Research Paper - Biomedical Research (2023) Volume 34, Issue 3
Underestimated etiology of tracheobronchomalacia in adults.
Zu Cao1, Yan He1, Shuo Liang1, Haiwen Lu1, Ye Gu2, Jiuwu Bai1*
1Department of Respiratory and Critical Care Medicine, Shanghai Pulmonary Hospital, Respiratory Medicine Institute, Tongji University School of Medicine, Shanghai 200433, China
2Endoscopy Center, Shanghai Pulmonary Hospital, Respiratory Medicine Institute, Tongji University School of Medicine, Shanghai 200433, China
- Corresponding Author:
- Jiuwu Bai
Department of Respiratory and Critical Care Medicine
Shanghai Pulmonary Hospital
Respiratory Medicine Institute
Tongji University School of Medicine
Shanghai 200433
China
Accepted date: May 22, 2023
Abstract
Background: Tracheobronchomalacia (TBM) is an infrequent airway disease, but frequently unrecognized or misdiagnosed with other respiratory diseases, and its etiology remains unclear in China.
Methods: Anthropometric information, symptoms, signs, etiology, diagnosis, treatment, smoking history, medical history, and prognosis of ten patients were retrospectively analyzed.
Results: The median onset age of the ten patients was 55 years. Patients presented productive cough, chest distress, and inspiratory wheezing. Etiologies of TBM included Chronic Obstructive Pulmonary Disease (COPD), tracheobronchial tuberculosis, relapsing polychondritis, asthma and bronchiectasis, and chronic bronchitis, the first two of which were dominated, accounting for 40%. Obstructive ventilation disturbance was found in the lung function test, and the flow-volume curve displayed main airway obstruction. Seven patients were worried about the side-effect of stenting, so they refused stenting. During follow-up (3-120 months), all patients survived.
Conclusion: In China, main etiologies of TBM may be COPD and tracheobronchial tuberculosis, which are different from those of western countries and seriously underestimated.
Keywords
Tracheobronchomalacia, Etiology, Bronchoscopy, Multidetector computed tomography, Chronic obstructive pulmonary disease, Tracheobronchial tuberculosis.
Introduction
Tracheobronchomalacia (TBM) is defined as the complete or nearly collapse of the tracheal lumen during respiration, which is caused by the loss of cartilage support of the trachea or main bronchus [1]. The main methods for diagnosing TBM are bronchoscopy and multidetector Computed Tomography (CT) [2]. Bronchoscopy is the traditional diagnostic method for TBM and can assess its severity [3]. Multidetector CT with 3-dimensional imaging is a noninvasive diagnostic method of TBM and provides anatomical information consistent with and complementary to bronchoscopy [4]. However, TBM is frequently unrecognized or misdiagnosed with other respiratory diseases due to the lack of awareness [5,6]. A survey showed that 71% of pulmonologists could not recognize TBM in bronchoscopy and 61% of them on CT examination [7]. TBM is often confused with obstructive airway disease and can be confirmed by pulmonary function tests after ruling out other diseases [8,9].
In adults, the main type of TBM is secondary TBM. TBM occurs in the normally developed trachea due to certain situations [2,4,10-13], some due to mechanical reasons, such as tracheal surgery, closed chest trauma, tracheostomy, etc. some due to chronic airway inflammation, the main representative diseases are Chronic Obstructive Pulmonary Disease (COPD), uncontrolled asthma, recurrent infection, relapsing polychondritis, tuberculosis, malignant airway obstruction, etc. and some due to other causes, such as cysts. According to previous reports of Western countries, the more common etiologies were COPD, asthma, Mounier- Kuhn syndrome and relapsing polychondritis [10-13]. However, PubMed database search for published articles on TBM revealed few case reports of TBM in China.
