Research Article - Biomedical Research (2017) Volume 28, Issue 9
Auxiliary biological cemented femoral stem was effective in treating elderly patients with intertrochanteric fracture
Xiangxun Cao*, Xiangdi Kong and Aimin LiDepartment of Orthopedics, Linyi Central Hospital, Shandong, PR China
Accepted on February 4, 2017
Abstract
Objective: Joints displacement has been introduced in treating intertrochanteric fracture. However, the studies on the treatment of femoral prothesis stem in elderly patients are very rare. This study aimed to observe the curative effect of auxiliary biological cemented femoral stem in treating elderly patients with unstable intertrochanteric fracture.
Methods: From January 2012 to January 2016, 85 elderly patients with intertrochanteric fracture in our department were randomly divided into two groups (control group, n=42 and observation group, n=43), who were treated with auxiliary biology cemented femoral stem replacement and biological artificial hip replacement with lengthened handle, respectively. The related clinical data were collected and compared.
Result: The average age was 79.6 years old. The prosthesis was fixed according to the Engh standard in all patients. No difference was found on the operation time between two groups (P>0.05). Observation group had significantly less bleeding volume during and after operation (P<0.05). The ambulation time in observation group was significantly shorter than that in the control group (P<0.05). Harris scores and VAS was comparable before surgery (P>0.05), which in observation group were all significantly higher than those in control group at 1, 3, and 6 months after surgery (P<0.05).
Conclusion: Treating intertrochanteric fracture elderly patients with auxiliary biological cemented femoral stem prosthesis is good for initial fixation, early walking with load, and long-term bone ingrowth, which can also greatly improve the hip joint function and patients’ life quality.
Keywords
Intertrochanteric fracture, Arthroplasty, Replacement, The elderly, Therapeutic efficacy.
Introduction
Coming with the aggravation of the aging problem, the number of intertrochanteric fracture in elderly patients is continuously increasing in China. This fracture is always complicated with osteoporosis, and the fracture stability is very poor; the fracture is also complicated with cardiopulmonary embolism, cerebral embolism, diabetes mellitus, poor cardiopulmonary function, and short life expectancy. Therefore, the disability and fatality rate are relatively high. Currently, joints displacement has been mostly adopted in the treatment of intertrochanteric fracture in elderly patients [1,2]. However, the studies on the clinical application of femoral prothesis stem, especially the proximal femoral osteoporosis in elderly patients are very rare. Thus, our paper aimed to investigate the therapeutic efficacy of auxiliary biological cemented femoral stem in treating elderly patients with unstable intertrochanteric fracture.
Patients and Methods
Patients
The patients with intertrochanteric fracture who have received prothesis replacement in our hospital from January 2012 to January 2016 were enrolled. The patients were divided into observation group and control group by the random number table method (observation group, n=43 and control group, n=42). The differences on sex, age, fracture type, injury cause, joint functions, complications and other general information between two groups were not statistically significant (P>0.05). This study was approved by the local ethical committee, and all patients signed the informed consent form.
Inclusion criteria were described as follows: 1) in accordance with the diagnostic criteria of intertrochanteric fracture; 2) with the age of no less than 66 years old; 3) with the indication of artificial hip joint replacement; 4) normal walking without or with single stick before intertrochanteric fracture; 5) Evans- Jensen type III-V fracture complicated with many underlying diseases, inappropriate for long-term bedridden after the surgery or complicated with serious osteoporosis; or Evans-Jensen type II fracture with the contraindication of fracture reduction and internal fixation. Patients with new or old cerebral thrombosis or Evans-Jensen type I fracture, or cardiac insufficiency, or pathological fracture of femoral neck or complicated with coagulation disorders and mental diseases were excluded.
