Research Article - Biomedical Research (2016) Volume 27, Issue 4
Total laparoscopic pancreatoduodenectomy for duodenal papilla carcinoma
Hongcun Sha1#, Xiangcheng Qin2#, Zhenzhen Dai3*, Xiaoming Hong1* and Kunjie Xu1
1Department of General Surgery, NingBo YinZhou No.2 Hospital, Branch Hospital of The First Affiliated Hospital of Medical School of Zhejiang University, 1 Qianhe Road, Ningbo 315100, China
2Department of Urology Surgery, NingBo Yinzhou No.2 Hospital, Branch Hospital of The First Affiliated Hospital of Medical School of Zhejiang University, 1 Qianhe Road, Ningbo 315100, China
3Department of Pathology, YinZhou People’s Hospital, Affiliated to Medical school of Ningbo University, 251 East Baizhang Road, Ningbo 315040, China
#These authors contributed equally to this work.
- *Corresponding Author:
- Zhenzhen Dai
Department of Pathology
YinZhou People’s Hospital
Affiliated to Medical school of Ningbo University
China
E-mail: su30d@sina.com
Xiaoming Hong
Department of General Surgery
NingBo YinZhou No.2 Hospital
Branch Hospital of The First Affiliated Hospital of Medical School of Zhejiang University
China
E-mail: hongxiaoming2002@aliyun.com
Accepted date: April 17, 2016
Abstract
Background: Advances in surgical technique and increase in surgeon’s experience have made total laparoscopic pancreatoduodenectomy (TLPD) a substantially safer procedure. This study aimed to report our successful experiences of TLPD for the treatment of duodenal papilla carcinoma.
Methods: Retrospective review of 4 patients who underwent TLPD between November 2013 and December 2014 was performed. The outcomes of these patients were analyzed.
Results: TLPD was accomplished successfully. The mean operative time was 367 minutes. The mean blood loss was 248 ml. The median lymph node count was 16.5. The median length of hospital stay was 16 days. Postoperative morbidity included 1 case of mild pancreatic leak and 1 case of pneumonia. The overall incidence of postoperative complications was 50%. There were no perioperative deaths.
Conclusion: TLPD is a feasible, safe and effective method for treatment of duodenal papilla carcinoma.
Keywords
Duodenal papilla carcinoma, Pancreatogastrostomy, Laparoscopy, Total laparoscopic pancreatoduodenectomy.
Introduction
Since Gagner and Pomp first described the total laparoscopic pancreatoduodenectomy (TLPD) [1], the safety and feasibility of TLPD has been under debate. TLPD was associated with more complicated operation longer time of operative procedure and hospital stay, more complications and higher incidence of open conversions. With the advance of laparoscopic techniques and experiences, especially in development of laparoscopic gastrectomy and laparoscopic distal pancreatectomy, it is safe, reliable and practical to carry out TLPD based on laparoscopic gastrectomy and laparoscopic distal pancreatectomy [2-6]. Here we report our experience of successful performing TLPD in 4 cases of duodenal papilla carcinoma.
Materials and Methods
Patients
This study was approved by the Ethics Committee of The Yinzhou Second People’s Hospital and the patients provided signed consent. Between November 2013 and December 2014, 4 patients received TLPD for duodenal papilla carcinoma at the Yinzhou Second People’s Hospital. They had no known family history, 3 were male and 1 was female, ranging in age from 59 to 75 years (mean 69 years). Obstructive jaundice was found in 3 cases and fever in 1 case.
The patients were thoroughly evaluated preoperatively by ultrasonography, computed tomography, gastroduodenoscopy, endoscopic ultrasonography, and biopsy was required to confirm duodenal papilla carcinoma. In addition, 3 patients with obstructive jaundice were assessed by MRCP and ERCP. The characteristics of patients are presented in Table 1.
| Patient | Age (days) |
Gender | The site of the tumor | Operative time (min) |
EBL (mL) | Tumor types | The time of anal exhaust | LNM | Complication | Stay (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 73 | Male | Duodenal papilla | 413 | 560 | Duodenal papilla | 4 | 0/13 | No | 12 carcinoma |
| 2 | 67 | Male | Duodenal papilla | 372 | 90 | Duodenal papilla | 3 | 19-Jan | Pneumonia | 25 |
| 3 | 75 | Male | Duodenal papilla | 357 | 70 | Duodenal papilla | 4 | 0/16 | Pancreatic leakage | 13 |
| 4 | 59 | Female | Duodenal papilla | 325 | 270 | Duodenal papilla | 2 | 18-Jan | No | 14 |
Table 1. Characteristics of 4 patients undergoing TLPD.