Materials and Methods
Patients
A retrospective analysis was made on basis of diagnosis and treatment process of ten TBM patients who were hospitalized in the outpatient department of Shanghai Pulmonary Hospital from December 2008 to December 2020, including general data and anthropometric data (i.e. age and sex), smoking history, medical history, onset age, course of disease, symptoms (such as sputum, cough, expectoration, chest distress, chest pain, and hemoptysis), signs, etiology, malacia position, diagnosis, treatment and prognosis. The study was conducted in strict compliance with the revised Declaration of Helsinki, and it was approved by the Ethics Committee of Shanghai Lung Hospital (K21-302; Shanghai, China).
Diagnostic criteria for TBM
At present, the main diagnostic modality and severity assessment of TBM are mainly through bronchoscopy and multidetector CT with 3-dimensional imaging [3,14]. The diagnostic criteria for adult TBM are that airway lumen stenosis during expiration is more than 50% [15]. In this study, the diagnosis of TBM was made by bronchoscopy and multidetector CT with 3-dimensional imaging.
Results
Of the ten patients, the median onset age was 55 years (32- 74 years), and the median time of diagnosis was 57.8 years (32-75 years). The course of disease ranged from 3 months to 120 months. Three patients had a history of smoking and COPD, two patients had a history of tracheobronchial tuberculosis, and one patient had a history of asthma and bronchiectasis (Table 1). Eight patients were misdiagnosed in other hospitals (3 cases of asthma; 3 cases of COPD; 2 cases of chronic bronchitis).
| Patient No. | Age | Sex | Onset age | Course of disease | Smoking | Other disease history |
|---|---|---|---|---|---|---|
| 1 | 38 | F | 37 | 13 months | No | No |
| 2 | 71 | M | 62 | 117 months | Yes | COPD |
| 3 | 59 | F | 59 | 25 months | No | Tracheobronchial Tuberculosis |
| 4 | 32 | M | 32 | 3 months | No | Tracheobronchial Tuberculosis |
| 5 | 75 | F | 74 | 14 months | No | Right hand injury |
| 6 | 54 | M | 54 | 2 months | Yes | COPD |
| 7 | 52 | F | 52 | 4 months | No | No |
| 8 | 73 | M | 72 | 12 months | No | No |
| 9 | 55 | F | 54 | 12 months | No | Asthma and bronchiectasis |
| 10 | 69 | M | 59 | 120 months | Yes | COPD |
Note: COPD: Chronic Obstructive Pulmonary Disease; F: Female; M: Male.
Table 1. Demographic data of ten patients.
The most common clinical symptom was chest distress. 90% (9/10) of the patients complained of chest distress, seven patients complained of expectoration, two patients had dry cough, two patients had chest pain, and a patient had hemoptysis. Inspiratory wheezing rale was heard during auscultation, and two patients had tachypnea, in examination (Table 2).
| Patient no. | Symptoms | Signs | |||||
|---|---|---|---|---|---|---|---|
| Cough | Sputum | Chest distress | Chest pain | Hemoptysis | Tachypnea | Inspiratory phase wheezing sound | |
| 1 | √ | √ | √ | √ | √ | √ | |
| 2 | √ | √ | √ | √ | |||
| 3 | √ | √ | √ | √ | √ | √ | |
| 4 | √ | √ | √ | ||||
| 5 | √ | √ | √ | √ | |||
| 6 | √ | √ | √ | √ | √ | √ | √ |
| 7 | √ | √ | |||||
| 8 | √ | √ | |||||
| 9 | √ | √ | √ | √ | √ | ||
| 10 | √ | √ | √ | ||||
Table 2. Symptoms and signs of ten patients.
