Research Article - Biomedical Research (2017) Volume 28, Issue 5
Viral respiratory tract infections and their correlation with clinical presentations and outcomes among young children attending emergency department of tertiary care hospital in China
Jun-Li Dang1*#, Jun-Jun Zhao2#1Department of Nursing, Zhumadian Central Hospital, No.747 Zhonghua Road, Zhumadian, Henan, PR China
2Department of Pathology, Dalian Municipal Central Hospital Affiliated of Dalian Medical University, PR China
#These authors contributed equally to this article
Accepted date: October 28, 2016
Abstract
Purpose: Besides advent of genome detection for respiratory viral infections by multiplex PCR, the correlation between individual viruses with clinical presentations and outcomes is unclear. We conducted a retrospective monocentric study in order to evaluate virus specific clinical correlation in children attending emergency department.
Methodology: A total 411 children aged<18 years during 5 winter seasons were evaluated for presence of viral infection by using multiplex PCR. Patients were sampled within 48 hours of their presentation to emergency department. Individual viruses were correlated with clinical presentations and clinical outcomes by using multivariate logistic regression analysis.
Results: Results of multiplex PCR demonstrated the presence of virus in 312/411 (76%) patients where single virus infections were identified in 256/312 (82%) patients and multiple (mixed) virus infections were found in 56/312 (18%) patients. Respiratory Syncytial Virus (RSV) and Human Rhinovirus (HRV) were more prominent among young children but only the presence of RSV virus was significantly higher among young children (<3 years) as compared to older (3-18 years). As most of the viral infections share common clinical presentations therefore discrimination of ARTI on the basis of signs and symptoms is not possible. HRV was found to be associated with bronchodilators (OR: 2.5) and corticosteroid treatment (OR: 4.2) as well as severe respiratory complications (OR: 4.7). RSV was found to be correlated with oxygen therapy (OR: 4.7) and inversely correlated with respiratory complications.
Conclusions: Most of the children presenting to emergency department had single virus infections with RSV and HRV. Presenting clinical presentations does not discriminate four virus groups while infections with RSV and HRV portended heavy burden of morbidity in our study.
Keywords
Respiratory infection, Polymerase chain reactions, Respiratory syncytial virus, Human rhinovirus, Clinical outcomes.
Introduction
Acute Respiratory Tract Infections (ARTIs) are most common problems among children, comprising as many as 50% of all illnesses in children less than 5 years old and 30% in children aged 5-12 years. ARTIs describe all infections of respiratory tract range from common and mild upper RTI to more severe Lower Respiratory Tract Infections (LRTIs) [1]. It has been estimated that out of total deaths among children having age less than five years, 19% (over 2 million) fatal cases occur due to ARTIs [2,3]. Bronchiolitis and pneumonia precipitated by viruses primarily contributed to these deaths [2]. Viruses are major etiological factors of ARTIs that may infect throughout the respiratory tract but do not necessarily always produce clinical manifestations. Furthermore, several other factors i.e. environmental (pollution, humidity), family (poverty, birth order) and medical circumstances (malnutrition, chronic lung disease) play a pivotal role to initiate clinical signs and symptoms of ARTIs [4].
Advent of genome detection systems such as Polymerase Chain Reaction (PCR) and micro-array technology provides sensitive and better identification of single and mixed viral infections [5]. Besides of these advancements, viral correlation with respiratory infections among paediatric population is still unclear. Two large scale studies evaluating virus association with respiratory illness failed to demonstrate accurate correlation due to utilization of less sensitive virus detection methods i.e. viral culturing and immunofluorescence techniques. Despite of less sensitivity, these methods are also unable to detect non-culturable or mixed viral infections [6,7]. Three population-based studies estimated prevalence of ARTIs as more than 21% in paediatric emergency department suggesting high burden of viral ARTIs in children. But this burden can’t be considered as true estimation because authors did not evaluate Human Rhinovirus (HRV) in their studies that may underestimate the true burden of viral ARTIs [8-10]. More recently, HRV evaluation was considered in several studies but viral correlation with infection is hampered by the differences in age and symptoms among enrolled participants [11,12] as well as inclusion of cases during influenza pandemic in these studies [13,14]. More recently, Gooskens et al. identified respiratory viruses in 82% of children with age<18 years presented to the emergency department in Netherland [5]. Besides these efforts, burden of respiratory viruses and their correlation with disease spectrum is still unclear and there is a dire need to evaluate such correlation in order to reduced related morbidity and mortality.