Surgery
The patients in control group were treated with biological type lengthened handle artificial hip replacement, while observation group were treated by bone cement auxiliary ordinary biology stem of artificial hip joint replacement. Subarachnoid block combined epidural anesthesia was adopted for all patients, patients were required to keep side-lying position and hip postlateral approach was used in their treatment. When cutting the femoral neck, since this fracture was always complicated with the fracture of the base in femoral neck, be sure to keep the greater trochanter, lesser trochanter and fascial fiber attached. Use a smaller drill to ream to avoid injuring bone cortex. Make an incision in proximal femoral medullary cavity. In the observation group, the distal medullary cavity was usually spacious, so it should only consider filling the proximal prosthesis and determine the type of the prosthesis. Set the cement plug 1 cm further than distal prosthesis; during the earlier period of wire drawing, 5 to 10 ml bone cement should be injected into the distal end of medullary cavity, about 1 to 2 min before its concretion, try to implant the prosthesis along in the middle position, hammer to implant it with low strength when necessary. Long specialized reamer was used in control group, and biological type lengthened handle was selected in this group for implantation. Take proximal femoral prosthesis as a support for broken bone block reduction, use steel wire for fixation to re-organize stable femoral calcar and greater trochanter, for the osteoporosis patients, the steel wire could also be used directly to suture the fracture block of greater trochanter. For the missing bone lump and spaces around femoral neck, cancellous bone inside femoral head could be pressed and used for filling. After the bone cement became solidified, install the head and neck of test mould, and reset; after testing the degree of tightness and equal limb length, implant the prosthesis for reduction. Operation time, bleeding volume during operation, postoperative blood loss, the total operative blood loss and ambulation time between the two groups were compared.
Postoperative treatment
After the surgery, routinely use low molecular heparin sodium for anticoagulation, use antibiotics to prevent infection, remove the drainage tube 48 h after the surgery, help the patients with their isometric limb muscle contraction practice and limb function exercise to prevent the formation of deep venous thrombosis within 1 to 3 days postoperatively. As a result of the postoperative management, there were no patients in this group suffered deep venous thrombosis after the surgery. Based on the preoperative evaluation of hip fracture in elderly patient, it should be paid continuous attention to prevent the complications [3,4], prepare the patients’ conditions and handle the situations continuously. According to the patients’ operation status, the patients were required to walk with crutches with no heavy burden within 3 days to 1 week postoperatively, part weight-bearing of affected limbs was permitted for patients 3 weeks after the surgery, and full weight-bearing was allowed 3 months after the surgery. The patients with serious osteoporosis should appropriately delay 1 to 2 weeks of their weight-bearing time.
Follow-ups
During follow-ups, Harris score, VAS and X-ray examinations were collected in all patients. Harris score of hip joint function before the surgery, 1, 3, 6 months and 1 year after the surgery, and VAS for grading hip pain were introduced. Also, the X-ray film could be used to observe whether the prosthesis shifted, the contact condition of prosthesis and femur; and the Engh standard [5] could be used to judge biomechanical stability of the prosthesis, which were divided into bone ingrowth stability, fiber ingrowth stability and instability (loose).
Statistical analysis
SPSS 18.0 statistical software (SPSS, Inc., Chicago, IL, USA) was used. The continuous data were expressed as mean ± standard deviations, and the differences were tested using independent student-t test. The categorical data were compared using chi-square test. P value<0.05 was considered to be statistically significant.
Result
Demographical and clinical data
There were 36 male patients and 49 female patients, and their age ranged from 66 to 98 years old with the average age of 79.6. For the fracture site, there were 46 cases of left-side intertrochanteric fracture and 39 cases of right-side intertrochanteric fracture. For the injury cause, there were 70 cases of falling down injury while walking and 15 cases of crush injury by non-motor vehicle.
According to Evans-Jensen classification of intertrochanteric fracture, there were 8 cases of type II, 42 cases of type III, 22 cases of type IV and 13 cases of type V. The time interval from injury to surgery ranged from 3 h to 12 d with an average time of 5.5 d. X-ray plain films of bilateral hip and CT three-dimensional reconstruction were conducted before surgery. All the cases were complicated with osteoporosis. Among the 85 cases, there were 35 cases complicated with Coronary Heart Disease (CHD), 40 cases complicated with hypertension, 18 cases complicated with diabetes, 14 cases of chronic bronchitis and emphysema, 15 cases of hypoproteinemia and anaemia, 14 cases of old cerebral infarction and 2 cases of renal insufficiency. There were 48 cases with two or more than two complications.
Therapeutic efficacy
Before surgery, the difference on Harris scores between the two groups was not statistically significant (P>0.05), while at 1, 3, and 6 months after surgery, Harris scores in observation group were all significantly higher than those in the control group and the differences were statistically significant (P<0.05) (Table 1).
| Group | Before surgery | 1 month after surgery | 3 months after surgery | 6 months after surgery |
|---|---|---|---|---|
| Observation group | ||||
| (n=45) | 25.32 ± 5.10 | 63.35 ± 6.23 | 75.55 ± 7.36 | 89.21 ± 7.54 |
| Control group | ||||
| (n=44) | 25.26 ± 5.24 | 54.64 ± 5.83 | 60.85 ± 6.34 | 78.12 ± 8.38 |
| t value | 0.19 | 5.15 | 6.15 | 5.12 |
| P value | >0.05 | <0.05 | <0.05 | <0.05 |
Table 1. Harris score before surgery, at 1, 3 and 6 months after surgery between two groups.