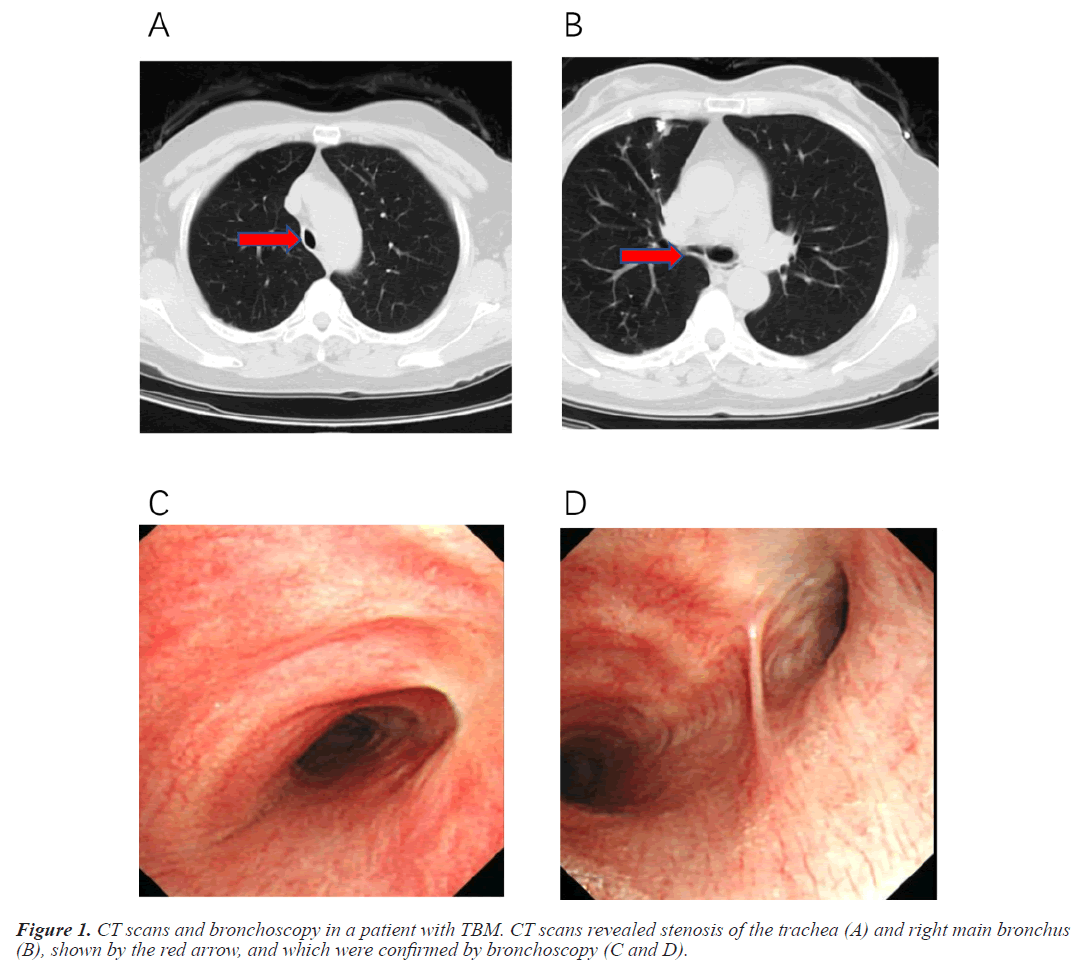
According to the diagnostic criteria proposed by Ngerncham et al., [14], TBM was diagnosed by dynamic bronchoscopy and multidetector CT with 3-dimensional imaging, and the diagnosis of each patient in this study complied with the requirements, as shown in Table 3 and Figure 1.
| Patient no. | Methods of diagnosis | Position | Etiology | Therapy | Current clinical status (Duration of survival) |
|---|---|---|---|---|---|
| 1 | Bronchoscopy 3D-CT |
BM | Polychondritis | Symptomatic therapy | Survived (74 months) |
| 2 | Bronchoscopy 3D-CT |
Trachea | COPD | Trachea stent | Survived (70 months) |
| 3 | Bronchoscopy 3D-CT |
Trachea and RM | Tracheobronchial Tuberculosis | Symptomatic therapy | Survived (27months) |
| 4 | Bronchoscopy 3D-CT |
Trachea and RM | Tracheobronchial Tuberculosis | Symptomatic therapy | Survived (12 months) |
| 5 | Bronchoscopy 3D-CT |
RM | Chronic bronchitis | Symptomatic therapy | Survived (3 months) |
| 6 | Bronchoscopy 3D-CT |
BM | COPD | Trachea stent | Survived (2 months) |
| 7 | Bronchoscopy 3D-CT |
LM | No | Symptomatic therapy | Survived (4 months) |
| 8 | Bronchoscopy 3D-CT |
Trachea and BM | No | Symptomatic therapy | Survived (12 months) |
| 9 | Bronchoscopy 3D-CT |
Trachea and BM | Asthma and bronchiectasis | Trachea stent | Survived (12 months) |
| 10 | Bronchoscopy 3D-CT |
Trachea and RM | COPD | Symptomatic therapy | Survived (120 months) |
Note: 3D-CT: Three-Dimensional Computed Tomography; BM: Both Main Bronchi; LM: Left Main Bronchus; RM: Right Main Bronchus.
