Research Article - Biomedical Research (2017) Volume 28, Issue 7
Urodynamic and radiological assessments in sigmoidorectal (Mainz II) pouch for continent urinary diversion in Chinese patients after radical cystectomy
Jingmin Yan, Bin Sun, Xianchu Li, Quan Hong, Guangxin Pan, Jizhou Shi and Heqing Guo*
Department of Urology, the Air Force General Hospital, People's Liberation Army, Beijing, China
- *Corresponding Author:
- Heqing Guo
Department of Urology
The Air Force General Hospital
People's Liberation Army
China
Accepted on December 1, 2016
Abstract
Purpose: To evaluate the pressure-volume changes and the radiological findings in Chinese patients undergoing sigmoidorectal pouch using sigmoidorectal pouch.
Methods: The ureters were implanted into the post walls of the detubularized sigmoid segment. Sigmoidal pressure and capacity and the anal pressure were measured. The intravenous pyelography, colon X-rays and uroflow rate assay were used. Continence was evaluated by interviewing the patients. A total of 20 patients with muscle-invasive bladder cancer underwent radical cystectomy and Mainz pouch II procedure between 2007 and 2012.
Results: In contrast to preoperative data, followed by postoperative procedure, the index has been changed significantly, such as colon X-rays anteroposterior pouch X-rays showed no passage up to an average volume of 360 ml (270-532 ml) through the descending colon, the sigmoidal colon pressure was on 26 cm H2O at the 3rd to the 6th month, but no changes in preoperative anal sphincter pressure.
Conclusion: Sigmoidorectal pouch could provide a reservoir with higher capacity and lower pressure without reflux to the upper urinary tract and descending colon, suggesting that Pouch II is a safe, effective and reproducible surgical means for urinary diversion in patients undergoing radical cystometry.
Keywords
Urodynamics, Invasive bladder cancer, Upper urinary tract, Mainz pouch II, Renal function.
Introduction
While the ileal conduit and orthotopic neobladder are the most commonly used diversions today [1], continent cutaneous reservoirs remain an invaluable treatment option for a welldefined subset of indications. After several decades of surgical experience, the optimization of continence is still on-going, which largely determines the treatment success in terms of patient satisfaction and quality of life. At present, no consensus has been achieved regarding an optimal technique. Common problems include stomal stenosis with impaired catheterisation, urinary incontinence, and nipple gliding [2]. The ideal urinary diversion should be fully continent, cosmetically impeccable, allow easy and complete emptying within socially acceptable intervals, and preserve renal function. The surgeon’s ‘wish list’ consists a surgical technique with a high degree of standardization and reproducibility, an acceptable learning curve, minimal tissue requirements, a low complication rate, favourable long-term functional results, and easy accessibility for potential instrumental exploration [2].
The first type of urinary diversion is ureterosigmoidostomy, which was developed about 140 years ago [3]. This method became more popular during the first half of the 20th century, leading to a number of technical modifications [4]. However, this method in which a colonic reservoir with high pressure was in permanent contact with the urine caused serious metabolic complications such as severe fluid and electrolyte imbalances, hyperchloremic metabolic acidosis, obstruction in the ureterocolonic unit, urinary infections and acute pyelonephritis, thus giving way to researches for newer diversions. Although Goodwin corrected certain complications using modified anastomosis techniques.
Ureterosigmoidostomy technique was not used due to continuing complications [5]. Ileal conduit diversion defined by Bricker in 1950 led to a decrease in complications, having been a selected method of diversion for years [6]. However, on a long-term basis, the presence of conditions such as stomal problems, urointestinal obstructions in anastomosis, incontinence and poor patient compliance led the researches once again to new diversions [7]. After Hinmann [8] accentuated the important role of detubularisated intestinal segments to obtain a reservoir with a higher capacity and lower pressure, Fisch et al. [9] applied the same principle to the colon and described the diversion as Mainz pouch II (sigmoidorectal pouch), which was further modified by Gumus et al. [10]. It has been demonstrated that the Mainz II is a simple, safe and effective approach for urinary diversion in invasive bladder cancer, and a good quality of life and can be achieved in patients receiving this procedure [11-14]. In this study, we performed urodynamic and radiological assessments in Chinese patients with invasive bladder cancer who received cystectomy and a sigmoidorectal pouch (Mainz pouch II). This aim of this study was to evaluate the short- and long-term outcome of this procedure in terms of reservoir volume, sigmoidal colon pressure, metabolic complications, and quality of life, especially continence.