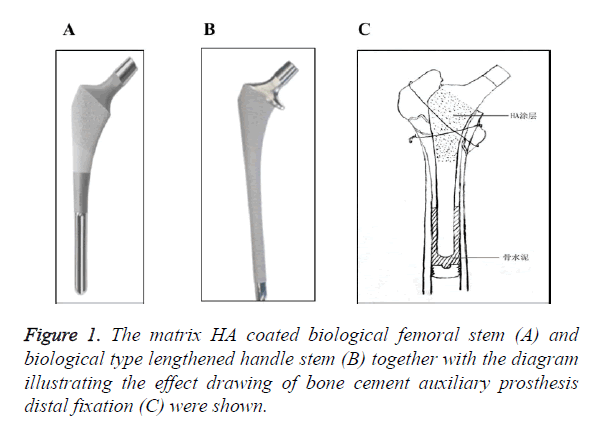
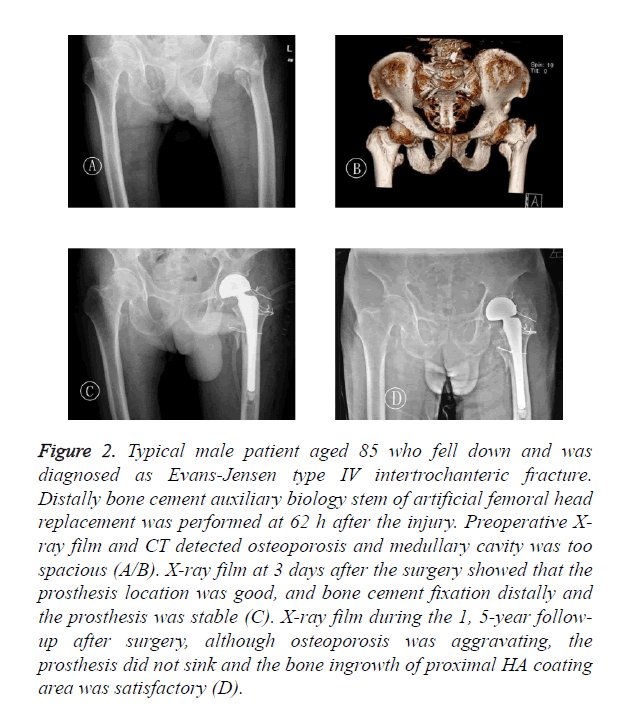
All patients in observation group have received the follow-up for 6 to 34 months after the surgery, with an average time of 24 months. At 1 year after the surgery, the function of hip joint had greatly improved in all patients. According to the latest follow-up (more than 1 year after the surgery), new bone growth was observed between the femoral prosthesis and endosteum, and there were no resorption (osteolysis) and formation of radiolucent line. According to Engh standard, all patients had received bony fixation. There were no neurovascular injury, infection, fracture, loosening or dislocation of prosthesis, pain in non-femoral region and host reactions of the transplantation occurred in any patients. After discharge, 3 cases of patients died of cardio-pulmonary failure, 1 case died of stroke, 1 case died of other internal medical disease (with unknown death cause). The prosthesis was shown in Figures 1A and 1B, effect drawing of the operation was shown in Figure 1C, and typical case was shown in Figure 2.
Figure 2. Typical male patient aged 85 who fell down and was diagnosed as Evans-Jensen type IV intertrochanteric fracture. Distally bone cement auxiliary biology stem of artificial femoral head replacement was performed at 62 h after the injury. Preoperative X-ray film and CT detected osteoporosis and medullary cavity was too spacious (A/B). X-ray film at 3 days after the surgery showed that the prosthesis location was good, and bone cement fixation distally and the prosthesis was stable (C). X-ray film during the 1, 5-year followup after surgery, although osteoporosis was aggravating, the prosthesis did not sink and the bone ingrowth of proximal HA coating area was satisfactory (D).