In this context, we conducted a retrospective monocentric study in order to estimate the burden of ARTIs among children attending the emergency department by using multiplex PCR and to determine virus specific clinical correlation in young children. Current study is the first description of estimation of ARTIs in children in China with larger sample size.
Methodology
Study design and setting
A retrospective cohort study was conducted among children (age<18 years) during winter seasons attending emergency department of Zhumadian Central Hospital, Henan China, from 2009 to 2013 (5 years).
Clinical and molecular diagnosis
Diagnosis of ARTIs was based on physician documentation of patients during their presentation to the emergency department. Type of respiratory viruses among enrolled cases were evaluated by respiratory virus multiplex PCR. Specimens from nasopharynx, throat, nose or trachea were taken within 48 hours of hospital presentation and subjected to nucleic acid extraction by a total nucleic acid kit (MagnaPure LC, Roche, Germany). Fixed amount of equine arteritis virus and phocid herpes virus were served as RNA and DNA internal controls, respectively. Whole procedure for viral specimen’s collection and detection including nature and type of primers, probes and amplification used in current study were described by Leones et al. [15]. Virus identified in current study were Human Rhinovirus (HRV), Respiratory Syncytial Virus (RSV), Human Coronavirus (HCoV), Influenza virus A and B (FLU), Para Influenza virus 1, 2, 3 and 4 (PIV), Human Metapneumovirus (HMPV), Human Adenovirus (HAdV) and Human Bocavirus (HBoV).
Data collection
All the data was collected by using structured data collection form. Patients’ demographics and signs/symptoms were recorded within 48 hours of hospital presentation. Adverse clinical outcomes including hospital admission, severe respiratory complications and mortality were also recorded within ≤ 7 days of hospital presentation. Data on laboratory (CReactive Protein (CRP) and white blood cell count (WBCs)) and pulmonary imaging that were available within 96 hours of hospital presentation were used for the study purpose. Pulmonary imaging findings were served to evaluate presence of LRTIs (presence of infiltrates in alveoli and peribronchi, hyperinflation and interstitial opacities). Bacteriological results by PCR and by sterile or non-sterile culturing techniques were also recorded.
Definitions
Absence of serious bacterial infections were described by cutoff values of CRP (<35 mg/l) and WBCs (<15 × 109). Adverse clinical outcomes included all pre-defined outcomes that occurred within ≤ 7 days of hospital presentation. Severe respiratory complications were termed as presence of apnea, initiation of respiratory intubation or Apparent Life Threatening Events (ALTEs). ALTEs were termed as children’s unusual breathing behaviour observed as possibly life threatening by their parents or caretakers. Fever>38.5°C, wheezing, pharyngitis, rhinitis, cough, crepitations, tachypnea or dyspnoea were considered as virus-associated symptoms. Dyspnoea was defined by the presence of laboured breathing, chest wall retractions, moaning or flaring. Tachypnea was referred to ≥ 60 beats/min (age<2 months), ≥ 50 beats/min (age 2-12 months) and ≥ 40 beats/min (≥ 12 months). Other definitions used in current study include premature birth (gestational age less than 37 weeks) and bronchial hyperactivity (bronchoconstriction due to contact with stimuli).
Ethical approval
Current study followed principles of World Medical Association`s Declaration of Helsinki. Protocol of study and final version of manuscript is approved by research ethical committee of Zhumadian Central Hospital (Reference No. APP/RECSU/R34532). Need of consent form was waived by ethical committee due to retrospective nature of the study. All the efforts were made to avoid patient’s identification during study process, by anonymization of patient`s identifiable data.