Methodology
Patient selections
This work was approved by our Hospital. Between 2007 and 2012, a total of 20 patients (19 male and 1 female, mean age 62 years, ranging from 38 to 70) with invasive bladder cancer were recruited for radical cystectomy and Mainz pouch II type urinary diversion. The inclusion criteria include: 1. invasive bladder cancer with/without urethral carcinoma; 2. Selfmotivation to be continent postoperatively; 3. base excess (BE) limit was accepted at-3 mmol/L; 4. rectosigmoidoscopy reveals no tumor or inflammation; 5. Capable of tolerating 500 ml normal saline in the colon for at least 1 h. Rectosigmoidoscopy, contrast colon X-ray examinations, and anal pressure were recorded and rectosigmoid capacity was measured under fluoroscopic control.
Urodynamic studies
Patients were given a diet with clear liquid for 2 days. A twoway 7.3 F catheter (one way for instillation, the other for pressure measurement) was placed into the sigmoid colon endoscopically. Another 12 F catheter with a balloon at the tip was also placed into the rectum for abdominal pressure measurement. The patient was then in a semi-lying position and the sigmoid pressure studies were performed by using the urodynamic device (Medical Measurement Systems (MMS)) according to the existing ICS GUP guidelines. The infusion rate of the 0.9% saline solution was 45 ml/min and the maximum amount of instillation was 500 ml. In this way, the baseline sigmoidorectal pressure and abdominal pressure were determined and the anal sphincter pressure was recorded. The uroflow rate was recorded by uroflowmetry.
Surgical procedure
All 20 patients underwent sigmoidorectal pouch procedure following radical cystectomy. The surgical procedure of the sigmoidorectal (Mainz II) pouch was performed according to Fisch et al. [9] and Gumus et al. [10]. Briefly, the rectosigmoid was cut open and the sigmoid was reconstructed, detubularized and widened. The posterior wall was closed for the seromuscular area and the mucosa by running Vicryl 3-0 and catgut 4-0 sutures, respectively. In the posterior wall, a 4-5 cm submucosal tunnel was formed to reimplant the ureters. The size of the entrance of the ureter into the pouch was twice as large as the diameter of the ureter. 8 Fr feeding tubes were placed as ureteral stents. Like the posterior wall, the anterior wall of the neobladder was closed. Then, a 30 Fr rectal tube with multiple holes was inserted in the rectum. In the procedure, the angle between the pouch and descending colon was particularly preserved in the prospect of preventing reflux from the pouch to the upper segments of colon. The mean operative time in this study was between 165 and 180 min.
Postoperative care and follow up
The patients were discharged from the hospital with the prescription of 1.5 g oral bicarbonate daily (24 hours for one time) and a diet rich in potassium. Metabolic assessment was performed postoperatively on the 15th day, at the 3rd and 6th month, at the end of the first year, and then every year. In these assessments, the blood biochemistry, blood gas analysis and CBC were examined. Same pressure studies and radiological assessments (pouch graphs and IVP) were carried out at the 3rd to 6th month postoperatively. Continence was evaluated by interviewing the patients during each follow-up visit.
Statistical analysis
End-filling pressures and volumes of sigmoidorectal colon and pouch were compared by paired Student’s t test using SPSS 19.0. Both statistical tests were two-sided, and the threshold of significance was set at p=0.05.