Safety
The comparison of operation time between two groups has no statistical significance (P>0.05); for the amount of bleeding during operation, postoperative blood loss and the total operative blood loss, the amount of observation group is significantly less than that of the control group, the differences are statistically significant (P<0.05); for the ambulation time, the time of observation group was significantly shorter than that of the control group, the difference has statistical significance (P<0.05) (Table 2). In observation group, there were no patients with toxic reaction, sudden drop of blood pressure, nausea, discomfort and other manifestations during treatment. And during the hospitalization period, there were no infection, bedsore, deep venous thrombosis, fat embolism and other complications in the two groups of patients.
| Group | Operation time, min | Bleeding volume during operation, ml | Postoperative blood loss, ml | Total operative blood loss, ml | Ambulation time, d |
|---|---|---|---|---|---|
| Observation group | |||||
| (n=45) | 71.32 ± 12.30 | 182.35 ± 30.23 | 104.55 ± 25.36 | 290.47 ± 32.50 | 3.21 ± 0.54 |
| Control group | |||||
| (n=44) | 70.26 ± 11.24 | 196.64 ± 42.13 | 126.85 ± 27.34 | 324.29 ± 38.33 | 9.12 ± 0.98 |
| t value | 2.83 | 2.05 | 3.15 | 3.98 | 5.12 |
| P value | >0.05 | <0.05 | <0.05 | <0.05 | <0.05 |
Table 2. Related clinical data were collected and compared between two groups.
Discussion
The incidence of hip fracture has increased year by year. According to the report of Miyamoto RG et al. there were about 1.7 million suffering from hip fracture in the globe range, and the mortality rate was ranging from 14% to 36% per year [6]. For that the conservative treatment usually takes longer time and brought several complications, the life quality of patients is very poor and surgical treatment becomes the first choice for the patients [1-4]. Due to some causes like osteoporosis, poor internal fixation or unstable fracture, using internal fixation would cause fracture nonunion or malunion, lag screw cut out femoral head, ischemic necrosis of the femoral head, traumatic arthritis, etc. [7]. Most scholars suggest adopting internal fixation for young patients with good bone condition and stable fracture, while using joint replacement for elderly patients with osteoporosis and unstable fracture [1,2], considering that the treatment of joint replacement would restore the limb length quickly, provide good stability immediately, help patients get out of bed in early period after surgery and reduce the complications in peri-operative period [8].
The intertrochanteric fracture could be caused by indirect or direct violence, and 90% patients of intertrochanteric fracture have low-energy injury. Falling down and osteoporosis are their main injured mechanism [9]. The elderly intertrochanteric fracture patients have weakened support for the prosthesis, moreover, the implant position and initial stability of artificial hip joint prosthesis are poor [10].
There are still some disadvantages of ordinary femoral stem prosthesis. 1. For bone cement prosthesis, since the bone cement could penetrate the broken ends at the fractured ends, it could directly prevent fracture healing. Hardy et al. [1] reported that bone cement with polymerization heat was sufficient to inactivate mesenchymal stem cells so as to affect the fracture healing, which went against the mid and long-term stability; Zhang et al. [12] pointed that the incidence rate of bone cement prosthesis complications was up to 47%, the toxicity of bone cement increased the risk of cardiopulmonary and vascular complication, while enhancing perfusion increased the risk of fat embolism. 2. Biological type femoral prosthesis stem avoided the toxin effect, however, the current design of biological prosthesis stem could not meet the various shapes of medullary cavities, especially for the unusual spacious femoral medullary cavity due to osteoporosis, that usually its near-end expanded to the thinner cortex while its distal end still kept unstable.
Currently, choosing biological type lengthened handle for treating elderly intertrochanteric fracture patients is relatively common [13,14], for relying on the lengthened handle could increase the contact area; however, since the elderly patients usually suffered osteoporosis and had spacious medullary cavities, their proximal femoral fractures were unstable and lacked rotary control, the rotation of the prosthesis inside medullary cavity was not stable; therefore, many osteoporosis patients still could not receive initial stability, this treatment could easily cause anteversion angle disappearing after reduction, joint dislocation and loosening, and postoperative pain, which seriously influenced the curative effect. Aiming to the above problems, we designed and used the distal bone cement auxiliary biology stem for fixation, used wire binding for fracture reduction combined femoral stem biological fixation at the near end, as the treatment for unstable intertrochanteric fracture in elderly patients.
