Research Article - Case Reports in Surgery and Invasive Procedures (2017) Case Reports in Surgery and Invasive Procedures (Special Issue 1-2017)
The incidence of retinal redetachment after Pars plana vitrectomy with 360° endolaser.
- *Corresponding Author:
- Peter Stalmans
Department of Ophthalmology, UZ Leuven Herestraat 49, B3000 Leuven Belgium
Tel: 003216332660
E-mail: peter.stalmans@uzleuven.be
Accepted date: March 16, 2017
Citation: Peene G, Fils JF, Vanwynsberghe D, et al. The incidence of retinal redetachment after Pars plana vitrectomy with 360° endolaser. Case Rep Surg Invasive Proced. 2017;1(1):8-12.
Abstract
Purpose: To evaluate the incidence of retinal redetachment after pars plana vitrectomy (PPV) with 360° laser for the treatment of primary Rhegmatogenous retinal detachment (PRDD). Methods: A retrospective review of 1,063 eyes after primary PPV and 360° laser retinopexy for PRRD between 2004 and 2014. Different parameters were analyzed for their influence on the redetachment rate. A multivariate regression analysis was performed. Results: The mean age was 61.49 ± 11 years. The Phakic status did not influence the success rate. The most common cause of redetachment was leakage through the original retinal tear (35.53%). Mostly, retinal breaks occurred in the superior quadrant (55.22%). The location of the break had no significant influence on the reoperation rate. Multivariate analysis identified the use of an encircling band as the only factor significantly associated with a lower reoperation rate. Conclusion: Primary vitrectomy combined with 360° laser therapy is an effective treatment in patients with PRRD. The primary anatomic success rate was 91.16%. The only factor that influenced the outcome was the positive effect of an encircling band.
Keywords
360° Endolaser treatment, Pars plana vitrectomy, Primary Rhegmatogenous retinal detachment.
Introduction
The precursors of primary Rhegmatogenous retinal detachment (PRRD) are changes in the vitreous body leading to tractional forces on the retina inducing a break through which fluid gains access to the sub retinal space [1]. To achieve successful retinal reattachment, the goal of surgery for RRD is to close all retinal breaks and relieve vitreous traction, which may also reduce the incidence of new breaks [2]. Significant improvements in vitrectomy technique in recent years are changing the surgical approach to multiple vitreoretinal pathologies. Since first introduced by Machemer in 1971, pars plana vitrectomy (PPV) has been shown to be an effective treatment for RRDs [1,3,4]. Although, there still is controversy regarding the best surgical technique to employ when repairing PRRD, PPV and combined PPV with an encircling band (PPV/EB) remain the most popular techniques used in the primary repair of RRD (The SPR study group, 2003).
The primary objective of this retrospective study was to evaluate the recurrence of RD after PPV with intraoperative 360° endolaser for the treatment of a PRRD. The study reviewed the characteristics and outcomes of patients, who underwent primary repair of RRD with this surgical technique.
Methods
All patients diagnosed at the center with PRRD between January 2004 and August 2014 were included in the study. Inclusion criteria were: PRRD in Pseudophakic or phakic eyes with retinal break(s). Only primary retinal detachment repairs were included. Exclusion criteria were: evidence of proliferative vitreoretinopathy (PVR) ≥ grade C; giant retinal tears; multiple breaks over 360°; exudative retinal detachment; previous vitreoretinal surgery or glaucoma surgery; and high myopia ≥ -8D. Retinal detachments treated by buckling surgery only were excluded from this trial. Retinal detachments treated with oil or C3F8 gas tamponade were also excluded. All surgeries were performed at the University Hospital of Leuven (UZ Leuven), Department of Ophthalmology, Leuven, Belgium, by different vitreoretinal surgeons. No surgeries were performed by fellows or residents in training.