Results
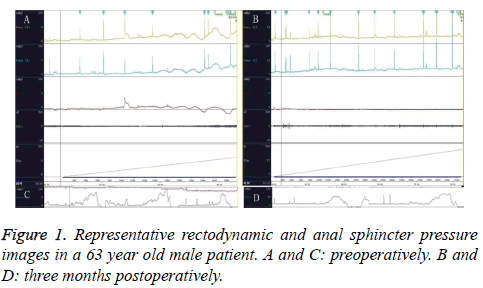
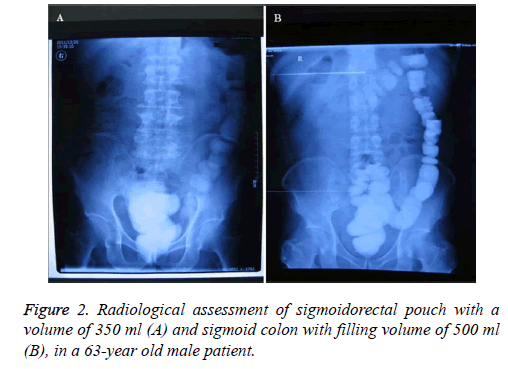
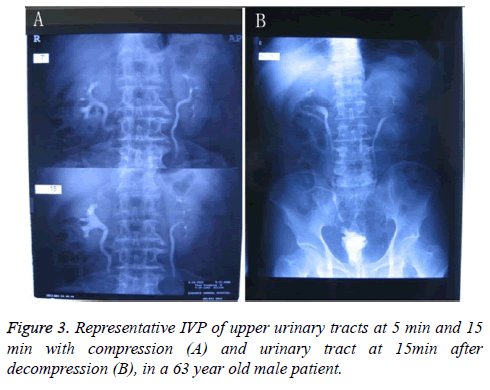
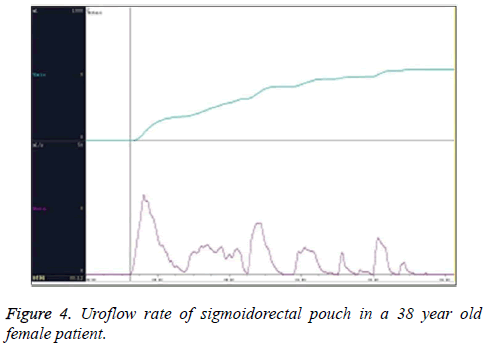
Twenty patients were eligible for sigmoidorectal pouch procedure. Before operation, the pressure and radiologic studies were performed and the baseline characteristics are shown n Table 1. Mean follow-up was 34 (5-54) months in the 20 cases. Our pressure studies showed an interesting pattern. Although the mean basal pressure in sigmoid colon was 36 cm H2O preoperatively, it was found to be 26 cm H2O at the 3rd to 6th month postoperatively and decreased significantly (Table 2 and Figure 1). While some contractions were found and their pressures ranged from 25 to 44 cm H2O preoperatively in all cases, there was no involuntary contraction in 20 patients postoperatively. When patients felt abdominal discomfort, the pressure raised up to 20 cm H2O on average. We accepted that this pressure referred to a desire to void. No cases developed pyelocaliceal ectasia in the ureters. There was one slight stricture in the right ureterointestinal anastomosis but no further intervention was needed. The pouch X-rays showed no sigmoidoureteral reflux in any patients (Figure 2A). While the amount of radioopaque substance (Compound Diatrizoate Meglumine) going up to the descending colon was about 150 ml (130-180) preoperatively (the mean sigmoid capacity, (Figure 2B)), the capacity increased to 360 ml (270-532) postoperatively (mean sigmoidorectal pouch capacity) (Table 2 and Figure 2A). The anal sphincter pressure was 90 cm H2O on average preoperatively and did not change postoperatively. The IVP study demonstrated that the upper urinary tract was preserved well (Figure 3). The Qmax was 30 ml/s and the average uroflow rate was 8 ml/s under abdominal strain (Figure 4). There was no residual urine in the sigmoidorectal pouch in any of the cases. Postoperatively, 18 cases had a normal metabolic status. Postoperative metabolic assessment in the 3rd to the 6th months revealed hyperchloremic metabolic acidosis and hypokalaemia in two cases, who had a BE value of-5 mmol/L. These two cases did not use 15 g postoperative bicarbonate protocol regularly during the follow-up period, which might be the cause of their abnormal metabolic status. The hyperchloremic metabolic acidosis and hypokalaemia were corrected with the oral intake of 15 g bicarbonate and kalium tablets. There was no faecal transit problem in any of the cases, and 17 patients could urinate and defecate separately. The other patients could not urinate and defecate separately with urine and faeces mixed usually. Two male patients suffered from unilateral pyelonephritis owing to not urinating regularly at the second and third year postoperatively, and were cured by intravenous injection of antibiotics. Following the advice of urinating regularly, there were no episodes of pyelonephritis in other 18 patients and the two affected patients were well.
