Research Article - Current Pediatric Research (2022) Volume 26, Issue 3
Turkish validity and reliability study of the Montreal children's hospital feeding scale.
Ibrahim Dogru1, Gulay Manav2, Pelin Uymaz3*
1Department of Pediatric Nursing, Specialist Uskudar University, ?stanbul, Turkey
2Department of Pediatric Nursing, Mugla Sitki Kocman Un?versity, Mugla, Turkey
3Department of Pediatric Nursing, Alanya Alaaddin Keykubat University, Alanya, Turkey
- Corresponding Author:
- Pelin Uymaz
Department of Pediatric Nursing, Alanya Alaaddin Keykubat University, Alanya, Turkey
E-mail: pelin.uymaz@alanya.edu.tr
Received: 03 March, 2022, Manuscript No. AAJCP-22-51331; Editor assigned: 04 March, 2022, PreQC No. AAJCP-22-51331 (PQ); Reviewed: 14 March, 2022, QC No. AAJCP-22-51331; Revised: 22 March, 2022, Manuscript No. AAJCP-22-51331 (R); Published: 31 March, 2022, DOI:10.35841/0971-9032.26.1.1289-1296.
Abstract
This study aims to evaluate and determine psychometric features, factor structure and internal validity of the Turkish version of Montreal Children’s Hospital Feeding Scale (MCH-Feeding Scale). The study started with 200 participants, but completed with 166 of them because of the drop-outs during test-retest period. The study, which used no sampling, was conducted with parents who accepted to participate. Of the participating children, 53.6% were female and 46.4% were male. To collect the data, the family questionnaire form (14 items) and the MCH-feeding scale (14 items) were used. The 14 items of the MCH-feeding scale were studied on factor analysis. Factor loads of all items were above 0.30 and the explained variance was found to be 34.598%. Therefore, no items were removed from the scale and a single sub-dimensional structure was accepted. Several indices were used to examine the appropriateness of the MCH-feeding scale model. Of these indices, x2/SD was 1.88, GFI was 0.97, AGFI was 0.95, CFI was 1.00, RMSEA was 0.073, and SRMR was 0.071. All related index values were found to be at the desired range. The cronbach α coefficient of the MCH-feeding scale was 0.838, and item-total correlation values for all items of the scale were found to be positive. The Turkish version of the MCH-feeding scale had a good structure and validity. According to the results of the scale, it is suitable to be used in further research to be conducted in Turkey.
Keywords
Child, Nutrition, In-adequate nutrition, Malnutrition, Eating disorders.
Introduction
Importance and description of the problem
Improving proper and balanced nutrition is important for individuals’ health status and economic status. Proper and balanced nutrition is a main requirement for a healthy life. It becomes possible for individuals who eat regularly to attain goals such as protecting their health, maintaining their health status, increasing their quality of life, and adopting these behaviors. Children should consume varied foods based on their body needs to ensure adequate growth and meet their energy needs. Nutrition condition not only causes changes in children’ health in the short term, but it can show its effects in the long term too and children with adequate and balanced nutrition, starting from fetal life, have less disease, less development and growth retardation, and appropriate intelligence development [1,2].
However, those children who do not consume nutrients as needed show growth and developmental retardation. Children’s nutritional habits depend on many factors, which are environmental, cultural, social, economic and individual factors. Among these factors, environment and culture have an important effect on pre-school children’s adopting healthy nutrition and healthy living habits. It is seen that family members, peers, the use of Internet, cartoons and TV advertisements have a major effect in preschool children’s food selection. The studies conducted in Turkey show that the majority of children do not have breakfast but consume snacks during their time at school. However, they do not consume enough necessary nutrients such as fruits and vegetables.