Table 3. Diagnosis methods, etiology, and prognosis of ten patients.
The application of bronchodilator can reduce the symptoms to a certain extent. Tracheal stents were placed in three patients but declined in seven because of concerns about side effects. All patients survived after a follow-up of 3-120 months.
Seven out of ten patients had lung function tests. The results showed that five patients had obstructive ventilation function disturbance, one patient had mixed ventilation dysfunction, and the remaining one had no lung function impairment (Table 4).
| Patient no. | FVC% | FEV1% | FEV1/FVC | RV% | RV/TLC | DLCO% | R% |
|---|---|---|---|---|---|---|---|
| 1 | 58.2 | 21.8 | 35.2 | 379.8 | 77.59 | 79.2 | 293.7 |
| 2 | 87.3 | 46.4 | 51.8 | 176.4 | 55.9 | 78.2 | 187.4 |
| 3 | 79.3 | 39.0 | 40.39 | 180.3 | 60.0 | 83.2 | 313.5 |
| 4 | 95.7 | 43.5 | 38.03 | 157.8 | 39.49 | 103.6 | 188.4 |
| 5 | 71.8 | 64 | 71.37 | 185.8 | 59.55 | 61.7 | 264.3 |
| 7 | 96.9 | 97.0 | 98.3 | 101.3 | 94.0 | 158.9 | |
| 8 | 75.4 | 25.3 | 26.17 |
Note: DLCO: Carbon monoxide Diffusing Capacity; FEV1: Forced Expiratory Volume in 1 second; FVC: Forced Vital Capacity; R: Airway Resistance; RV:Residual Volume; TLC: Total Lung Capacity.
Table 4. Pulmonary functions of the patients.
Discussion
In our study, the median onset age of TBM was 55 years, which is consistent with previous reports that adult TBM often occurs in middle-aged and elderly patients [8]. The course of TBM varies greatly (from a few months to more than ten years), which may be related to its wide range of etiologies. Adult TBM usually occurs in the normally developed trachea, and its main causes are chronic airway inflammation, mechanical causes, and so on [4,11-13]. In this study, the etiologies of TBM included COPD, tracheobronchial tuberculosis, bronchiectasis, relapsing polychondritis, and chronic bronchitis. The main etiologies in our hospital were COPD and tracheobronchial tuberculosis, which differed from those in western countries.
In some countries, the main cause of adult TBM is COPD, but the two are likely to be confused with each other due to similar symptoms and pulmonary function [8]. One study showed that 53% of patients with COPD had TBM on their expiratory CT scan [16]. Both smoking and chronic airway inflammation can lead to changes in airway structure, resulting in bronchial cartilage deficiency [17]. The pathogenesis of TBM in chronic bronchitis is like that in COPD. In 2018, The China Pulmonary Health (CPH) [18]study led by Chen-Wang showed that the incidence rate of COPD was 13.7% among people over 40 years old, indicating that there are approximately 100 million patients with COPD in China. However, there are few case reports about TBM secondary to COPD in China due to insufficient attention. Therefore, we suggest that TBM should be suspected if COPD patients have poor or no response to rational bronchodilators and glucocorticoids. More attention should be paid to dynamic multidetector CT with 3-dimensional imaging and flow-volume curve. Bronchoscopy can be performed to assist the diagnosis if the patient is in good condition.