Surgical technique
A standard, three-port 23 Gauge pars plana vitrectomy (PPV) technique using the Associate® or EVA™ systems (DORC, Zuidland, The Netherlands) and the EIBOS noncontact wideangle viewing system (Haag-Streit, Wedel, Germany) was used in all cases. Phakic eyes were vitrectomized without cataract surgery if the patient was younger than 50 years old and had a clear lens. In phakic patients older than 50 years old, a combined phaco-vitrectomy procedure was performed. In all cases, core vitrectomy was performed in vacuum mode, followed by a partial perfluorocarbon liquid (PFCL) injection. Subsequently, further removal of the peripheral vitreous up to the vitreous base was performed in flow-mode. Adjacent to the ora serrata, a row of 4-5 endolaser spots in width was applied over 360° and completely surrounding all retinal breaks after a complete fill of the vitreous cavity with PFCL. During PFCL/air exchange, endodrainage was done at the site of the break to capture any subretinal fluid that was potentially pushed peripherally from the retinal break. Depending on the pre-operative assessment, the use of an encircling band was preferred when the location of the retinal break(s) was/were in the inferior quadrant(s), or when a PVR grade C or worse was present. We only included eyes with air/SF6 gas tamponade. The concentration used was 25%.
Statistical analysis
Student T-test was used for continuous data after a test of the normality of the residuals of the model with the Shapiro- Wilks test and the homoskedasticity of the variances with the Bartlett’s Chi-Squared test. Fisher and its associated odds ratio, or Chi-Squared Tests were used to compare groups for count data. Tuckey’s multiple comparisons for binary data were performed with the multcomp R package [5]. A p-value <0.05 was considered as statistically significant. The R Software 3.2.1 [6] was used to produce statistical results. Stepwise multivariate regression analysis was used to identify the independent factors related to a low reoperation rate.
Results
Patient demographics and initial retinal detachment characteristics
A total of 1,063 eyes from 1,034 patients were included in this study. Patients were divided into two study groups: a ‘reoperation group’ (94 eyes) and a ‘no reoperation group’ (969 eyes) (Table 1). Investigation into whether the two groups differed in terms of age was carried out. The Bartlett’s chi-squared test (χ2=0.668, df=1, p-value=0.414) indicates that the variances of the two groups do not differ. The Kolmogorov-Smirnov test indicates that the residuals (D=0.043, p-value=0.036) are not normally distributed. We therefore performed a non-parametric test: the Wilcoxon signed-rank test. Results indicate (W=47734, p-value=0.441) that patients are not older in the reoperation group (median=60.50, Q25=53, Q75=69) compared to the no reoperation group (median=61.00, Q25=55, Q75=68). The mean age, sex and phakic or pseudophakic state at time of operation are listed in Table 1. Standard of care included one follow-up visit in our hospital and we assumed that patients were referred back by their own ophthalmologist in case of surgery failure with redetachment. All patients in this trial were followed for at least 8 weeks. 44 eyes were lost for follow-up. The mean followup time of all patients was 363 days with a mean ± standard deviation of 582 days. The localization of the retinal breaks was as follows: superior quadrant (10-2 O’clock), inferior quadrant (4-8 O’clock), nasal quadrant (2-4O’Clock, right eye and 8-10 O’clock, left eye) and temporal quadrant (2-4 O’clock, left eye and 8-10 O’clock, right eye). When taking both groups together, most of the retinal breaks occurred in the superior quadrant (55.22%). There was no significant difference in age, sex, affected eye (right eye or left eye), location of the retinal break and (pseudo)phakic status of the eye. None of the quadrants had a significantly higher number of reoperation. (I=9.14%, N=7.27%, S=9.88%, T=8.68%; p-value=0.769, Pearson’s Chi2 test) (Table 2).