Attitudes of parents, an environmental factor, towards nutrition have an important effect on the formation of obesity in children. Their attitudes towards nutrition affect not only children themselves but also their weighing status. Parents’ oppressive and controlling attitudes regarding nutrition of children result in the failure of development of children’s responsibilities on nutrition. Meal times and food amounts that are determined by parents wipe out the feeling of hunger and satiety in children. As a result, children cannot be fed as required by their body, which affects their weight. One of the oppressions that parents put on their children’s nutrition is to restrict certain food (junk food, etc.) or to force them to consume certain food. Such oppression may lead children to consume less healthy food and more unhealthy food. Individual factors are among developmental period of children.
Essential nutrient of 0-6 month infants is breast milk. Complementary food/nutritional supplements should be given to those infants after the sixth month. The period of transition to solid food depends on children. The infants’ neuromuscular, digestive, excretory and immune systems must reach the necessary maturity for solid food. A child of one year age can consume the same food as the family members consume. Because growth is fast in the period of 0-1 year of age, nutrition is very important. Nutrition-related problems that may occur at this period become harder to fix, so children should be taught to have proper nutritional habits in this period. A newborn should be exclusively breastfed for the first six months, but in case of any obstacles to breastfeeding, the infant should be provided with formulas.
According to Turkey demographic and health survey 2018 (TNSA), 41% of infants fewer than six months are exclusively breastfed. As children grew, the percentage of exclusively breastfeeding decreased to 59% in 0-1 month old infants, to 45% in 2-3 months old infants and to 14% in 4-5 months old infants. Giving feeding bottle and false breast is not recommended. Suction power in infants using dummy decreases, thus production of milk decreases and the infant has to leave the breast earlier [3-6]. Supplementary foods are given to infants after their first six months. The start of complementary food is closely related to the maturation of the infant’s neuromuscular, digestive, excretory and immune system. After starting complementary food, infants should be breastfed at least eight times a day when they want. The amount and variety of food given to children should be increased as children aged 1-3 years grow. Nutrients should be given according to children’s dentition and chewing power.
Children at this age range should be given soft food. Gradually, grain and tough nutrients are added to their diet. Children should be directed to consume foods without being intervened unnecessarily. Children at this age should not consume foods that they cannot take so that they do not lose their interest in them. Otherwise, this may cause them to obstinate and refuse such foods. In such cases, children should be expected to eat by themselves or show that they are hungry. It should be reminded that children aged 1-3 years may put anything in their mouth, so they should be under surveillance. The preschool period (3-6 years) is deemed an important period in which nutritional habits are underlain. Children of this age group can eat by themselves without any help. However, it is natural that children seek help while eating until five years of age. Children of this age group do not like much vegetable food. They prefer foods that they can eat by their hands. They are sensitive to strong odors and flavors. Oppressive behaviors towards children regarding food may result in backlash and cause them to refuse eating. They may consume food, which they refuse to eat home, with their peers [7].
There are very few studies conducted on food consumption in children of this age group. Studies have focused on school age and adolescence mostly. Scales that are frequently used for nutrition in Turkey are as follows; feeding attitude scale for infants to families, child nutrition questionnaire for school-aged children, scale to identify adolescents’ nutrition knowledge and eating behaviors for adolescents and child nutrition scale for parents. Growth of undernourished and malnourished children slows down. In these children whose development retards, developmental disorders, the risk of getting sick and mortality rates increase and leave lasting marks in their future lives. Inadequate vitamins may cause simple goiter and negatively affect dental health. Besides, new studies have shown that there is an increase in hyperlipidemia and hypertension due to malnutrition even in the absence of obesity. Hyperlipidemia and hypertension are reasons of coronary heart diseases.
Undernourished and malnourished children have inadequate physical power and low intelligence levels in future life. Therefore, economic, cultural and educational problems become greater. Nutrition-based problems cause important problems in children; it is seen that 25%-50% of infants and young children have nutritional problems. Irregular and unbalanced nutrition not only causes physical problems in children, but also affects their mental development. Nutritional problems are defined as global issues [8-10]. These problems are not seen only in underdeveloped countries but also in developing countries. According to the report of the World Health Organization (WHO), the incidence of shortness is 29% in Egypt, 17% in Malaysia and 16% in Mexico, 8% in Jordan and 7% in Brazil. There are great differences regarding nutritional problems between regions of Turkey and in urban-rural settlements. TNSA divided Turkey into five main sections in the 2008 study.