Another main cause of TBM was tracheobronchial tuberculosis in this study. The two patients had no history of other diseases, except tracheobronchial tuberculosis, which was the most common concurrent diseases in China. Mycobacterium tuberculosis can involve the bronchial wall and destroy the bronchial cartilage, resulting in thickening and fibrosis of the bronchial wall [19]. Bronchial cartilage destruction and fibrosis lead to TBM. China is the third largest country with high burden of tuberculosis in the world, there are nearly 800,000 new cases of tuberculosis every year in China [20]. More than 50% of patients with active pulmonary tuberculosis were endobronchial tuberculosis [21]. It is surmised that there are an abundant number of patients with TBM secondary to tracheobronchial tuberculosis. However, the morbidity of TBM secondary to tracheobronchial tuberculosis is substantially undervalued due to pulmonologists' insufficient recognition of TBM in China. Therefore, a longterm prospective multicenter study on the morbidity of TBM secondary to tracheobronchial tuberculosis is needed.
The main etiologies of TBM in western countries are COPD, asthma, Mounier- Kuhn syndrome, and recurrent polychondritis. In our study, COPD and tracheobronchial tuberculosis were the main etiologies of TBM. Moreover, the morbidity of TBM is substantially undervalued due to insufficient recognition and epidemiological survey results.
The main symptoms of TBM patients are chest distress and cough, which consistent with previous studies [22], are common in obstructive airway disease, leading to TBM misdiagnosis as COPD or asthma. Although chest distress and cough are not the specific clinical symptoms of TBM, they may be indications of TBM. Therefore, in clinical practice, it is needed to consider whether patients with TBM, if the response to conventional treatment is not good for COPD and asthma.
The diagnosis of symptomatic TBM can be complex. The clinical presentation of TBM is nonspecific and like that of other common respiratory diseases. It is important to have a high degree of clinical suspicion especially when the symptoms are caused by COPD and asthma or conventional treatment fails. For TBM, pulmonary function test is neither sensitive nor specific, and main airway obstruction shown in flow-volume curve may be a hint of TBM. Chest distress and cough, inspiratory wheezing rale in auscultation and flow-volume curve are beneficial supplement and hint for the diagnosis of large airway obstruction.
In our study, all patients were given symptomatic treatment, and their symptoms were improved to some extent. Some patients chose conservative treatment, and three patients were inserted with tracheal stents. Despite severe symptoms, some patients refused tracheobronchial stenting because of worry about the side effects. None of the 10 patients received surgical treatment.
Medical management, stenting and surgical treatment are the main treatment methods for TBM. Expectorant treatment is an effective management means and almost all patients with TBM will benefit from airway mucus clearance [23,24]. Tracheobronchial stenting can reduce the symptoms of chest distress and improve lung function. However, it is associated with a higher risk of granulation tissue formation as well as stent fracture, migration, or blockage [12,25]. Therefore, tracheobronchial stents should only be used when tracheobronchoplasty is not feasible or is contraindicated [12]. The definitive method for patients with TBM is surgical treatment [23,26]. In our study, all patients were given symptomatic treatment, and their symptoms were improved to some extent. Some patients chose conservative treatment, and three patients were inserted with tracheal stents. Despite severe symptoms, some patients refused tracheobronchial stenting because of worrying about the side effects. None of the ten patients received surgical treatment.
There are diverse etiologies of TBM in adults. Different primary diseases have different outcome and survival time. The long-term outcomes of TBM in adults with different etiologies are unclear.