Statistical analysis
Continuous and categorical data were presented as mean (SD) and frequencies (percentages), respectively. Data were analysed by using Chi-square test, Fisher’s exact test, student ttest and Mann-Whitney U-test, where appropriate. A comparison of categorical variables between different virus groups was performed by logistic regression. Multivariate analysis was adjusted for gender, age, history and underlying chronic disorders by forward stepwise selection method. A two sided p-value and confidence interval were calculated where P<0.05 were considered as significant. All the data were analysed by using SPSS version 20.0.0.
Results
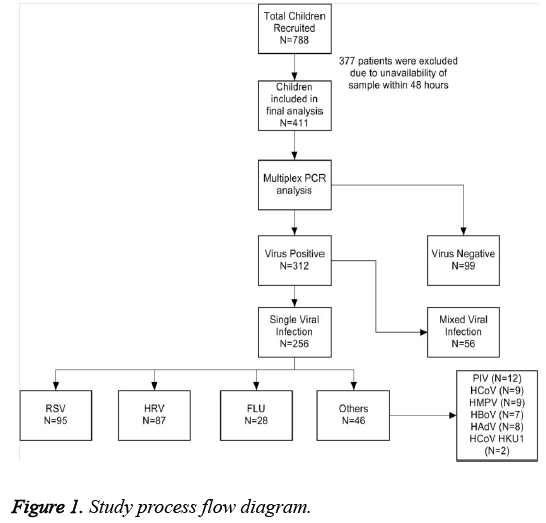
A total 788 patients attended emergency department with ARTIs during five winter seasons from 2009 to 2013. A total 377 patients were excluded from the study due to unavailability of sample of patients within 48 hours of their presentation to the hospital. Finally, 411 patients were included in the study. Out of the total patients, 374 (91%) patients had age<3 years while 37 (9%) were 3-18 years old. Results of multiplex PCR demonstrated the presence of virus in 312/411 (76%) patients where single virus infections were identified in 256/312 (82.1%) patients. Multiple (mixed) virus infections were observed in 56/312 (17.9%) patients. Out of 256 patients with single virus infections, RSV was found in 37% of patients while HRV and FLU were observed in 34% and 11% of children, respectively. Viral distribution among 256 patients is described in Figure 1. In order to make accurate and robust comparison between different viruses, we aggregated PIV, HCoV, HMPV, HBoV and HAdV into a single group name “others”, as the number of cases with these viruses were very small resulting is weak power of statistical analysis. By this way, group “others” constitutes 46 (18%) of 256 patients with single viral infections. We did not analyse mixed virus infections in our study due to less number of patients (N=56) and difficulty to establish clinical relevancy. A comparison describing distribution of viruses between young children and older children are presented in Table 1. We found that the prevalence of single virus infection, RSV, HRV and FLU was higher in young children as compared to older cases but statistically significant difference was only observed for RSV and HRV. On the other hand, prevalence of mixed virus infections and other viruses were higher in older age groups than younger children. Among all viruses, RSV and HRV were more prominent while the prevalence for FLU was very low in present study (Table 1).
| Total (N=312) | Children with age <3 years (N=281) | Children with age 3 to 18 years (N=31) | P-value | |
|---|---|---|---|---|
| Single virus infection | 256 (82.1%) | 237 (84.3%) | 19 (61.4%) | 0.061 |
| Mixed viral Infection | 56 (17.9%) | 49 (17.4%) | 7 (22.6%) | 0.093 |
| RSV | 95 (30.4%) | 91 (32.4%) | 5 (16.1%) | 0.013 |
| HRV | 87 (27.9%) | 83 (29.5%) | 4 (12.9%) | 0.034 |
| FLU | 28 (9.0%) | 26 (9.3%) | 2 (6.5%) | 0.623 |
| Others | 46 (14.7%) | 33 (11.7%) | 13 (41.9%) | <0.001 |
Table 1: Virus distribution among two age groups included in current study.