According to the results of the present study, 20.9% of children aged 0-18 years in the “East” region are short, while the prevalence of shortness in this age group is 7.6% in the “West” [11,12]. According to the results of this study, shortness is seen more in certain provinces and districts. According to TNSA, 3.2% of children under five years old are severely short, while 10.3% of them are short. In previous studies, the shortness rate of children under five years old was 16% in 1998 and 12.2% in 2003. Shortness is a state of being shorter for the related age, which is an indicator of inadequate unbalanced nutrition. Lower weight in proportion to height is defined as slimness. Slimness is seen in 1% of the children living in Turkey. In other words, their body weight is low in proportion to their height due to nutritional deficiencies. Many infants and children suffer from nutrition-related disability, illness or developmental delay. According to 2018 TNSA data, 25% of the general population of Turkey consists of children under 15 years old.
The same study has shown that 6% of 5 children under five years old in Turkey are short for their age, and 1.5% is severely short. The TNSA 2018 showed that the percentages of shortness were 8% in rural areas, 8% in the Eastern region of Turkey, 12% in lower-income population, and 9% in children whose mothers are uneducated. Since the TNSA 2008 data, there has been a regular decrease in the rate of shortness. The prevalence of shortness decreased from 12% to 6% in the last 10 years. Similarly, there has been a decrease in the rate of overweight children under five years old [13]. The prevalence of overweight in those children decreased from 11% to 8% in the last 5 years. The prevalence of slimness in children under five years old has increased from 1% to 2%. Another nutritional problem in children is obesity. Obesity is one of the chronic diseases seen in childhood today.
Being an important public health problem, obesity affects 25%-30% of children and adolescents. Obesity becomes dangerous in childhood and its prevalence increases every year. Studies have reported that if a child becomes obese in childhood is more likely to be obese in adulthood compared to a child with a normal weight in childhood. Parents and home environment have a major effect in children’s growth and development. Children acquire eating behaviors from their parents and take them as role models. Determination of child feeding behaviors and attitudes of parents in home environment are important sources of information for health-care professionals to prevent and treat any potential nutrition-driven diseases. For this, valid and reliable data collection tools are needed. The present study aims to early detect nutritional problems and to evaluate Turkish validity and reliability of the Montreal Children’s Hospital feeding scale (MCH-Feeding Scale) developed by Ramsay et al. [14,15].
Aim of the Study
The aim to find out whether the MCH feeding scale is a valid and reliable data collection tool for children in Turkey.
Research type
This is a methodological study.
Setting and time period of the study
The study was conducted in preschool institutions in Hatay province of Turkey between November 2018 and February 2019. The region of the selected schools has varied socioeconomic characteristics with varied populations. Four schools were selected from different regions to create a sample that varied in terms of socioeconomic levels, gender and health status. One of the schools providing dual education, Cemil MeriC preschool, locates in Antakya/Hatay. It hosts 148 students. Another school providing dual education, Sabiha GOkCen preschool, locates in Antakya/Hatay. This school hosts 322 students. Another school providing dual education Saraykent 125. Yil preschool, locates in Antakya/Hatay. It hosts 173 students. The final school providing dual education 75. Yil preschool, also locates in Antakya/Hatay. It hosts 460 students [16].
Population and research sample
The population of the research included the parents of 166 pre-school children studying in 4 public pre-schools in Hatay. The MCH-Feeding Scale includes 14 items. It is recommended to include 10 participants for each item in the scale for the scale studies to be carried out. Considering the potential drop-outs during the test-retest application, the number of the sample was distributed to at least 200 parents, but after the drop-outs from the test-retest, the study was continued with 166 people. No sample selection was made in the study, which was conducted with parents who agreed to participate voluntarily [17,18].