| Age (years) | Male/female | G1 | G2 | G3 | Stage II | Stage III |
|---|---|---|---|---|---|---|
| 62±8.0 (38~70) | 19-Jan | 10% (2/20) | 60% (12/20) | 30% (6/20) | 70% (14/20) | 30% (6/20) |
Table 1. Baseline characteristics and the staging of invasive bladder cancer in twenty patients undergoing radical cystectomy and sigmoidorectal (Mainz II) Pouch.
| Variables (M ± SD) | Preoperation | 3 to 6 m postoperatively | P |
|---|---|---|---|
| End-filling pressure of sigmoidorectal colon/pouch | 36±3.5 cm H2O | 26±4.0 cm H2O | <0.001 |
| Pressure of anal sphincter | 90±9.5 cmH2O | 90±9.6 cmH2O | 1 |
| Qmax | 30±6.0 ml/s | ||
| Qave | 9±1.5 ml/s | ||
| Volume of sigmoidorectal colon/pouch | 150±5.8 ml | 360±69.4 ml | <0.001 |
Table 2. Urodynamic variables measured pre- and/or 3 to 6 months postoperatively in twenty patients undergoing radical cystectomy and sigmoidorectal (Mainz II) Pouch.
Discussion
An abdominal pressure level ranging from 60 to 80 cm H2O is required to push faeces forward. This level may increase up to 260 cm H2O during the defaecation process [9]. The aim of making an ureterosigmoidal diversion should be to increase the capacity and to lower the high pressure, thus leading to a decrease in reflux in both the upper colonic segments and urinary tract to prevent the very well-known metabolic complications.
In 1988, Kock et al. first described a technique for sigmoidorectal reservoir with low pressure and high capacity [15]. Fisch et al. simplified the procedure on Mainz pouch II type diversion [16]. This type of urinary diversion has achieved high patient satisfaction. Independence from appliances such as external collecting devices and catheters favours this type of diversion from the patients’ view. There is no risk of rupture compared with other continent urinary diversions. As with orthotopic bladder substitution, the lack of cutaneous stoma is regarded as beneficial for patient’s body image. A stoma-free type of urinary diversion is also particularly important in Muslim countries since it preserves ablution, an important Islamic rule of the prayer, and in countries where, for economic and/or logistical reasons, it is difficult to provide a sufficient supply of collecting devices and catheters, and to have access to enterostomal therapists [10,17].
Fisch et al., Gilja et al. and Gumus et al. have conducted comprehensive studies with the sigmoidorectal pouch pressure [10,16,18]. Fisch et al. [12] reported a preoperative average pouch pressure of 23 cm H2O in their study group of 72 subjects, whereas Gilja et al. [18] and Gumus et al. [10] reported that it was 21.4 and 20 cm H2O, respectively. We also measured this pressure level, which was 36 cm H2O preoperatively. The preoperative levels of the three studies were similar, but the preoperative average pouch pressure was higher than that in their studies. The sigmoidorectal pouch pressure was 26 cm H2O in the present study, and it was similar to the results of 21 and 21.7 cm H2O determined by Fisch et al. [16] and Gilja et al. [18], respectively. And it was higher than the average 6 cm H2O pouch pressure that was measured at the 3rd month determined by Gumus et al. [10]. Gumus et al. [10] concluded that in addition to the role of their larger reservoir, insertion of catheters into the reservoir with the help of rectosigmoidoscopy during the measurement of average pouch pressure might contribute in achieving such a lower value. The differences among the four studies may be due to the patient position and examination methods to adjust the zero level. Recently, Sullivan et al. [19] demonstrated that initial resting abdominal and intravesical pressures were similar and at least 95% lay in the following ranges: lying 0-18 cm H2O, sitting 15-40 cm H2O, and standing 20-50 cm H2O, respectively.
As reported by Gilja et al. [18] and Gumus et al. [10], the mean reservoir capacities were 300 ml (250-500 ml) and 520 ml (270-650 ml), respectively. The mean sigmoidorectal pouch capacity was 360 ml (270-532 ml). Though the mean pouch capacities were somewhat different, the range of pouch capacity was comparable, and similar to the physiologic bladder volume in normal people.
