition of activation of the IkappaB kinase. Cancer Res. 2000;60:3477-83.
- Hirazumi A, Furusawa E. An immunomodulatory polysaccharide-rich substance from the fruit juice of Morinda citrifolia (noni) with antitumour activity. Phytother Res. 1999 Aug 1;13(5):380-7.
- Akihisa T, Matsumoto K, Tokuda H, et al. Anti-inflammatory and potential cancer chemopreventive constituents of the fruits of Morinda citrifolia (Noni). J Nat Prod. 2007 May 25;70(5):754-7.
- Faria A, Oliveira J, Neves P, et al. Antioxidant properties of prepared blueberry (Vaccinium myrtilus) extracts. J Agric Food Chem. 2005;53:6896-902.
- Renaud SD, de Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. The Lancet. 1992 Jun 20;339(8808):1523-6.
- Colantuoni A, Bertuglia S, Magistretti MJ, Donato L. Effects of Vaccinium Myrtillus anthocyanosides on arterial vasomotion. Arzneimittel-Forschung. 1991 Sep;41(9):905-9.
- Torri E, Lemos M, Caliari V, Kassuya CA, Bastos JK, Andrade SF. Anti-inflammatory and antinociceptive properties of blueberry extract (Vaccinium corymbosum). J Pharm Pharmacol. 2007 Apr 1;59(4):591-6.
- Donaldson MS, Corrigan JM, Kohn LT, editors. To err is human: Building a safer health system. National Academies Press;2000 Apr 1.
- Bronstein AC, Spyker DA, Cantilena LR, Green JL, Rumack BH, Dart RC. 2010 Annual Report of the American Association of Poison Control Centers? National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila). 2011 Dec 1;49(10):910-41.
- US Department of Health and Human Services, Food and Drug Administration. Guidance for industry: current good manufacturing practice in manufacturing, packaging, labeling, or holding operations for dietary supplements;small entity compliance guide. Accesses Aug. 2010;15:2011.
- Glade MJ. The Dietary Supplement Health and Education Act of 1994-focus on labeling issues. Nutrition. 1997 Nov 1;13(11-12):999-1001.
- American Institute for Standards (ANSI). (2010). Dietary supplements-NSF International Standard/American National Standard. NSF/ANSI 173-2010 American National Standards Institute, Ann Arbor U.S.
- MartÃnez-Sanz JM, Sospedra I, Ortiz CM, et al. Intended or Unintended Doping? A Review of the Presence of Doping Substances in Dietary Supplements Used in Sports. Nutrients. 2017 Oct 4;9(10):1093.