Data collection tools
•To collect the data, the Family Questionnaire (FQ) and the MCH-feeding scale were used.
•The FQ included 14 questions. These questions aimed to collect data on demographic attributes, social impact, health experiences and environmental sources [19].
MCH-feeding scale
This scale was developed by Ramsay et al. in 2011 to quickly identify nutritional problems. The scale sections consisted of how parents decide their children’s meal time, how worried they are about what their children eat, their appetite, which period of the meal they refuse to eat, duration of the meal, their behaviors at mealtimes, whether they show reaction to certain foods, whether they keep their food in their mouth before swallowing, whether they use different methods at mealtimes, whether there is force to eat, chewing power, growth status, nutritional status affecting their relationship with their parents and nutritional status affecting family relations.
The scale comprises a set of steps including the following nutritional areas: Oral motor (items 8 and 11), verbal sensory (items 7 and 8), and appetite (items 3 and 4), which makes a total of 14 items. Other topics are related to nutrition (items 1, 2 and 12), mealtime behaviors (items 6 and 8), maternal strategies used (items 5, 9 and 10), and family reactions to their children’s nutrition (items 13 and 14). Scaling and scoring of 22 questions: Each question was scaled based on the seven-point Likert type scale with connection points in both ends. Seven items are scored from negative to positive, while the other is scored from positive to negative. The primary feeder marks each item based on the frequency or difficulty level of a certain behavior or based on parenting level.
The total eating problem score is obtained with the addition of the scores for each item after reversing the scores from the seven items from negative to positive. Based on the scale results, the minimum obtainable score is 14 and the maximum is 98 points. As the score gets closer to 98, nutritional problem decreases [20-25]. To conduct the study and collect the data, permission was obtained from UskUdar university ethics committee and the institutions where the study was to be conducted. The parents of the participating children were informed about the aim of the study and provided their informed consent. Based on self-report, the researcher explained the questions to the parents, answered any questions coming from them and collected the data through face-to-face interviews.
Language validity and translation process
The scale was translated from the original language (English) into Turkish by three translators who were proficient in English. The translators were not informed about the scale. Appropriate statements for the scale were revised, so the most comprehensible and appropriate Turkish form was created. The Turkish scale was back translated into English by other translators. The original form and translated form of the scale were compared, checked whether there were any semantic differences between the two by the researcher and the Turkish form was finalized.
Content validity
The content validity index of the scale was determined by the predetermined experts. The result of the content validity index, used to analyze the relevance of the opinions of five doctors, three nurses and two dieticians who were consulted at this stage, showed the consistency between the scores.
Preliminary application
After the evaluation by experts and language equivalence of the scale, pre-application was made with the parents of 15 children from the four schools to evaluate the comprehensibility of the statements in the scale.
Test-retest application
After the scale was administered to parents twice, three weeks apart, the scale’s test-retest reliability coefficient was evaluated. Doing test-retest, time-dependent reliability of the scale items was tested.
Data analysis
The statistical analyses were made using SPSS for Windows 22 and LISREL 8.80 software. Descriptive statistics were used to determine the attributes of the sample. The content validity index was used to test the content validity of the scale. CFA and hypothesis test were used for the construct validity. The CFA results were examined to determine fit indices of the scales. PATH diagrams and modifications were examined. The acceptable fit indices were p>0.05, df ≤ 2 perfect fit, df ≤ 5 moderate fit, RMSEA ≤ 0.05 perfect fit, RMSEA ≤ 0.08 good fit, SRMR ≤ 0.8 good fit, and CFI ≥ 0.90 good fit.”
The internal consistency was tested using Pearson correlation and Cronbach’s alpha. The Cronbach’s alpha coefficient shows whether the items of a scale measure a single trait or not and the relationship of the items with the study. A Cronbach’s alpha value less than 0.40 shows that the scale is not reliable, however the reliability of the scale increases as the Cronbach’s alpha approaches to 1. Item-total correlations in the scale or in sub-dimensions>0.25 are considered appropriate. Test-retest was used to evaluate reliability of the scale. The total score and factor total scores of the first application, as well as the total score and factor total scores of the scale administered two weeks later, were examined using Pearson correlation analysis. The acceptable rate of test-retest correlation was>0.40 [26].
