- Biomedical Research (2011) Volume 22, Issue 4
Transient congenital hypothyroidism- A Rare Case
Manish Kumar Singh, Pushpa Tondon, Ashish Gupta, S. M. Natu*, Wahid Ali, Raj MehrotraDepartment of Pathology, C S M Medical University (Earlier King George’s Medical University), Lucknow, U.P., India
- Corresponding Author:
- S. M. Natu
Chemical Pathology Lab
Department of Pathology
CSM Medical University
(Earlier King George’s Medical University)
Lucknow-226003, U.P., India
Accepted Date: May 15 2011
Abstract
Iodine deficiency is the most common cause of hypothyroidism worldwide but in areas of Iodine sufficiency, other causes including autoimmunity and iatrogenic factors are more common. During pregnancy, autoimmune thyroid disease, characterized by presence of specific thyroid auto antibodies, is mostly responsible for hypothyroidism. Such females, who often had previous history of repeated abortions, have infants with transient mild elevation of serum TSH above normal reference value for age in initial months of life. This type of transient congenital hypothyroidism, caused by maternal-fetal transfer of TSH-R blocking antibodies, is a rare condition. Here we present a case of newborn with known hypothyroid mother, whose TSH level was found to be raised at age of 1 day and goes back to within the normal range at the age of 17 days without taking treatment.
Keywords
Transient congenital hypothyroidism, Pregnancy, TSH-R blocking antibodies.
Introduction
Transient congenital hypothyroidism is an uncommon condition and caused by multiple factors including maternal exposure to goitrogenous substances (iodine, thioureas, sulphonamides etc.), prematurity and maternal-fetal transfer to TSH receptor blocking antibodies [1]. The mean annual incidence rate of autoimmune hypothyroidism is up to 4 per 1000 women and 1 per 1000 men [2]. But epidemiological data about true incidence of transient congenital or neonatal hypothyroidism due to autoimmunity is limited. It is now well established that maternal thyroid function throughout pregnancy influences the neurodevelopmental outcome of the child. There are examples, in which maternal hypothyroidism leads to the impaired psychomotor development of the offspring. So the diagnosis of such case where maternal hypothyroidism could lead to hypothyroidism or any of its consequences in infant should be thoroughly evaluated. Transient Congenital hypothyroidism is one of those condition where maternal defect leads to an abnormal pattern of TSH level in offspring after birth and may compel any practitioner to advice oral thyroid supplement to the infant for long periods without even knowing the exact cause. Moreover the knowledge of such entity would alert the practitioner to control the mother's thyroid function in subsequent pregnancies in order to avid any impairment of fetal neronal development.
In one of the study carried out in a study material of Greece, it was found that transient congenital hypothyroidism due to maternal-fetal transfer of TSH-R blocking antibody accounts for 2.7% of all cases of congenital hypothyroidism [1]. We present a case of newborn with known hypothyroid mother, whose TSH level was found to be raised at age of 1 day and goes back to within the normal range at the age of 17 days without taking treatment.
Case Report
A one day old female baby along with her mother, who is 26 years old, multiparous (P2+5) lady, married for 8 years (no consanguineous marriage) attended the Chemical Pathology Lab, Department of Pathology, C S M Medical University
(Earlier King George’s Medical University), Lucknow, Uttar Pradesh, India for thyroid profile.