Surgical technique
TLPD was undertaken under general anesthesia with the patients in supine position. The first incision at the umbilicus was 10 mm for the lens, then we established pneumoperitoneum using a standard umbilical cut down technique and the pressure of carbon dioxide was about 12-15 mmHg. Four other incisions of 12, 5, 12 and 5 mm were made at the left upper quadrant, the left side of abdomen, the right side of abdomen and the right upper quadrant, respectively.
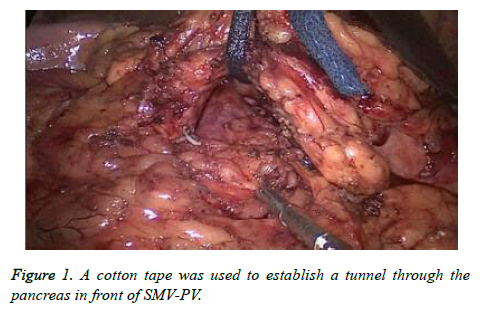
Abdominal exploration did not reveal metastasis of the nearby organs or ascites. We incised greater omentum along the edge of transverse colon, then opened omental sac. The post-bulbar duodenum was divided until the gastroduodenal artery was completely freed, then we ligated its origin. The dissection was performed below the pancreatic head so that Henle’s surgical trunk could be easily located. This artery was then followed cranially to the superior mesenteric vein (SMV). To explore the relationship of the lesion and SMV, portal vein (PV), the division was performed between the pancreas and SMV. We used a cotton tape to establish a tunnel through the pancreas in front of SMV-PV (Figure 1).
The pancreatic head and duodenum were detected, dissected and freed in a clockwise direction along the c-ring of duodenal wall. If the tumor had not invaded the surrounding blood vessels, the procedure was continued with the removal of the posterior peritoneum and the ligament of Treitz along the descending part and horizontal part of duodenum. After the transection of proximal jejunum, the proximal jejunum was pulled further to subphrenic space by natural clearance behind mesenteric vascular root. At this stage, we accomplished the dissection of the pancreatic head and duodenum.
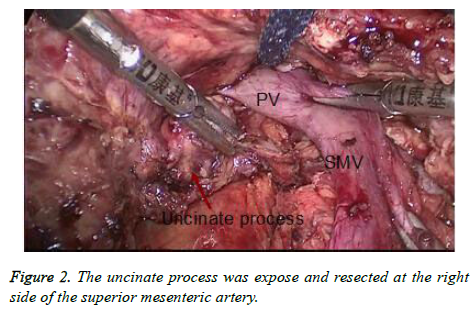
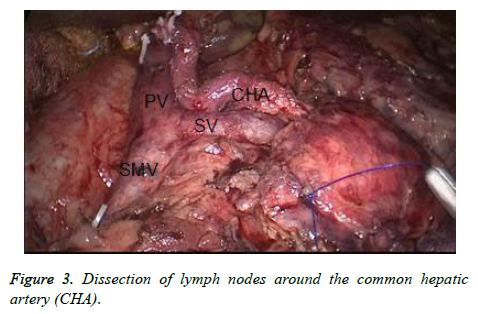
Next we performed complete separation between SMV-PV and the pancreas, and the uncinate process was exposed and resected at the right side of the superior mesenteric artery (Figure 2). Lymph nodes in the hepatoduodenal ligament were dissected, then the gallbladder was removed and common hepatic duct was transected at the level of the cystic duct. The neck of the pancreas was transected in front of the PV. In addition, dissection of lymph nodes around the common hepatic artery was performed (Figure 3). Distal gastric area accounting for 50% of full stomach was transected using an Endo-GIA Stapler with a green or golden staple cartridge. The resected specimen was removed through an approximately 4 cm of longitudinal incision in umbilical region.