Study Inclusion Criteria
Criteria for children
•Being between 6 months and 6 years of age
•Being enrolled in a preschool
•Having a parent
•Living with the parents criteria for parents
•Being literate of Turkish
Ethical consideration
Permission was obtained via e-mail from Maria Ramsay to conduct validity and reliability study of the MCH–feeding scale. Along with the scale, the necessary information about the study was sent to Maria Ramsay via e-mail. Before launching the study, approval was obtained from the UskUdar University, non-invasive research ethics committee in the meeting No.10 on 9/3/2018 (Annex-5). Besides, permission was obtained from Hatay governorship provincial directorate for National Education, to which the research schools were affiliated, with the petition No. 32889839-605.01-E.20635351 (Annex-6) dated 10.31.2018 [27,28].
Strengths of the Study
The scales that evaluate nutrition of preschool and school children together are available in Turkey. However, no scale was found regarding preschool children only. This is the first study to integrate the MCH-feeding scale with Turkish society in nursing field in Turkey (Table 1).
| n | Min. | Max. | Mean | SD | % | |
|---|---|---|---|---|---|---|
| Child’s general health status | ||||||
| Good | 111 | 22.3 | ||||
| Moderate | 18 | 66.9 | ||||
| Perfect | 37 | 10.8 | ||||
| Numeric data | ||||||
| Number of people in the family | 1 | 7 | 4.07 | 0.93 | ||
| Age | 2 | 6 | 5.04 | 0.66 | ||
| Height | 90 | 198 | 111.84 | 10.25 | ||
| Weight | 13 | 32 | 20.07 | 3.96 | ||
| Mother’s weight | 45 | 100 | 65.73 | 10.03 | ||
| Mother’s height | 147 | 188 | 163.11 | 6.3 | ||
| Father’s weight | 55 | 120 | 81.69 | 11.91 | ||
| Father’s height | 100 | 192 | 174.18 | 8.49 | ||
Table 1. Distribution of descriptive attributes of the MCH-feeding scale participants.
As shown in Table 1, 53.6% of the children are females, parents of 95.8% are alive and living together 57.8% have economic difficulties at a moderate level, and mothers of 34.9% have undergraduate degree or higher. Fathers of 35.5% of the children had high school education, and 65.1% maternal health status, 65.7% paternal health status and 66.9% child health status were at a “good” level. The mean number of people living in the family is 4.07 ± 0.93, the mean age is 5.04 ± 0.66, the mean height is 111.84 ± 10.25, and the mean weight is 20.07 ± 3.96. The mean weight of mothers was 65.73 ± 10.03, the mean height of mothers was 163.11 ± 6.30, the mean weight of father was 81.69 ± 11.91, and the mean height of father was 1.74.18 ± 8.49. In this study, the MCH-feeding scale was examined in three different ways, which were content validity, construct validity and internal validity, to be examined in terms of validity and reliability in Turkish.
Findings from content validity
After the translation of the MCH-nutrition scale, whose validity and reliability study was done, the scale was presented to a group of 10 experts in order to evaluate its cultural equivalence dimension and ensure its content validity. Content validity scores of all items ranged from 0.8 to 1.0 with the use of the Davis technique for content validity analysis. Based on the results, no item was excluded from the scale.
Findings from construct validity
Factor analysis was made for construct validity of the MCH-feeding scale to more clearly and reliably determine the study results. After the adequate sample size is determined, factor analysis can be made. The Kaiser Meyer Olkin (KMO) analysis was made to determine the adequacy of the sample size and Bartlett’s test was used to test significance of the correlation between variables. The KMO was found to be 0.863, which indicates its suitability for main components and the adequacy of the sample size. Results from the Bartlett’s test also show that the (x2=699.186; p=0.000) values relate to each other and indicate their suitability with factor analysis. The anti-image correlation was examined in the study, aiming to determine suitability of the study data for factor analysis.