Examination of Baby
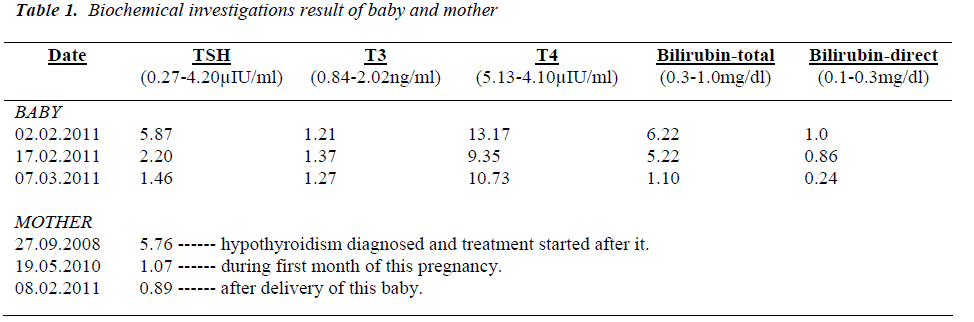
The thyroid profile of baby showed increased TSH, normal T3 and normal T4 levels. Meanwhile, the mother was diagnosed as having hypothyroidism in September, 2008 and was on oral thyroxin supplement (initially 25μg) since then, including the whole pregnancy period (now 50μg). Her thyroid profile after delivery was within range. However at the age of 17 days of this baby, thyroid profile was again done for baby (still the baby not taking treatment) and this time it showed normal TSH, normal T3, normal T4 levels. We again did the thyroid profile at the age of 35 days and it came out within the range.
During pregnancy, pathological examination reports of mother were negative for TORCH infections, HIV 1 & 2, VDRL, lupus anticoagulant and anticardiolipin antibodies. She did not give history of impaired glucose tolerance or gestational diabetes mellitus, hypertension, smoking, alcohol intake, irradiation exposure or intake of goitrogenous substances or noxious drugs during pregnancy.
The baby was delivered at the gestational age of 38 wk 5 days, weighing 2.8kg. Baby had APGAR scoring of 6/6/7. Both mother and baby did not show features suggestive of any complication and baby was breastfed by mother within 30 minutes. However the mother had bad obstetric history including 5 repeated abortions in last 8 years. Her last pregnancy resulted in a female baby weighing 2.5kg in July 2009 (after starting treatment for hypothyroidism) and did not show any motor or developmental delay or other features suggestive of hypothyroidism up to the current age of 1½yrs. Her thyroid profile at this time showed normal TSH, normal T3, normal T4 levels (Table 1).
Discussion
Thyroid gland embryogenesis is completed by 10 wks of gestation, at which time colloid formation is demonstrable. Pituitary and plasma TSH concentration increase during 2nd trimester in human fetus, coincident with development of pituitaryportal circulation. The fetal thyroid secretes predominantly thyroxin (T4) and plasma total concentration increase from low levels at 16 wks gestation to plateau values at 36-38 wks gestation [3]. Although fetal thyroid development occurs largely independent of maternal influences, limited maternal to fetal transport of thyroid hormones occurs (supplying 20-30% of turnover) and it may serve as local T3 production by hypothyroid fetus and may also related to relative lack of signs and symptoms in such congenital hypothyroid infants. In this case, as is evident that despite of mother taking thyroxin supplement daily (and being euthyroid) the baby developed hypothyroidism immediately after birth. But soon, TSH level come to normal and remains so. This transient form of congenital or neonatal hypothyroidism occurs either due to maternal exposure to goitrogenous substances, prematurity (both of which are not present in this case) or due to autoimmune causes. However, strictly speaking, here we are not dealing with a patient of clinical hypothyroidism. This case is a result of maternal autoimmune thyroid disease, due to presence of TSH receptor blocking antibodies (which are going to disappear subsequently) leading to transient elevation of TSH levels
whereas serum T3 and T4 levels are normal. Now with absence of any inter relating cause which leads to solitary TSH elevation (like severe nonthyroid illness, TSH secreting pituitary tumor, (thyroid hormone resistance) and hypothyroidism being the most common cause of elevated TSH level- we are designating it as Hypothyroidism.