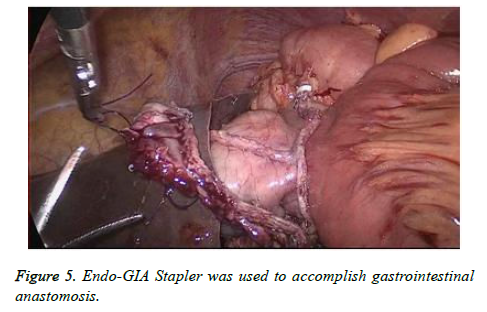
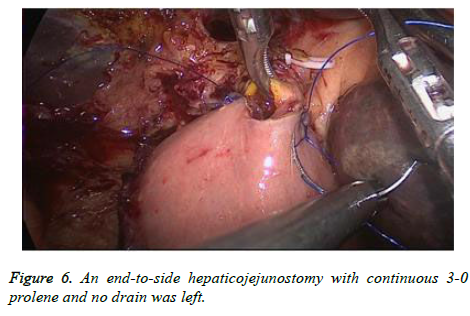
The last surgical step was reconstruction of digestive tract. First, binding pancreatogastrostomy (PG) was performed (Figure 4). After drainage tube was put in the pancreatic duct, small incision was made in the posterior wall of the stomach and a preset double purse-string suture was used to put the pancreatic duct into gastral cavity. Next, Endo-GIA Stapler was used to accomplish gastrointestinal anastomosis (Figure 5). Finally, an end-to-side hepaticojejunostomy with continuous 3-0 prolene and no drain was left (Figure 6).
Results
TLPD procedure was successful in all 4 patients. None of the cases required conversion to an open operation. The duration of the procedure was 325-413 min (mean 367 min).The volume of blood loss was 70-560 ml (mean 248 ml). The time of gut function recovery was 2-4 days (mean 3.3 days). The hospital stay for the 4 patients was 12-25 days (mean 16 days). One patient had grade A postoperative pancreatic leakage (POPF) according to the international clinical grading system and was treated conservatively. Pulmonary infection occurred in one patient and was cured by use of antibiotics. The overall incidence of postoperative complications was 50%. The postoperative histopathology confirmed duodenal papilla carcinoma in 4 patients. The surgical margin was negative. The median number of lymph nodes harvested was 16.5 (rang 13 to 19) per patient. The follow-up was 12 months, at the time of the last follow-up, 4 patients were still alive.
Discussion
Pancreatoduodenectomy is one of the most difficult abdominal operations and should be performed only by very experienced surgeons. However, there is controversy about the safety and feasibility of this technique [7]. In recent years, as surgeons’s experiences with advanced laparoscopy have increased, there is evidence demonstrating the safety and feasibility of TLPD [8,9]. Several clinical series have indicated that TLPD can be performed as safely as the traditional open approach [10,11]. The whole operation fits the principles of no-touch radical excision of pancreatic and duodenal carcinoma, including emphasis on the whole block excision of tumor to ensure enough surgical margins and complete the lymph node dissection. Laparoscopic technique can enlarge local field of vision and it is beneficial to the exposure of the surgical field [12]. Therefore, the separation of PV, SMV, and identification of the surgical plane can be more easily accomplished to produce perivascular lymph node dissection. Laparoscopic resection of uncinate process of the pancreas is one of the difficulties in TLPD. As long as it is done in a controlled way with excellent exposure, laparoscopic resection of the uncinate process of the pancreas is feasible and safe. We alternately used ultrasonic knife together with Ligasure to widen the potential space between SMV-PV and the head of pancreas. Consequently, this group of 4 patients got thorough removal of the uncinate process of the pancreas smoothly, and blood loss was negligible. Another operation difficulty is the reconstruction of the pancreas, which is still one obstacle of pancreatic surgery. Compared with binding pancreaticojejunostomy, our cases of pancreatic duct size (<3 mm) with PG are relatively simple and the operative time is only 20 min. Binding PG has several advantages, such as being less invasive, and the preservation of pancreas function. The reconstruction is more beneficial because gastroscope after surgery can stop the bleeding of the pancreatic remnant. In our case, because the pancreatic duct diameter was not thick, binding PG was used to accomplish digestive tract reconstruction. The main complication only included 1 case of postoperative pancreatic leakage, with gastroparesis at the same time, and then cured with conservative management. Reexamination by gastroscope at 2-3 months after surgery showed that pancreatic tissue in gastric cavity recovered by gastric mucosa. The indications of TLPD often include the size and location of the tumor, usually require tumor diameter ≤ 3.5 cm. We consider that TLPD is not a practical approach for large tumors that are likely to cause infiltration, vascular pressure and uncontrollable bleeding when separated. When the tumor is located in the distal bile duct or the ampulla of Vater, we will find it early. Appropriate patient selection is important. We chose 4 cases of tumors within duodenum, as demonstrated on preoperative imaging, which was much better for us to practice TLPD. Operative time of TLPD was 325-413 min, shorter than reported in relevant literature [13].