The main limitation of this study is that the number of cases was only ten, and some etiologies were not summarized. However, Shanghai, as the representative city of East Asia, is a large city in eastern China with a population of more than 20 million. Patients in Shanghai, in addition to residents, are from everywhere of Chinese mainland. The etiologies of TBM in this study included COPD (Case 2, 6 and 10), tracheobronchial tuberculosis (Cases 3 and 4), relapsing polychondritis (Case 1), Chronic bronchitis (Case 5) and Asthma and bronchiectasis (Case 9). China has a large population and the incidence of COPD and tracheobronchial tuberculosis, indicating that the number of patients with COPD and tracheobronchial tuberculosis are large. The results of this study still have considerable clinical value. Large-scale epidemiological investigation about TBM remains to be conducted in the future.
Conclusion
Ten patients were retrospectively analyzed in this study, and the etiologies of TBM included COPD, tracheobronchial tuberculosis, chronic bronchitis, asthma, bronchiectasis and relapsing polychondritis. In China, main etiologies of TBM may be COPD and tracheobronchial tuberculosis, which are different from those of western countries and seriously underestimated.
Funding
This work Supported in part by grants from the Advanced and Appropriate Technology Promotion Project of Shanghai Municipal Health Commission (No. 2019SY055).
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Murgu SD, Colt HG. Tracheobronchomalacia and excessive dynamic airway collapse. Respirology 2006; 11: 388-406.
[Crossref] [Google Scholar] [PubMed]
- Hammond K, Ghori UK, Musani AI. Tracheobronchomalacia and excessive dynamic airway collapse. Clin Chest Med 2018; 39: 223-228.
[Crossref] [Google Scholar] [PubMed]
- Nemes RM, Postolache P, Cojocaru DC, Nitu MF. Tracheomalacia in children and adults-not so rare as expected. Rev Med Chir Soc Med Nat Iasi 2014; 118: 608-611.
[Google Scholar] [PubMed]
- Kamran A, Zendejas B, Jennings RW. Current concepts in tracheobronchomalacia: Diagnosis and treatment. Semin Pediatr Surg 2021; 30: 151062.
[Crossref] [Google Scholar] [PubMed]
- Xia Y, Huang Y, Li QB, Luo ZX, Liu EM, Chen KH, Tang W, Bo N, Zhao H, Yuan XP. Analysis of 53 cases with bronchoscopically confirmed pediatric tracheobronchomalacia. Zhonghua Er Ke Za Zhi 2007; 45: 96-99.
[Google Scholar] [PubMed]
- Ridge CA, O'Donnell C R, Lee EY, Majid A, Boiselle PM. Tracheobronchomalacia: Current concepts and controversies. J Thorac Imaging 2011; 26: 278-289.
[Crossref] [Google Scholar] [PubMed]
- Matus I, Richter W, Mani SB. Awareness, competencies, and practice patterns in tracheobronchomalacia: A survey of pulmonologists. J Bronchology Interv Pulmonol 2016; 23: 131-137.
[Crossref] [Google Scholar] [PubMed]
- Majid A, Fernández L, Fernández-Bussy S, Herth F, Ernst A. Tracheobronchomalacia. Arch Bronconeumol 2010; 46: 196-202.
[Crossref]
- Dubey S, Gelder C, Pink G, Ali A, Taylor C, Shakespeare J, Townsend S, Murphy P, Hart N, D'Cruz D. Respiratory subtype of relapsing polychondritis frequently presents as difficult asthma: a descriptive study of respiratory involvement in relapsing polychondritis with 13 patients from a single UK centre. ERJ Open Res 2021; 7: 00170-2020.
[Crossref] [Google Scholar] [PubMed]
- Hong G, Kim H. Clinical characteristics and treatment outcomes of patients with relapsing polychondritis with airway involvement. Clin Rheumatol 2013; 32: 1329-1335.
[Crossref] [Google Scholar] [PubMed]
- Schmitt P, Dalar L, Jouneau S, Toublanc B, Camuset J, Chatte G, Cellerin L, Dutau H, Sanchez S, Sauvage M. Respiratory conditions associated with tracheobronchomegaly (mounier-kuhn syndrome): A study of seventeen cases. Respiration 2016; 91: 281-287.
[Crossref] [Google Scholar] [PubMed]
- Kheir F, Majid A. Tracheobronchomalacia and excessive dynamic airway collapse: Medical and surgical treatment. Semin Respir Crit Care Med 2018; 39: 667-673.