Gumus et al. [10] reported that the mean pouch pressure when patients felt an abdominal discomfort before micturation was 13.8 cm H2O and interval to reach that level was about 5.2 h. They suggested that the patients who had been previously told to urinate frequently were recommended to have micturation intervals not shorter than 5 h, and to urinate when they felt an abdominal discomfort. The requirement for micturation during the night was also cancelled. The patients stated that they urinate one to four times during the night in this study, and one patient stated that he has been used to urinate four times in the night due to previous LUTS and bad sleep habits. While the upper urinary tract was well preserved in all the patients, we still recommend the patients to urinate no less than once in the night to protect the kidney function. The Qmax was 30 ml/s and the average uroflow rate was 8 ml/s under abdominal strain, the value of Qmax was larger than 15 ml/s and 20 ml/s for men and women, respectively. Therefore, the sense of micturation was more similar to the processes of physical voiding.
Electrolyte imbalances and hyperchloremic metabolic acidosis are important problems following ureterosigmoidostomy [20,21], however, sufficient renal function is believed to prevent the development of such complications [22]. Pyelonephritis and ureteral obstruction caused by the reflux may lower the renal function and therefore exacerbate these complications. Jin et al. confirmed that obstruction was the leading and an independent risk factor for renal function deterioration for both ileal conduit diversion patients and orthotopic ileal bladder substitution patients who lived no less than 10 years [23]. The most important principle in forming a reservoir is to prevent ureteral obstruction and reflux. IVP observation revealed that no ureteral obstruction or kinking of ureter occurred; the ureter-sigmoidal anastomosis is more physiological and natural. The low pressure and high capacity of sigmoidorectal pouch and attempts aim to prevent ureteral obstruction and reflux preserved the renal function.
It has been accepted that the absorptive feature of a reservoir decreases with time as a result of villous atrophy and muscular thickening within the intestinal mucosa caused by the urine [22]. The reconstructive structures of sigmoidorectal pouch partially mimic the natural urointestinal structure in birds which has muscle clusters both in the ureter and urodeum near the opening area and the coprourodeal fold prevents the mixing of faeces and urine, inhibits the effects of increased pressure and prevents the reflux of urine to the upper segments [24]. It is widely believed that the refluxing to the functional absorptive descending colon leads to the increased number of metabolic complications. During the preoperative radiological assessments, we observed a passage of opaque substance through the descending colon at a volume of 150 ml, whereas during the postoperative period, no passage of opaque substance through the descending colon was observed up to a volume of 360 ml due to preserved angulation, increased capacity, and lowered pressure. The target is to keep the urine in the reservoir, which will lose its absorptive feature with time. An increased capacity of reservoir, low pressure, and preserved angulation between pouch and descending colon may prevent the urine from passing through to the descending colon. Although the sigmoidorectal pouch illustrates many advantages for patients undergoing radical cystometry, there is also one drawback that presence of metabolic acidosis, which can be managed by oral alkalinisation therapy. We utilized the prophylactic oral alkalinisation in all of the patients, and no patient resulted in the severe acidosis necessitating hospital admission, which is not consistent with the previous study [25]. Meanwhile, the sigmoidorectal pouch could also cause the complication of unilateral pyelonephritis, which could be prevented by aminoglycoside antibiotics in the kidney.
Conclusions
In this study, we reported the good filling pressure and capacity of the neobladder by Detubularized sigmoidorectal pouch, with well-preserved renal function, physical micturation, and minimal metabolic complications. This should be attributed to the preserved angle between the descending and the sigmoid colon, which keeps urine in a certain space under a lower pressure to prevent the reflux to both the upper urinary tract and the upper part of the colon. Actually, this study confirmed the conclusions of the previous studies. What's most important is that this study is the first one to analyse the usage of sigmoidorectal pouch in Chinese people.
Acknowledgements
None
Competing Interests
None
References
- Ardelt PU, Woodhouse CR, Riedmiller H, Gerharz EW. The efferent segment in continent cutaneous urinary diversion: a comprehensive review of the literature. BJU Int 2012; 109: 288-297.
- Bricker EM. Bladder substitution after pelvic evisceration. SurgClin North Am 1950; 30: 1511-1521.
- Fisch M, Wammack R, Muller SC, Hohenfellner R. The Mainz pouch II (sigma rectum pouch). J Urol 1993; 149: 258-263.