Baseline characteristics and clinical outcomes of the study participants were compared based upon viral distribution. We only included younger age group (<3 years) for this analysis. Children with age 3 to 17 years were excluded from the analysis due to age related confounding differences that may affect the statistical power of the study. Baseline characteristics of the studied participants are described in Table 2. Patients having FLU and others infection were older than RSV and HRV, but difference was statistically insignificant. Males were found to be most affected population in HRV and male predominance was only significant when compared with FLU (P=0.035). All others baseline characteristics were equally distributed among four virus groups. As we found proportional differences of these baseline characteristics in different virus groups, therefore possible considerations are require during statistical comparison in order to avoid the confounding effects of these characteristics.
| Total (N=256) | RSV (N=95) | HRV (N=87) | FLU (N=28) | Others (N=26) | |
|---|---|---|---|---|---|
| Age (months) | 10.8 (5.8) | 8.7 (7.1) | 9 (6.2) | 12.3 (4.4) | 14.1 (6.8) |
| Male | 162 (63.3%) | 61 (64.2%) | 70 (80.5%) | 12 (42.9%) | 19 (73.1%) |
| Premature Birth | 28 (6.3%) | 12 (12.6%) | 9 (10.3%) | 3 (10.7%) | 4 (15.4%) |
| BHR history | 26 (5.9%) | 9 (9.5%) | 10 (11.5%) | 4 (14.3%) | 3 (11.5%) |
| CCD | 18 (4.1%) | 7 (7.4%) | 8 (9.2%) | 2 (7.1%) | 1 (3.8%) |
| CPD | 3 (0.7%) | 0 | 3 (3.4%) | 0 | 0 |
| CID | 8 (1.8%) | 2 (2.1%) | 1 (1.1%) | 3 (10.7%) | 2 (7.7%) |
| Antibiotics | 110 (24.9%) | 48 (50.5%) | 41 (47.1%) | 9 (32.1%) | 12 (46.2%) |
| Bronchodilators | 60 (15.9%) | 31 (32.6%) | 30 (34.5%) | 6 (21.4%) | 3 (11.5%) |
| Steroids | 74 (16.8%) | 22 (23.2%) | 41 (47.1%) | 6 (21.4%) | 5 (19.2%) |
| Oxygen Therapy | 136 (30.8%) | 71 (74.7%) | 55 (63.2%) | 2 (7.1%) | 8 (30.8%) |
| CRP ≥ 35 mg/l | 71 (16.1%) | 31 (32.6%) | 31 (35.6%) | 5 (17.9%) | 4 (15.4%) |
| WBC ≥ 15×109/l | 74 (16.8%) | 29 (30.5%) | 33 (37.9%) | 6 (21.4%) | 6 (23.1%) |
| LRTI | 109 (24.7%) | 51 (53.7%) | 42 (48.3%) | 7 (25%) | 9 (34.6%) |
| Hospitalization | 180 (40.8%) | 73 (76.8%) | 66 (75.9%) | 22 (78.6%) | 19 (73.1%) |
| SRC | 37 (14.5%) | 8 (8.4%) | 21 (24.1%) | 3 (10.7%) | 5 (19.2%) |
| Apnea | 19 (4.3%) | 6 (6.3%) | 11 (12.6%) | 1 (3.6%) | 1 (3.8%) |
| Intubation | 21 (4.8%) | 3 (3.2%) | 12 (13.8%) | 2 (7.1%) | 4 (15.4%) |
| ALTE | 14 (3.2%) | 6 (6.3%) | 8 (9.2%) | 0 | 0 |
| Mortality | 0 | 0 | 0 | 0 | 0 |
Table 2: Baseline Characteristics and outcomes among children (<3 years) with single virus infection.