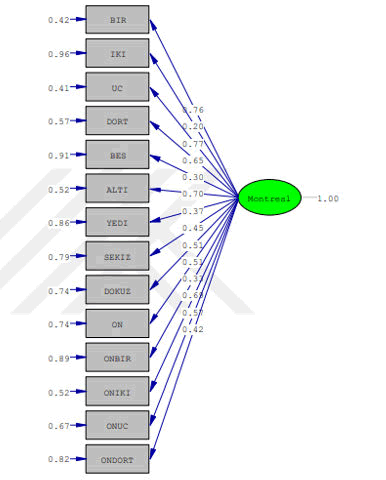
Confirmatory factor analysis
The MCH-feeding scale, similar to its original version, consisted of a single sub-dimension. The factor loads of the items were above 0.30, and the explained variance was 34.598% for the total scale. Therefore, no item was excluded from the scale and it was taken as a single sub-dimension as in the original one. Structural equation modeling was made with confirmatory factor analysis to reach clearer and more precise findings after the explanatory factor analysis.
Findings from confirmatory factor analysis
Different indices were used to analyze appropriateness of the MCH-Feeding Scale model. Of the indices, x2/SD value was 1.88, GFI was 0.97, AGFI was 0.95, CFI was 1.00, RMSEA was 0.073 and SRMR was 0.071. All of the related fit indices were at the desired ranges. The factor load in the model ranged between 0.20 and 0.76. T-values of the model items were found to be above 1.96 (Table 2).
| Index | Normal value | Acceptable value | Value found |
|---|---|---|---|
| x2/SD | <2 | <5 | 1.88 |
| GFI | >0.95 | >0.90 | 0.97 |
| AGFI | >0.95 | >0.90 | 0.95 |
| CFI | >0.95 | >0.90 | 1 |
| RMSEA | <0.05 | <0.08 | 0.073 |
| SRMR | <0.05 | <0.08 | 0.071 |
Table 2. Fit index values of the MCH-feeding scale normal and acceptable fit values.
The Cronbach's alpha coefficient of the MCH-feeding scale was 0.838 and the item-total correlation values of all items were positive. Also, when items deleted from the scale, the Cronbach's alpha coefficient did not change significantly. Thus, no item was excluded from the scale. The MCH-feeding scale lower and upper 27% comparison results were statistically significant (p<0.05). This finding is an indicator of distinctiveness power of the scale.
| Items | Mean | SD | Item-total correlation | If item deleted α |
|---|---|---|---|---|
| How do you experience your meals with your child? | 5.05 | 1.69 | 0.683 | 0.815 |
| How much do you care about your child’s nutrition? | 6.28 | 1.46 | 0.228 | 0.84 |
| How is your child’s appetite (hunger)? | 4.95 | 1.74 | 0.692 | 0.814 |
| When does your child start to refuse eating during mealtime? | 4.71 | 2.19 | 0.563 | 0.821 |
| How long does it take for your child to eat? | 5.66 | 1.38 | 0.295 | 0.837 |
| How does your child behave while eating? | 4.91 | 1.88 | 0.611 | 0.818 |
| Does your child show reactions such as spitting, retching, or vomiting to certain foods? | 4.99 | 2.41 | 0.375 | 0.836 |
| Does your child keep food in his/her mouth before swallowing it or chew for long time? | 5.07 | 2.27 | 0.45 | 0.83 |
| Do you have to use toys or television for diverting your child so that he/she eats? | 5.02 | 2.32 | 0.476 | 0.828 |
| Do you have to force your child to eat or drink? | 3.89 | 2.36 | 0.438 | 0.831 |
| How is your child’s chewing (or suction) power? | 6.42 | 1.12 | 0.312 | 0.836 |
| How do you evaluate your child’s growth? | 5.37 | 1.72 | 0.637 | 0.818 |
| How your child does eating habits affect the relationship between you and your child? | 5.32 | 1.78 | 0.566 | 0.822 |
| How your child does eating habits affect the relationship between your spouse and your child? | 5.81 | 1.67 | 0.382 | 0.833 |
| Total MCH-feeding scale Cronbach’s alpha | 0.838 | |||
Table 3. The MCH-feeding scale item-total correlations and Cronbach’s alpha coefficients (n=166).