| Variable | No reoperation (NEyes=969) | Reoperation (NEyes=94) | p-value | All included eyes (NEyes=1063) |
|---|---|---|---|---|
| # patients | 943 | 93 | - | 1034 |
| Mean age | 61 (55-68) | 60.5 (53-69) | 0.441 | 61.49 (±10.93) |
| Male, no. (%) | 628 (64.81%) | 70 (74.47%) | 0.068 | 365 (34.34%) |
| Right eye, no. (%) | 492 (50.77%) | 51 (54.26%) | 0.928 | 543 (51.08%) |
| Retinal break T, no. (%) | 338 (34.88%) | 34 (36.17%) | 0.821 | 372 (35.00%) |
| Retinal break N, no. (%) | 153 (15.79%) | 12 (12.77%) | 0.551 | 165 (15.52%) |
| Retinal break S, no. (%) | 529 (54.59%) | 58 (61.70%) | 0.194 | 587 (55.22%) |
| Retinal break I, no. (%) | 200 (20.64%) | 19 (20.21%) | 1.000 | 219 (20.60%) |
| Phakic eye, no. (%) | 609 (62.85%) | 57 (60.64%) | 0.738 | 666 (62.65%) |
| Macula ?on RD, no. (%) | 398 (41.07%) | 32 (34.04%) | 0.487 | 430 (40.45%) |
T, temporal; N, nasal; S, superior; I, inferior; RD, retinal detachment
Table 1: Baseline characteristics of the ‘no reoperation group’ and the ‘reoperation group’.
| Group | Affected Quadrant | |||
|---|---|---|---|---|
| Inferior (n=372) | Nasal (n=165) | Superior (n=587) | Temporal (n=219) | |
| No reoperation | 338 (90.86%) | 153 (92.73%) | 529 (90.12%) | 200 (91.32%) |
| Reoperation | 34 (9.14%) | 12 (7.27%) | 58 (9.88%) | 19 (8.68%) |
Table 2: Relation between the affected quadrant with a retinal break and reoperation.
Intraoperative data
The intraoperative data are summarized in Table 3. All patients received air and SF6 gas tamponade. All eyes underwent small gauge surgery (23 Gauge). In the no-reoperation group, 132 eyes (13.62%) underwent a combined PPV with an encircling band. In the reoperation group, 5 eyes (5.32%) underwent a combined PPV with an encircling band, 14 eyes underwent placing of an encircling band during the second PPV. The Fisher’s Exact Test indicates that the two variables are not independent from each other (p-value=0.022). The odds ratio with its 95% Confidence Interval equals 2.81 (1.13; 9.02, Wilcoxon test). Eyes that underwent an encircling band procedure were less likely to be reoperated than those without an encircling band (3.65% vs. 9.61%). At the end of each vitrectomy procedure, endolaser photocoagulation was applied over 360° to completely surround all retinal breaks. The mean number of laser coagulates placed was 1056 (range, 522- 2338 coagulates) with a mean ± standard deviation of 262.17. Patients in the no reoperation group did not have a higher number of laser coagulates (median=1.018, Q25=876, Q75=1.200, Wilcoxon test) compared to patients of the reoperation group (median=1.018, Q25=8635, Q75=1232, Wilcoxon test).
| Variable | No reoperation (NEyes=969) | Reoperation (NEyes=94) | p-value | All included eyes (NEyes=1063) |
|---|---|---|---|---|
| Encircling band, no. (%) | 132 (13.62%) | 5 (5.32%) | 0.022 | 137 (12.89%) |
Table 3: Intraoperative characteristics in the ?no reoperation group? and the ?reoperation group?.
Multivariate regression analysis
Multivariate analysis using stepwise method was performed using variables potentially related to the reoperation rate: the preoperative age, gender, eye, location of retinal break T/N/S/I, phakic status of the eye, the use of a scleral buckle, macula status and the number of laser coagulates placed. The result of multivariate logistic regression analysis showed that the only remaining variable related to the reoperation model is the use of an encircling band (p-value=0.006).