Our experiences are as follows: (1) The surgical team was relatively fixed, including the surgeon, the first assistant, and the camera holder. (2) Before attempting the first TLPD, extensive experience was ensured. Our surgical team has almost 10 years of experience for laparoscopic gastrectomy. Sufficient experience with laparoscopic distal pancreatectomy in over 40 patients has been obtained. Moreover, we are familiar with the anatomy of the peripancreatic vessel system. (3) Inclusion criteria included relatively simple tumors confined to the duodenal papilla or the head of the pancreas and favorable vascular anatomy. Exclusion criteria included patients with malignant involvement of the inferior vena cava and portal vein. (4) All selected patients underwent accurate preoperative evaluation. Laparoscopic exploration and resection at the same time would reduce operating time in the course of concrete operation. (5) We used a cotton tape to pass around the neck of the pancreas, then the uncinate process of the pancreas was removed, and portal vein was completely dissected free before the resection of the neck of the pancreas. These procedures could ensure suitable tension and are less time consuming. (6) Binding PG is still a good choice for reconstruction with some advantages [14]. Additionally, it reduces operating time and bleeding. This group of 4 patients underwent regional lymph node dissection. The mean number of lymph nodes was 16.5, similar to reported in the literature [15]. Our experience of laparoscopic lymphadenectomy is that the operation should follow the principle of giving priority to the surgical plane. This not only can reduce intraoperative bleeding, speed up process, but also conform to the principle of tumor-free technique. When cleaning lymph nodes around the blood vessels, it is easy to make the blood vessels skeletonize because the level along vascular sheath is devoid of blood vessels. In conclusion, these case series highlight the feasibility and safety of TLPD for treating duodenal papilla carcinoma. However, the number of cases in our group is limited and the follow-up time is short. Long-term follow-up in larger numbers of cases are needed to support our experiences.
Acknowledgements
We thank financial support of NingBo YinZhou No.2 Hospital in Zhejiang, China.
References
- Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994; 8: 408-410.
- Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy: feasibility and outcomes in an early experience. Arch Surg. 2010; 145: 19-23.
- Costi R, Randone B, Mal F. Laparoscopic minor pancreatic resections (enucleations/atypical resections). A long-term appraisal of a supposed mini invasive approach. Videosurgery Miniinv. 2013; 8: 117-129.
- Jacobs MJ, Kamyab A. Total laparoscopic pancreaticoduodenectomy. JSLS 2013; 17:188-93.
- Machado MA, Surjan RC, Goldman SM, Ardengh JC, Makdissi FF. Laparoscopic pancreatic resection From enucleation to pancreatoduodenctomy 11-year experience. Arg Gastroenterol 2013; 50: 214-218.
- Keck T, Küsters S, Wellner UF, Hopt UT, Karcz KW. Total laparoscopic partial pancreatoduodenectomy and reconstruction via laparoscopic pancreatogastrostomy. Langenbecks Arch Surg. 2013; 397: 1009-1012.
- Gumbs AA, Rivera AMR, Milone L. Laparoscopic pancreatoduodenectomy: A review of 285 published cases. Ann Surg Oncol. 2011; 18: 1335-1341.
- Senthilnathan P, Srivatsan Gurumurthy S, Gul SI. Long-term results of laparoscopic pancreaticoduodenectomy for pancreatic and periampullary cancer-experience of 130 cases from a tertiary-care center in South India. J Laparoendosc Adv Surg Tech A 2015; 25: 295-300.
- Liang S, Hameed U, Jayaraman S. Laparoscopic Pancreatectomy: indications and outcomes. World J Gastroenterol 2014; 20: 14246-14254.
- Chalikonda S, Aguilar-Saavedra JR, Walsh RM. Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc 2012; 26: 2379-2402.
- Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the accordion severity grading system. J Am Coll Surg 2012; 215: 810-819.
- Fisher SB, Kooby DA. Laparoscopic pancreatectomy for malignancy. J Surg Oncol 2013; 107: 39-50.
- Boggi U, Amorese G, Vistoli F, Caniglia F, De Lio N, Perrone V, Barbarello L, Belluomini M, Signori S, Mosca F. Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc. 2015; 29: 9-23.
- Ohigashi H, Ishikawa O, Eguchi H, Sasaki Y, Yamada T, Kishi K, Noura S, Takachi K, Miyashiro I, Oue M. A simple and safe anastomosis in pancreaticogastrostomy using mattress sutures. Am J Surg. 2008; 196: 130-134.
- Kim SC, Song KB, Jung YS. Short-term clinical out- comes for 100 consecutive cases of laparoscopic pylorus- preserving pancreatoduodenectomy: pancreatoduodenectomy: improvement with surgical experience. Surg Endosc 2013; 27: 95-103.