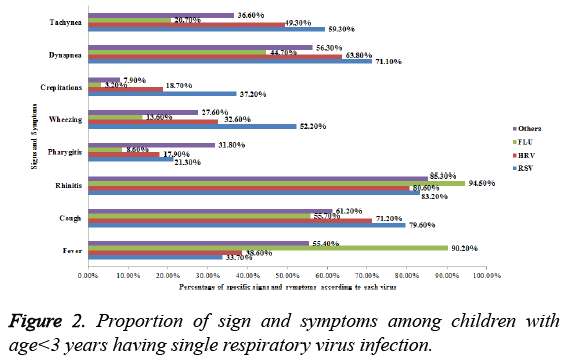
Signs and symptoms at the time of presentation to the emergency department are described in Figure 2. Fever and rhinitis was more common in FLU while cough, wheezing, dyspnoea and tachypnea were more abundant signs and symptoms in patients with RSV infection. Among patients with RSV infection, presence of cough was significantly higher as compared to those having infection with FLU and others (P=0.031 and 0.024, respectively). Similarly, crepitations were frequently occurred in RSV infection as compared to HRV (0.011). Moreover, patients with RSV infection also had high prevalence of dyspnoea and tachypnea as compared to patients FLU infection (0.031 and 0.036, respectively). The presence of fever was significantly higher among patients with FLU virus infection, as compared to those with RSV and HRV infection (P<0.001 and P<0.001, respectively).
Clinical outcomes of patients in different virus groups were compared (Table 2). Bacteriology findings in our study revealed no potential bacterial infections among virus groups. PCR did not identify any atypical bacteria among studied participants. On the other hand, sterile and non-sterile bacterial culturing found 1 positive result in RSV and HRV groups, respectively. Additionally, high levels of CRP and WBC were statistically insignificant among different virus groups suggesting absence of any serious bacterial infection. Use of antibiotics was equally distributed among virus groups that further support our assumption of absence of bacterial infection. Hospitalization was observed in more than 70% population in each group and we found no significant difference in hospital admission. Occurrence of apnea, intubation and ALTE were also equally distributed among different virus groups. Fortunately, there was no mortality in our study.
Need of bronchodilators, steroids, oxygen therapy and occurrence of severe respiratory complications were not equally distributed among virus groups. These variables were subjected to multivariate analysis after adjusting age, sex and underlying diseases (stepwise) in order to determine association of each virus group with these variables (Table 3).
| Odds ratio | 95% CI | P-value | ||
|---|---|---|---|---|
| Bronchodilators | HRV overall | 2.5 | 1.5-5.9 | 0.034 |
| HRV vs. Others | 5.5 | 2.6-8.4 | 0.001 | |
| Steroids | HRV overall | 4.2 | 2.4-6.3 | 0.025 |
| HRV vs. RSV | 3.8 | 2.1-7.6 | 0.031 | |
| Oxygen therapy | RSV overall | 4.7 | 3.2-8.6 | 0.015 |
| FLU overall | 0.3 | 0.2-1.3 | 0.017 | |
| RSV vs. FLU | 31.5 | 21.3-89.7 | <0.001 | |
| RSV vs. Others | 2.8 | 1.4-5.7 | 0.028 | |
| HRV vs. FLU | 17.6 | 8.7-33.2 | <0.001 | |
| Severe respiratory complication | HRV overall | 4.7 | 3.2-8.8 | 0.032 |
| RSV overall | 0.41 | 0.22-0.45 | 0.05 | |
| HRV vs. RSV | 6.4 | 2.7-12.6 | 0.026 |
Overall comparison refers to comparison of specified virus with rest of the virus types
Table 3: Correlation of clinical outcomes and type of respiratory viruses according to multivariate logistic regression.
Among treatments, use of antibiotics was equally distributed in virus groups while need of bronchodilators, steroids and oxygen therapy varies significantly among virus groups. The need of bronchodilators was significantly higher among patients having HRV (34.5%) infection and overall these patients had 2.5 times more odds of bronchodilators need. According to individual comparison, HRV infection was more prominently associated with bronchodilators need (OR: 5.5) than FLU infection. Similarly, need of steroid therapy was also significantly higher (47.1%) among patients with HRV infection and such patients had 4.2 times more chances of having steroid therapy than patients with RSV, FLU and others infections and 3.8 times more chances than patients with RSV.