Anatomical outcome
Primary success was achieved in 969 eyes (91.16%). Full attachment of the retina was obtained in 100% of the patients’ at the most recent follow-up (mean follow-up time, 363 days). Single surgical re-attachment was defined as anatomically-attached retina without the need for additional surgery. Residual or recurrent peripheral subretinal fluid that was contained by surrounding laser scars was not considered a success, hence only completely reattached retina was considered as a success for this study.
Subsequent surgeries
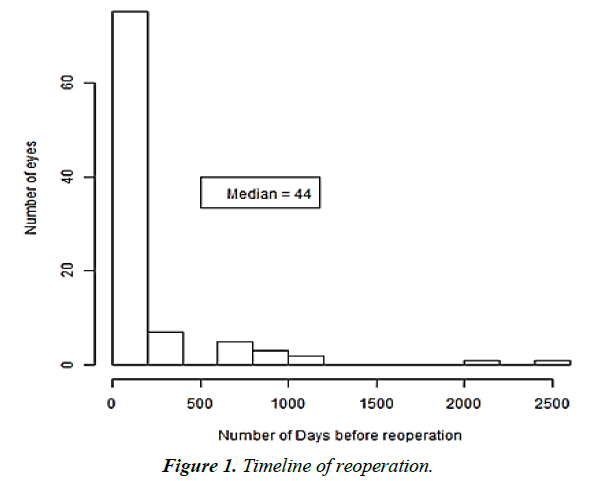
The mean number of days before retinal redetachment and reoperation was 199.6 days (range, five-2445 days; median, 44 days) with a mean ± standard deviation of 393 days (Figure 1). Amongst the eyes that had a redetachment, the majority of eyes required only one subsequent surgery to obtain anatomical success (70 eyes). 15 eyes required a third, 7 eyes a fourth and two eyes a fifth vitrectomy to achieve 100% reattachment. Permanent oil filling was necessary in six of the 10 eyes that required four vitrectomies and in one of the two eyes that required five vitrectomies. The most common cause of a first redetachment was leakage through the original retinal tear (35.53%) followed by PVR, an atrophic hole after laser coagulation, a new retinal tear, laser spots not enough visible on the retina and persistent sub retinal fluid. The most common causes of a second redetachment were PVR, an atrophic hole after laser coagulation, persistent sub retinal fluid and leakage through the original retinal tear (Table 4).
| Reason for First Redetachment | N (%) |
|---|---|
| Atrophic hole after laser coagulation | 14 (18.42%) |
| Leakage through original retinal tear | 27 (35.53%) |
| New retinal tear | 8 (10.53%) |
| Persistent sub retinal fluid | 3 (3.95%) |
| PVR | 19 (25.00%) |
| Not enough endolaser coagulates | 1 (1.32%) |
| Laser spots not enough visible on the retina | 4 (5.26%) |
| Reason for Second Redetachment | N (%) |
| Atrophic hole after laser coagulation | 1 (20.00%) |
| Leakage through original retinal tear | 1 (20.00%) |
| PVR | 1 (20.00%) |
| Persistent sub retinal fluid | 2 (40.00%) |
| PVR, Proliferative Vitreoretinopathy | |
Table 4: Reasons for first- and second redetachments.