The MCH-feeding scale test-retest comparison results were statistically significant (p<0.05). A positive and significant correlation (r=0.982) was found between the first and the second measurements. The mean scores from the scale were 73.45 ± 15.05 and the scores ranged between 31 and 98. The highest score was obtained from “How is your child’s chewing (or suction) power?” whereas the lowest was obtained from “Do you have to force your child to eat or drink?”
Results
The study was conducted in preschool institutions in Hatay province of Turkey between November 2018 and February 2019. The region of the selected schools has varied socioeconomic characteristics with varied populations. Four schools were selected from different regions to create a sample that varied in terms of socioeconomic levels, gender and health status. In line with the data obtained from this study, conducted to determine Turkish validity and reliability of the MCH-feeding scale, the following results were obtained.
•The study group consisted of 166 children. Of them, 53.6% were female and 46.4% were male. The mean age was 5.04 and the mean weight was 20.07.
•The MCH-feeding scale was found to be valid and reliable according to the opinions of the experts and the statistical results, and its Turkish version could be used by the Turkish society to measure the nutritional status of children aged between 6 months and 6 years.
•The content validity scores of the MCH-feeding scale ranged from 0.8 to 1.0. Overall, the content validity score of the scale was 0.9.
•The item-total correlation values for all items of the scale were found to be positive in the MCH-feeding scale.
•The Cronbach’s alpha coefficient that shows internal validity and reliability of the MCH-feeding scale was 0.83. The Turkish version of the MCH-Feeding Scale had high validity and reliability.
•The Turkish version of the MCH-Feeding Scale had high validity and reliability.
Suggestions
The Montreal feeding scale whose Turkish validity and reliability study was conducted and which can be easily applied by healthcare professionals, can be used to evaluate nutrition in children aged 6 months to 6 years, which can contribute to;
•Nurses to early determine nutritional status and to make care plan accordingly.
•Elimination of nutritional problems which may affect future life of children aged between 6 months and 6 years.
Thus, the scale can be used by all healthcare professionals who deal with pediatric care, such as in pediatric clinics, institutions providing primary health care services and in the follow-up of healthy children.
Healthcare professionals who deal with both sick healthy children are recommended to have sufficient knowledge about nutrition and to regularly evaluate the nutritional status of children using a scale of which validity and reliability studies have been conducted to prevent nutrition-related diseases that may come out.
Conflict of Interest
The authors declare no conflict of interest for this study.
Financial Disclosure
No financial support was taken from any institution or entity for this study.
Authors’ Contributions
Conception ID, GM, PU; Design: ID, GM, PU; Data Collection: ID, GM, PU; Conducting research: ID, GM, PU; Statistical Analysis: PU; Literature review: ID, GM, PU; Writing; ID, GM, PU. Critical Review: ID, GM, PU.
References
- Abdurrahman U, Murat D, Zerrin E, et al. Evaluation of the effect of childhood obesity on cardiac functions with echocardiographic and electrocardiographic methods. J Pediatr Endocrinol Metab 2008; 27(3-4): 261-71. [Crossref], [Google Scholar], [Indexed]
- Akgul A. Statistical analysis techniques in medical research-SPSS applications 3rd Edition. Ankara: Emek Ofset 2005; pp: 382-95.