It is interesting to note that need of oxygen therapy was significantly higher in RSV (74.7%) and HRV (63.2%) infection. Overall patients with RSV infection was 4.7 time more likelihood of having oxygen therapy than patients with HRV, FLU and others infection. It is worthwhile to mention that FLU infection was found to be inversely correlated with oxygen therapy (OR: 0.3) when compared with rest of the virus groups. The individual comparison of RSV and HRV with FLU infection showed that RSV and HRV infections were associated with oxygen therapy (OR: 31.5 and 17.6, respectively). However, RSV infection was found to be correlated with oxygen therapy (OR: 2.8) when compared with others infection.
The prevalence of severe respiratory complications was significantly higher (24.1%) among patients with HRV infection. Overall, HRV infection was correlated (OR: 4.7) with SRC while on the other hand, RSV infection was found to be inversely associated (OR: 0.41) with SRC. The individual comparison of HRV with RSV revealed that patients having HRV infection had 6.4 times more odds of having SRC than patients with RSV infection. Individual comparison of FLU infection with all other virus groups showed that FLU infection is not associated with any specific clinical outcomes in current study.
Discussion
Present study reports a large case series of patients (N=411) having acute respiratory tract infections with viral etiology. Current study is also first presentation of children aged<18 years with ARTIs attending emergency department of Zhumadian Central Hospital, China. Our findings provide additional support to previously published literature in this context.
Despite of high global burden of ARTI, the identification of causative agents usually omitted or limited to a few viruses easy to detect by rapid antigen direct tests (influenza virus and RSV). Sometimes empirical therapy without identification of causative agents may directly lead to antibiotic resistance, hospitalization and indirectly to nosocomial infection and burden to the health care system. More recently, nucleic acid amplification tests (e.g. multiplex PCR) were introduced in clinical practice for precise and rapid detection of causative agent in ARTIs. These techniques allow simultaneous detection of wide range of pathogens including viruses and atypical bacteria within frame of time [16]. Similar technique was used in current study and detected respiratory viruses in 76% of studied population. Detection rate reported by our study is comparable as reported by others [5,13]. Among patients with virus positive ARTIs, detection rate of single and mixed viral infections were 82% and 18%, respectively. These findings are also consistent with previous reports describing high detection rates of single and mixed viral infections [5,11,13].
Out of total patients with respiratory viral infection (N=312), the prevalence of RSV was higher than HRV while FLU and others were merely accounted in 9% and 14.7% of children, respectively. About 90% (281/312) studied participants had age<3 years in our study and rest of the children had age 3 to 18 years. Comparison of two age groups (Table 1) revealed the predominance of RSV (P=0.013), HRV (P=0.034) and others (P<0.001) among young children. These findings are also consistent with previous reports where RSV is predominant among young children [9,10]. Higher prevalence of HRV in young children in our study contraindicates the findings of Gooskens et al. who reported equal distribution of HRV among two age groups [5]. Firm epidemiological conclusion on association of FLU infection with age-distribution can’t be withdrawn in present study due to less number of cases in both age groups (n=26 vs. 2, respectively).
Signs and symptoms during ARTIs are usually atypical and diagnosis of specific viral infection based upon clinical presentations is difficult due to commonly shared signs and symptoms among viruses and mixed viral infections. In our study, we tried to evaluate specific signs and symptoms associated with specific viruses, as presence of fever was significantly higher among patients with FLU infection as compared to RSV and HRV (P<0.001). By the same way, cough was significantly associated with RSV infection when compared with FLU and others infection. But unfortunately, our findings are unable to make firm conclusion for signs and symptoms specifically related to different viral infections. It might be due to the presence of common clinical presentations among patients with viral infections and most importantly due to presence of mixed infection i.e. either mixed viral or virus and bacterial infection [11]. More large scale and controlled studies are needed in order to evaluate typical signs and symptoms for specific viral infection.