The prosthesis was matrix HA coated biological femoral stem with almost 1/3 coating, the distal end of the prosthesis was smooth (Figure 1). Use bone cement at the distal end of femoral stem to form an about 3-4 cm fixed cement column after implantation, which could receive the immediate effect of rigid fixation, and solve the unstable problem when turning inward and outward, and rotating. On the on hand, it could reduce the systemic reaction upon bone cement prosthesis, and had little interference for elderly intertrochanteric fracture patients with poor compensation ability; on the other hand, it did not require over-sized prosthesis for stability. Fixing the fracture block of proximal greater trochanter and lesser trochanter around the femoral stem for reduction, is good for keeping proximal bone mass, and has less invading towards the proximal femoral trochanteric bones, the stability of prosthesis is good for healing of intertrochanteric fracture. The good stability of prosthesis helps patients for their early ambulation, reduced the occurrence of complications during peri-operative period, and it is also good for biological prosthesis bone ingrowth, thus to improve the curative effect. Wang et al. [15] reported that biological lengthened handle would increase trauma as well as the amount of bleeding during operation, and prolong the ambulation time. In this study, the amount of bleeding during operation, postoperative blood loss and the total operative blood loss of observation group was significantly less than that of the control group, the differences were statistically significant (P<0.05). For patients with serious osteoporosis, thinner cortex and spacious medullary cavity, we think, it is difficult for biological type lengthened handle to receive rotational stability, while using distal bone cement auxiliary ordinary biology stem for fixation has significant advantage.
Taken together, choosing bone cement auxiliary biological femoral stem prosthesis for joint replacement as individualized treatment for intertrochanteric fracture in elderly patients, especially for patients with serious osteoporosis, has good initial stability and exact curative effect, which will definitely benefit such patients.
Conflict of Interest
The authors confirm that this article content has no conflict of interest.
References
- Zhang S, Chen KF, Zhang CL. Cemented bipolar femoral head arthroplasty in treatment of senile intertrochanteric fracture with cardiopulmonary diseases. Chinese J Trauma 2015; 31: 531-535.
- Tong PJ. Correctly understand the treatment of joint replacement for intertrochanteric fracture. Chin J Traum 2015; 31: 3-6.
- He ZY, Di ZL, Zhang JH. Prevention and treatment for complications in peri-operative period of hip replacement in patients eighty years of age and older. Chin J Geriatr 2008; 27: 435-438.
- Gao H, Wang BJ, Zhao L. Analysis on complications and death causes of intertrochanteric fracture in peri-operative period. Chin J Orthopaed 2015; 35: 819-824.
- Engh CA, McAuley JP, Sychterz CJ. The accuracy and reproducibility of radiographic assessment of stress-shielding. A postmortem analysis, Bone Joint Surg (Am) 2000; 82: 1414-1420.
- Miyamoto RG, Kaplan KM, Levine BR. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. Am Acad Orthop Surg 2008; 16: 596-607.
- Liu ZT, Pan XY, Wang Q. Internal fixation failure in treating intertrochanteric fracture with hip replacement. Chin J Orthop 2011; 31: 784-788.
- Zhang XM, Zhang PX, Chen JH. Analysis and countermeasure of hospitalized death cases with around-the-hip fractures of traumatic orthopedics. Chin J Orthop Trauma 2014;16: 679-683.
- Liu Q. Treatment of osteoporotic and intertrochanteric fractures. Chin J Orthop 2014; 34: 92-95.
- Sidhu AS, Singh AP. Total hip replacement as primary treatment of unstable intertrochanteric fractures in elderly patients. Int Orthop 2010; 34: 789-792.
- Hardy DC, Frayssint P, Guihem A. Bonding of hydroxyapatite-coated femoral prostheses. Bone Joint Surg Br 1991; 73: 732-740.
- Zhang B, Chiu KY, Wang M. Hip arthroplasty for failed internal fixation of intertrochanteric fractures. J Arthropl 2004; 19: 329-333.
- Lv L, Niu XB, Zhang JJ. The treatment of elderly intertrochantor fracture by biological type lengthened handle artificial hip replacement. Chin J Orthop 2012; 32: 637-641.
- Guo QJ, Wang L, Zhen XZ. Mid-term curative effect analysis on treating the unstable intertrochanteric fracture in elderly patients with biological type lengthened handle artificial femoral head replacement. Chin J Prim Med Pharm 2015; 22: 989-992.
- Wang L, Chen HF, Zhen XZ. Treating unstable intertrochanteric fracture in elderly patients with cementless hemiarthroplasty. Chin J Orthop 2012; 32: 642-647.