- Archer La, Rosenbaum Pl, Streiner Dl, et al. The children's eating behavior inventory: Reliability and validity results. J Pediatr Psychol 1991; 16: 629-42. [Crossref], [Google Scholar], [Indexed]
- Birch Ll, Fisher Jo, Grimm-Thomas K, et al. Confirmatory factor analysis of the child feeding qustionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 2001; 36: 201-10. [Crossref], [Google Scholar], [Indexed]
- Birch Ll, Fisher Jo. Development of eating behaviors among children and adolescents. Pediatrics 1998; pp: 539-49. [Crossref], [Google Scholar], [Indexed]
- Carruth Br, Skinner Jd. Feeding behaviors and other motor development in healthy children (2-24 months). J Am Coll Nutr 2002; 21: 88- 96. [Crossref], [Google Scholar], [Indexed]
- Crist W, Mcdonnell P, Beck M, et al. Behavior at mealtime and nutritional intake in the young child with cystic fibrosis. J Dev Behav Pediatr 1994; 15: 157-61. [Crossref], [Google Scholar]
- Eksioglu A, Yesil Y, Turfan CE, et al. Adaptation of infant nutrition attitude scale (iowa) to Turkish: A validity and reliability study. J Nurs Educ 2016; 13: 209-215. [Crossref], [Google Scholar], [Indexed]
- Erdim L, Ergun A, Kuguoglu S. Validity and reliability of child nutrition questionnaire in school-aged children. Clin Exp Health Sci. 2017. [Crossref], [Google Scholar], [Indexed]
- Evaluation of the effect of childhood obesity on cardiac functions with echocardiographic and electrocardiographic methods
- Giray H. Nutrition with breast milk. Front Pediatr 2004; 13. [Crossref], [Google Scholar]
- Gozum S, Aksayan S. Guidelines for cross-cultural scale adaptation II: Psychometric properties and cross-cultural comparison. J Res Nurs 2003; 1: 3-14. [Crossref], [Google Scholar], [Indexed]
- Gurel S Inan G. Diagnostic methods, prevalence and etiology of childhood obesity. Med Teach 2001; 2: 39–46. [Crossref], [Google Scholar]
- Hamamci Z, Hamamci E. Child development theories and their reflections for language teachers. J Educ Train 2015; 4: 125-134. [Crossref], [Google Scholar]
- Harrington D. Confirmatory factor analysis. Printed in the United States of America: Oxford University Press. 2009.
- Holub S, Musher E. Examining preschoolers' nutrition knowledge using a meal creation and food group classification task: Age and gender differences. Early Child Dev Care 2010; 180(6): 787-98. [Crossref], [Google Scholar]
- Ilgaz S. Complementary nutrition guidebook for health professionals (2nd edn). 2009.
- Kandemir D. Classification and clinical characteristics of obesity. J Pediatr 2000; 21: 500-506. [Crossref], [Google Scholar]
- https://motherchildnutrition.org/#:~:text=It%20is%20the%20World's%20Largest,of%20balanced%20nutrition%20and%20health.
- Koksal G, Gokmen H. Obesity in preschool period. Ankara: Ministry of Health Publications. 2008
- Koksal G, Gokmen H. Preschool obesity. Ankara: Ministry of Health Publications. 2012
- Lynn M. Determination and quantification of content validity. Nurs Res 1986; 35: 382-385. [Crossref], [Google Scholar]
- Oguz S, Derin DO. Examination of some nutritional habits of 60-72 months-old children. Primary Education. 2013; 12: 498-511. [Crossref], [Google Scholar]
- Onur F. A Study on nutrition knowledge levels and vegetable and fruit consumption habits of families with different socio- economic levels. Ankara: Ministry of Health Publications.
- Oner N, Vatansever U, Garipagaoglu M, et al. Dietary intakes among Turkish adolescent girls. Nutr Res 2005; 25: 377–386. [Crossref], [Google Scholar]
- Ozdemir O, Ozdemir GP, Kadak TM. "Current approaches in psychiatry" 2012; 4: 566-589. [Crossref], [Google Scholar]
- Ozmert EN. Supporting early childhood development-II: Environment. J Child Health Care 2015; 48: 337-54. [Crossref], [Google Scholar]
- https://www.who.int/publications-detail-redirect/9241562218