A comparison of clinical outcomes among children with respiratory viral infections by different viruses unveiled some similarities in these outcomes. High levels of CRP and WBCs were similar in all four types of virus groups. Similarly, use of antibiotics was also equally distributed among virus groups. These findings are supported by results of Gooskens et al. where author reported same distribution among virus groups [5]. On the other hand, Garcia et al. reported that patients with HRV infection had significantly higher levels of CRP and WBC. Similarly, use of antibiotics was also frequent among patients with HRV infection [12]. Rapid detection of RSV as compared to HRV by PCR might be a reason that use of antibiotic is more restricted in RSV infection than HRV infection [17,18].
It is interesting to note that treatments other than antibiotics and Severe Respiratory Complications (SRC) were significantly differing within four virus groups. Use of bronchodilators and corticosteroids were more common in HRV infection than RSV and others infection. Rational for bronchodilator treatment in our study was its effectiveness in reactive airway disease while corticosteroids were prescribed to alleviate wheezing induced by HRV virus. Despite of knowing the fact that RSV infection is often associated with respiratory complication, it is interesting to note that HRV infection was found to be associated with SRC than RSV (Table 3). These findings are also supported by results of Gooskens et al. where RSV was also found to be inversely associated with SRC [5]. Furthermore, infection with FLU virus was less likely to be associated with supplemental oxygen therapy. We can’t give a firm conclusion that patients with FLU infection are less likely to have oxygen therapy because of very less number of patients for comparative analysis (n=2). As life threatening events with FLU infection have been reported therefore such assumption requires to be tested by controlled studied with larger patient`s pool. Fortunately, none of the patients were died in our study [19].
Being a monocentric and retrospective study design, some important limitations are needed to be addressed. Current study lacks virus-clinical outcomes correlation information for other settings i.e. private paediatric clinics and basic health units. Due to retrospective nature of study, presence of reporting biasness might be present [20]. In routine practice, more cautious and vigilant clinical and diagnostic approaches are provided to younger children that may lead to patient’s selection biasness as we set criteria of selection of sampling within 48 hours. It might be contributed to the reason that most of our studied participants (approximately 90%) were belonged to young age group (<3 years). Different sites were used for respiratory sampling in our study and it may cause differences in sensitivity of PCR based on viral frequency. Though our study tried to identify maximum number of viruses including HBoV and HCoV (that were not detected by Gooskens et al.) but still multiplex PCR was unable to identify HKU1, enteroviruses and influenza C virus in current study causing underestimation of prevalence of ARTIs. We performed multiple comparisons in our study that may lead to many type 1 errors. We did not use Boneferroni correction for the adjustment of this error because it may increase type II errors and hence interpretation errors [21]. We aimed current study to determine some novel correlations of viruses with clinical outcomes (hypothesis generation), not hypothesis testing. More studies with better and improved study protocols are needed to confirm ours and others findings to make firm conclusion on virus-clinical outcome co-relation.
Conclusion
We described a large case series of children presented to the emergency department of our hospital with ARTIs. Viral agents were identified among more than 70% population by using molecular diagnostic methods. Presenting clinical presentations does not discriminate four virus groups. Some of the demographics and clinical outcomes were equally distributed among virus groups while infections with RSV and HRV portended heavy burden of morbidity in our study as compared to infections with FLU and others (PIV, HCoV, HMPV, HBoV and HAdV).
Acknowledgement
We are thankful to the staff of emergency department of Zhumadian Central Hospital for providing assistance and all the possible supports to conduct this study.
Conflict of Interest
None
References
- Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics 2008; 121: 244-252.
- Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet 2005; 1; 365: 1147-1152.
- Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis 2002; 2: 25-32.
- Wei L, Chan KH, Ip DK, Fang VJ, Fung RO, Leung GM, Peiris MJ, Cowling BJ. Burden, seasonal pattern, and symptomatology of acute respiratory illnesses of different viral etiology in children presenting at outpatient clinics in Hong Kong. ClinMicrobiol Infect 2015; 21: 861-866.