Discussion
In this study, in phakic patients older than 50, a combined phacovitrectomy procedure was performed. Many surgeons prefer combined phacoemulsification cataract surgery, vitreous surgery and IOL Implantation in the bag because it is a safe procedure that does not significantly increase the operating time, allows excellent fundal visualisation and spares the patient from having to return for further cataract surgery. The presence of cataract often necessitates a second operation soon after vitreoretinal surgery if lens extraction is not performed simultaneously with the vitreoretinal surgery. In addition, vitrectomy itself causes cataract to progress. Li et al. [7] showed that combined surgery using phacoemulsification with posterior chamber IOL implantation and vitrectomy enables better visualization for the surgeon, reduces the need for a second operation, decreases costs, and allows for early postoperative visual rehabilitation. Based on extensive experience with the combined procedure, they suggest that combined surgery is recommended in selected patients with simultaneous vitreoretinal changes and cataracts [7,8]. Many factors, including surgeon experience and patient
The mean number of days before retinal redetachment and reoperation was 199.6 days (Median, 44 days; Range, five-2,445 days) with a mean ± standard deviation of 393 days. preoperative characteristics, influence the surgical technique in RRD repair. There are no definitive guidelines towards making the decision as to whether or not 360° laser retinopexy is done during a vitrectomy for the treatment of PRRD in a way that will result in a lower incidence of redetachment. 360°retinopexy laser treatment may close occult breaks or may act as a restraint against the posterior migration of an anterior retinal detachment and reduce the incidence of retinal re-detachment [9-12]. A curved endolaser probe allows treatment near the ora serrata in both phakic and pseudophakic patients. Falkner-Radler et al. [13] showed that primary vitrectomy combined with 360° endolaser therapy seems to be as effective as vitrectomy combined with an encircling scleral buckle in patients with Rhegmatogenous retinal detachment, with possible benefits of an improved patient-comfort and a more stable refractive status after surgery [13], 360° laser retinopexy was also found to have a protective effect on the redetachment rates post silicone oil removal (SOR) [14]. Koh et al. [15] showed that intraoperative 360 degree retinopexy was associated with a three-fold reduction in the incidence of RRD after PPV [15]. Also, Chaturvedi et al. [2] showed in a recent study that PPV with scleral depressed vitreous shaving, 360 degree peripheral endolaser and 14% C3F8 leads to successful anatomical reattachment with visual improvement in patients with primary RRD breaks [2].
In this study, peripheral vitreous removal and 360° endolaser photocoagulation yielded an overall 91.16% (969/1063) single surgical success rate. In literature, PPV for primary RRD has a single surgical re-attachment rate of 70% to 98% [16-19]. 360° endolaser seems to be an important step in reducing the rate of post-operative complications (new retinal breaks and recurrent RRDs). The mean number of laser coagulates placed was 1,056 without a statistically-significant difference between number of coagulates in both groups. No statistically-significant differences between the superior, nasal, temporal or inferior localization of the retinal breaks and the reoperation rate was found. The only factor that influenced the outcome in this study was the positive effect of a combined encircling band. Presence of an encircling element has been shown to support the vitreous base, ensure meticulous removal of the peripheral vitreous during vitrectomy, as well as decrease the traction at the vitreous base [20,21]. The most effective treatment in the study was the combination of PPV and an encircling band with intraoperative 360° laser therapy. Eyes that underwent an encircling band procedure were less likely to be reoperated than those without an encircling band (3.65% vs. 9.61%, p-value=0.002, Fisher exact test). The strength of this study is the large amount of data reported for retinal redetachment after vitrectomy for the treatment of PRRD.
Limitations
Limitations of the current study are the retrospective design, that this study is a single- center study, the lack of a control group and the missing data. All the patients in this trial were followed for at least 8 weeks post-operatively. 44 eyes were lost for follow-up. Ciccone et al. [22] discuss the feasibility and effectiveness of a disease and care management in the primary health system [22]. They introduce the concept of a care manager, serving as a bridge between specialists and patients, collaborating with the patients’ doctors while working directly with individual patients. The care manager helps to coordinate patient care by managing the patient follow-up appointments, providing the necessary information and achieve better compliance with care recommendations. A care manager has the skills in understanding people and is sympathetic to his patients’ problems so that patients can complete the care program with optimal results. We believe that with such a care management the number of lost for follow-up patients will be lower and there will be less missing data in the future [22].
Conclusion
PPV combined with 360° peripheral endolaser is an effective treatment and leads to successful anatomical reattachment in patients with PRRD. The primary anatomic success rate was 91.16%. The only factor that influenced the outcome in this study was the positive effect of a combined encircling band.