[Crossref] [Google Scholar] [PubMed]
- Choi S, Lawlor C, Rahbar R, Jennings R. Diagnosis, classification, and management of pediatric tracheobronchomalacia: A review. JAMA Otolaryngol Head Neck Surg 2019; 145: 265-275.
[Crossref] [Google Scholar] [PubMed]
- Ngerncham M, Lee EY, Zurakowski D, Tracy DA, Jennings R. Tracheobronchomalacia in pediatric patients with esophageal atresia: comparison of diagnostic laryngoscopy/bronchoscopy and dynamic airway multidetector computed tomography. J Pediatr Surg 2015; 50: 402-407.
[Crossref] [Google Scholar] [PubMed]
- Gangadharan SP, Bakhos CT, Majid A, Kent MS, Michaud G, Ernst A, Ashiku SK, deCamp MM. Technical aspects and outcomes of tracheobronchoplasty for severe tracheobronchomalacia. Ann Thorac Surg 2011; 91: 1574-1580.
[Crossref] [Google Scholar] [PubMed]
- Sverzellati N, Rastelli A, Chetta A, Schembri V, Fasano L, Pacilli AM, Di Scioscio V, Bartalena T, de Filippo M, Zompatori M. Airway malacia in chronic obstructive pulmonary disease: Prevalence, morphology and relationship with emphysema, bronchiectasis and bronchial wall thickening. Eur Radiol 2009; 19: 1669-1678.
[Crossref] [Google Scholar] [PubMed]
- Ernst A, Odell DD, Michaud G, Majid A, Herth FFJ, Gangadharan SP. Central airway stabilization for tracheobronchomalacia improves quality of life in patients with COPD. Chest 2011; 140: 1162-1168.
[Crossref] [Google Scholar] [PubMed]
- Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, Kang J, Ran P, Shen H, Wen F. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): A national cross-sectional study. Lancet 2018; 391: 1706-1717.
[Crossref] [Google Scholar] [PubMed]
- Iwamoto Y, Miyazawa T, Kurimoto N, Miyazu Y, Ishida A, Matsuo K, Watanabe Y. Interventional bronchoscopy in the management of airway stenosis due to tracheobronchial tuberculosis. Chest 2004; 126: 1344-1352.
[Crossref] [Google Scholar] [PubMed]
- Harding E. WHO global progress report on tuberculosis elimination. Lancet Respir Med 2020; 8: 19.
[Crossref] [Google Scholar] [PubMed]
- Jung SS, Park HS, Kim JO, Kim SY. Incidence and clinical predictors of endobronchial tuberculosis in patients with pulmonary tuberculosis. Respirology 2015; 20: 488-495.
[Crossref] [Google Scholar] [PubMed]
- Hoffmann H, Gompelmann D, Heußel CP, Dienemann H, Eberhardt R. Tracheobronchoplasty for severe diffuse tracheomalacia. Zentralbl Chir 2016; 141: S35-S42.
[Crossref] [Google Scholar] [PubMed]
- Kamran A, Jennings RW. Tracheomalacia and tracheobronchomalacia in pediatrics: An overview of evaluation, medical management, and surgical treatment. Front Pediatr 2019; 7: 512.
[Crossref] [Google Scholar] [PubMed]
- Kamran A, Baird CW, Jennings RW. Tracheobronchomalacia, tracheobronchial compression, and tracheobronchial malformations: Diagnostic and treatment strategies. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2020; 23: 53-61.
[Crossref] [Google Scholar] [PubMed]
- Biswas A, Jantz MA, Sriram PS, Mehta HJ. Tracheobronchomalacia. Dis Mon 2017; 63: 287-302.
- McGinn J, Herbert B, Maloney A, Patton B, Lazzaro R. Quality of life outcomes in tracheobronchomalacia surgery. J Thorac Dis 2020; 12: 6925-6930.
[Crossref] [Google Scholar] [PubMed]