- Gooskens J, van der Ploeg V, Sukhai RN, Vossen AC, Claas EC. Clinical evaluation of viral acute respiratory tract infections in children presenting to the emergency department of a tertiary referral hospital in the Netherlands. BMC Pediatr 2014; 14: 297.
- Monto AS. Epidemiology of viral respiratory infections. Disease 2003; 49: 160-174.
- Jacobs JW, Peacock DB, Corner BD, Caul EO, Clarke SK. Respiratory syncytial and other viruses associated with respiratory disease in infants. Lancet 1971; 1: 871-876.
- Forster J, Ihorst G, Rieger CH, Stephan V, Frank HD, Gurth H, Berner R, Rohwedder A, Werchau H, Schumacher M, Tsai T. Prospective population-based study of viral lower respiratory tract infections in children under 3 years of age. Eur J Pediatr 2004; 163: 709-716.
- Iwane MK, Edwards KM, Szilagyi PG, Walker FJ, Griffin MR, Weinberg GA, Coulen C, Poehling KA, Shone LP, Balter S, Hall CB. Population-based surveillance for hospitalizations associated with respiratory syncytial virus, influenza virus, and parainfluenza viruses among young children. Pediatr 2004; 113: 1758-1764.
- Bourgeois FT, Valim C, Wei JC, McAdam AJ, Mandl KD. Influenza and other respiratory virus–related emergency department visits among young children. Pediatr 2006; 118: e1-8.
- Cilla G, Onate E, Perez-Yarza EG, Montes M, Vicente D. Viruses in community-acquired pneumonia in children aged less than 3 years old: High rate of viral coinfection. J Med Virol 2008; 80: 1843-1849.
- Garcia-Garcia ML, Calvo C, Pozo F, Villadangos PA, Perez-Brena P, Casas I. Spectrum of respiratory viruses in children with community-acquired pneumonia. Pediatr Infect Dis J 2012; 31: 808-813.
- Laurent C, Dugue AE, Brouard J, Nimal D, Dina J, Parienti JJ, Vabret A. Viral epidemiology and severity of respiratory infections in infants in 2009: a prospective study. Pediatr Infect Dis J 2012; 31: 827-831.
- Pierangeli A, Scagnolari C, Selvaggi C, Monteleone K, Verzaro S, Nenna R, Cangiano G, Moretti C, Papoff P, Antonelli G, Midulla F. Virological and clinical characterization of respiratory infections in children attending an emergency department during the first autumn-winter circulation of pandemic A (H1N1) 2009 influenza virus. ClinMicrobiol Infect 2012; 18: 366-373.
- Loens K, Van Loon AM, Coenjaerts F, Van Aarle Y, Goossens H, Wallace P, Claas EJ, Ieven M. Performance of different mono-and multiplex nucleic acid amplification tests on a multi-pathogen external quality assessment panel. J Clinical Microbiol 2012; 50: 977-987.
- Pillet S, Lardeux M, Dina J, Grattard F, Verhoeven P. Comparative evaluation of six commercialized multiplex PCR kits for the diagnosis of respiratory infections. PLoS One 2013; 8: e72174.
- Purcell K, Fergie J. Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections. Arch PediatrAdolesc Med 2002; 156: 322-324.
- Wishaupt JO, Russcher A, Smeets LC, Versteegh FG, Hartwig NG. Clinical impact of RT-PCR for paediatric acute respiratory infections: a controlled clinical trial. Pediatrics 2011; 128: e1113-1120.
- Ruf BR, Knuf M. The burden of seasonal and pandemic influenza in infants and children. Eur J Pediatr 2014; 173: 265-276.
- Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Incidence, characteristics and risk factors of acute kidney injury among dengue patients: a retrospective analysis. PloS One 2015; 10: e0138465.
- Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Clinico-laboratory spectrum of dengue viral infection and risk factors associated with dengue haemorrhagic fever: a retrospective study. BMC Infect Dis 2015; 15: 1.