References
- Ghazi NG, Green WR. Pathology and pathogenesis of retinal detachment. Eye(Lond). 2002;16:411-21.
- Chaturvedi V, Basham RP, Rezaei KA. Scleral depressed vitreous shaving 360 laser, and perfluoropropane (C3 F8) for retinal detachment. Indian J Opthalmol. 2014;62:804-8.
- The SPR study group. View 2: The case for primary vitrectomy. Br J Ophthalmol. 2003;87:784-7.
- Machemer, R, Buettner H, Norton EW, et al. Vitrectomy: A pars plana approach. Trans Am Acad Ophthalmol Otolaryngol1971; 75:813-20.
- Bretz F, Hothorn T, Westfall P.Multiple comparisons using R. CRC Press. Boca Raton. 2011.
- Development Core Team (2015) R: A language and environment forstatisticalcomputing. R Foundation for Statistical Computing,Vienna, Austria. ISBN 3-900051-07-0. [URLhttp://www.R-project.org.]
- Li W, Sun G, Wu R, et al. Longterm results after phacovitrectomy and foldable intraocular lens implantation. Acta Ophthalmol. 2009;87(8):896-900.
- Simcock PR, Scalia S.Phaco-vitrectomy for full-thickness macular holes. Acta Ophthalmol Scand.2000;78(6):684-6.
- Misra A, Burton RL.Incidence of intraoperative complications during phacoemulsification in vitrectomized and non-vitrectomized eyes: prospective study.J Cataract Refract Surg. 2005;31(5):1011-4.
- Laidlaw DA, Karia N, Bunce C, et al. Is prophylactic 360-degree laser retinopexy protective? Risk factors for retinal redetachment after removal of silicone oil. Ophthalmology. 2002;109:153-8.
- Li H, Zhu X, Jiang D. Risk factors of retinal redetachment after expected silicone oil removal. Yan KeXueBao. 2005;21:92-4, 98.
- Ahluwalia HS, Gray RH. Prophylactic argon laser retinopexy prior to removal of silicone oil: a pilot study. Eye (Lond). 1998;12 (Pt 3a):490.
- Falkner-Radler CI, Graf A, Binder S. Vitrectomy combined with endolaser or an encircling scleral buckle in primary retinal detachment surgery: A pilot study. ActaOphthalmol. 2015;93(5):464-9.
- Nagpal MP, Videkar RP, Nagpal KM. Factors having implications on re-retinal detachments after silicone oil removal. Indian J Ophthalmol 2012;60:517-20.
- Koh HJ, Cheng, L, Kosobucki B, et al. Prophylactic intraoperative 360 degrees of laser retinopexy for prevention of retinal detachment. Retina. 2007;27:744-9.
- Dugas B, Lafontaine PO, Guillaubey A, et al.The learning curve for primary vitrectomy without scleral buckling for pseudophakic retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2009;247:319-24.
- Heimann H, Zou X, Jandeck C, et al.Primary vitrectomy for Rhegmatogenous retinal detachment: An analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol2006;244:69-78.
- Mendrinos E, Dang-Burgener NP, Stangos AN, et al. Primary vitrectomy without scleral buckling for pseudophakicRhegmatogenous retinal detachment. Am J Ophthalmol. 2008:28:1063-70.
- Lai MM, Ruby AJ, Sarrafizadeh R, et al.Repair of primary Rhegmatogenous retinal detachment using 25-gauge transconjunctival suture less vitrectomy. Retina.2008;28:729-34.
- Jonas JB, Knorr HL, Rank RM, et al. Retinal detachment after removal of intraocular silicone oil tamponade. Br J Ophthalmol. 2001;85:1203-7.
- Nagpal MP, Videkar RP, Nagpal KM. Factors having implications on re-retinal detachments after silicone oil removal. Ind J Ophthalmol. 2010;60(6):517.
- Ciccone MM, Aquilino A, Cortese F, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6:297-305.