- Fisch M, Wammack R, Muller SC, Hohenfellner R. The Mainz pouch II. EurUrol 1994; 25: 7-15.
- Gumus E, Miroglu C, Saporta L, Baayaran G, Horasanli K. Rectodynamic and radiological assessment in modified mainz pouch II cases. EurUrol 2000; 38: 316-322.
- Gilja I, Kovacia M, Radej M, Kosuta D, Bakula B. The sigmoidorectal pouch (Mainz pouch II). EurUrol 1996; 29: 210-215.
- Gumus E, Mutus R, Daglioglu S, Tanriverdi O, Horasanli K. The relationship between uretero-cloacal structure in birds and sigmoidorectal pouch surgery. AktuelleUrol 2004; 35: 228-232.
- Hautmann RE, Abol-Enein H, Davidsson T, Gudjonsson S, Hautmann SH. ICUD-EAU International Consultation on Bladder Cancer 2012: Urinary diversion. EurUrol 2013; 63: 67-80.
- Hinman F. Weyrauch HM Jr. A critical study of the different principles of surgery which have been used in ureterointestinal implantation. Trans Am Genito-Urin Sur 1936; 29: 15.
- Hinman F Jr. Selection of intestinal segments for bladder substitution: Physical and physiological characteristics. J Urol.1988; 139: 519-523.
- Hammouda H, Shalaby M, Adelelateef A, Elakkad M. Mainz II and double folded rectosigmoid pouches. Experience with 95 patients. J SurgOncol 2006; 93: 228-232.
- Hadzi-Djokic JB, Basic DT. A modified sigma-rectum pouch (Mainz pouch II) technique: analysis of outcomes and complications on 220 patients. BJU Int 2006; 97: 587-591.
- John JS. Use of bowel in urologic surgery. UrolClin North Am 1997; 24: 715-724.
- Jin XD, Roethlisberger S, Burkhard FC, Birkhaeuser F, Thoeny HC, Studer UE. Long-term renal function after urinary diversion by ileal conduit or orthotopic ileal Bladder substitution. EurUrol 2012; 61: 491-497.
- Kock NG, Ghoneim MA, Lycke KG, Mahran MR. Urinary diversion to the augmented and valved rectum: Preliminary results with a novel surgical procedure. J Urol 1988; 140: 1375-1379.
- McDougal WS. Metabolic complications of urinary intestinal diversion. J Urol 1992; 147: 1199-1208.
- Philipson BM, Hockenstrom T, Akerlund S. Biological consequences of exposing ileal mucosa to urine. World J Surg 1987; 11: 790-797.
- Pahernik S, Wiesner C, Gillitzer R, Stein R, Thuroff JW. Conversion from colonic conduit into recto-sigmoid pouch (Mainz pouch II). BJU Int 2006; 97: 157-160.
- Simon J. Ectopiavesica absence of the anterior walls of the bladder and pubic abdominal parities. Operation for directing the orifices of the ureters into the rectum; temporary success; subsequent death; autopsy. Lancet 2004; 1852: 568.
- Stameyt A. The pathogenesis and implications of the electrolyte imbalance in ureterosigmoidostomy. SurgGynecolObstet 1956; 103: 736-758.
- Sullivan JW, Grabstald H, Whitmore WF Jr. Complications of ureteroileal conduit with radical cystectomy: review of 336 cases. J Urol 1980; 124: 797-801.
- Sullivan JG, Swithinbank L, Abrams P. Defining achievable standards in urodynamics-a prospective study of initial resting pressures. NeurourolUrodyn 2012; 31: 535-540.
- Triantafyllidis A, Rombis V, Papatsoris AG, Papathanasiou A, Kalaitzis C. Sigmoidorectal (Mainz II) pouch for continent urinary diversion in bladder cancer. Int J Urol 2005; 12: 599-602.
- Zhvania G, MshvildadzeSh, Managadze G, Khvadagiani G. Results of radical cystectomy with Mainz pouch II diversion (single institution experience). Georgian Med News 2012; 211: 7-13.
- Girgin C, Sezer A, Ozer K, Tarhan H, Bolukbasi A. Comparison of three types of continent urinary diversions in a single center. Sci World J 2004; 4: 135-141.