Autoimmune thyroid disease is complex interaction between genetic and environmental factors, many of which remains to be defined. Thyroid cells express MHC class II molecules in autoimmune thyroid disease but not under normal conditions and its expression leads to thyroid auto antigen presentation. But this occurs only after stimulation with IF-γ by T-cell infiltrate, so this class II expres-sion is 2o events.The common thyroid auto antigens in-clude thyroglobulin (TG), thyroid peroxidase (TPO), and TSH Receptor and Na+/I- symporter (NIS) antigen. TG and TPO antibodies occur commonly in patients of Hashimoto’s thyroiditis and myxedema [4]. But transplacental passage of either of these antibodies don’t cause any effect on fetus thyroid as cell mediated injury is re-quired to initiate autoimmune injury to thyroid [4,2]. Thyroid stimulating antibodies directed against TSH-Receptor (TSAbs) are hallmark of Graves’ disease.Up to 20% of patients with autoimmune hypothyroidism also have antibodies directed against TSH-R but in contrast to TSAbs, they prevent binding of TSH. Therefore these TSH-R blocking antibodies can cause hypothyroidism by transplacental passage and are especially common in Asian population and may induce transient neonatal hypo-thyroidism [1,4,2]. However the incidence of these TSH-R blocking antibodies during pregnancy is not well known [5]. These TSH- R blocking antibodies are present in newborn’s serum and used to disappear from infant’s circulation by 3rd month of life [1]. All such infants with transient congenital hypothyroidism due to maternal thy-roid autoimmunity are full term and are born after an un-eventful pregnancy. The most common clinical findings are prolonged jaundice (>10 days; in our case it is pre-sent) and large posterior fontanelle (> 0.5 cm). No mal-formations are present in these patients [1,5].
Rarely patients have a mixture of TSAbs and TSH-R blocking antibodies and thyroid function oscillate be-tween hyper- and hypo thyroidism as one of the other an-tibody become dominant. Predicting the course is difficult and requires close monitoring of thyroid function [4,2]. In our case, there is initially hypothyroidism, followed by euthyroid hormone levels. As already mentioned that ma-ternal thyroid function throughout pregnancy influences the neurodevelopmental outcome of the child and there are studies in which both mother and child are hypothy-roid, as in areas with severe iodine deficiency or in auto-immune thyroid disease, the psychomotor developmental of the offspring is also impaired.
Therefore in these families genetic counseling is very im-portant to alert the parents to the possibility of recurrence of the disease in subsequent offspring, information which will ensure early evaluation and treatment of the newborn.
Furthermore such findings are of utmost importance for alerting physicians to control the mother's thyroid func-tion in subsequent pregnancies in order to avid any im-pairment of fetal neuronal development. There is well defined inheritance pattern found for this entity and all such infants are born after uneventful pregnancy and only abnormal findings are persistent jaundice and large poste-rior fontenelle. No long term follow up literature is avail-able for such cases now [1]. On the basis of these facts and findings, we present a rare case of transient congeni-tal or neonatal hypothyroidism caused by autoimmune disease of mother due to TSH-R blocking antibodies. The diagnosis of such case is very important for genetic coun-selling, early treatment initiation and adequate control of mother’s thyroid function during subsequent pregnancies so that any neurodevelopmental abnormality of fetus could be avoided.
References
- Mengrelli C. Transient Congenital Hypothyroidism due to maternal autoimmune diseases; HORMONES. En-docrinol Metabol 2003; 2: 113-119.
- Diseases of Thyroid gland, Harrison?s Principles of Internal Medicine, Vol.II, 17th ed., McGraw Hill, 2230.
- Polk DH, Fisher DA. Fetal and Neonatal thyroid Physi-ology; Burrow GN, Fisher DA, Lasen PR: Maternal and Fetal thyroid Function. N Eng J Med 1994; 331:1072-1078.
- Cho BY, Kim WB, Chung JH. High prevalence and little changes in TSH receptor blocking antibodies titer with thyroxin and anti thyroid drug therapy in patients with nongoitrous autoimmune thyroiditis. Clin Endo-crinol 1995; 43: 465-471.
- Rovelli R. Newborns of mother affected by autoimm-une thyroiditis: the importance of thyroid function monitoring in first few months of life. Italian J Pediat 2010; 36:24-26.