Research Article - Journal of Cardiovascular Medicine and Therapeutics (2025) Volume 9, Issue 1
The evaluation of regional and global myocardial function post Coronary Artery Bypass Graft (CABG) by speckle tracking echocardiography technique.
Mansour Jannati1, Iman Pourgholami1, Khalil Zarrabi2, Mehdi Atari3, Firoozeh Abtahi1*
1Department of Cardiovascular Surgery, Shiraz University of Medical Sciences, Shiraz, Iran
2Department of Cardiovascular Surgery, Iranian hospital, Dubai, UAE
3Department of Cardiovascular Surgery, Gerash University of Medical Sciences, Fars, Iran
*Corresponding Author:
-
Firoozeh Abtahi
- Department of Cardiovascular Surgery, Shiraz University of Medical Sciences, Shiraz, Iran
E-mail:abtahifa@sums.ac.ir
Received: 03-October-2024, Manuscript No. AACMT-23-115777; Editor assigned: 05-October-2024, AACMT-23-115777 (PQ); Reviewed: 19-
October-2024, QC No. AACMT-23-115777; Revised: 17-January-2025, Manuscript No. AACMT-23-115777 (R); Published:
24-January-2025, DOI: 10.35841/aacmt.9.1.170
Citation: Jannati M, Pourgholami I, Zarrabi K, et al. The evaluation of regional and global myocardial function post Coronary Artery Bypass Graft (CABG) by speckle tracking echocardiography technique. J Cardiovasc Med Ther. 2025;9(1):170.
Abstract
This study aims to evaluate STE to investigate the alterations in global and regional myocardial function after CABG. General and regional parameters were measured for different parts of the myocardium to evaluate the outcome of surgery, dyspnea at rest, dyspnea on exertion, chest pain on exertion, function class, (2D)-STE was performed before and 8-12 weeks after the surgery for the 54 patients. The mean of general parameters including End-Systolic Volume (ESV) (P>0.945), End-Diastolic Volume (EDV) (P>0.816), Ejection Fraction (EF) (P>0.968), and Global Longitudinal Strain (GLS) (P>0.941) were not statistically significant before and after CABG. In spite of the fact that patients' cardiac function improves clinically after CABG surgery, speckle tracking echocardiography findings did not show a statistically significant difference between before and after the surgery in terms of general and regional parameters.
Keywords
Coronary artery disease, Coronary artery graft bypass surgery, Speckle tracking echocardiography, Global longitudinal strain.
Introduction
Coronary Artery Disease (CAD) is one of the primary cardiovascular diseases and the major cause of death in both developed and developing countries [1]. According to current guidelines, Coronary Artery Bypass Graft Surgery (CABG) is treatment of choice for patients with severe CAD, including those with left main CAD and those with three-vessel disease [2].
Left ventricular dysfunction is related to a higher risk of death after cardiac surgery [3]. The baseline LV function may be crucial to formulating a perioperative management plan and risk stratifying perioperative consequences [4,5]. Myocardial deformation evaluation is a method for assessing cardiac function that allows global and regional investigation of myocardial mechanics during the cardiac cycle [6,7]. Myocardial strain quantifies myocardial deformation and can be evaluated in three dimensions: longitudinal, radial, and circumferential [8,9].
Although imaging techniques such as angiography are used extensively, non-invasive recognition of CAD patients remains clinical challenge; many patients show normal or nonobstructive CAD on angiographic evaluations [10]. The CAD diagnosis by echocardiography is typically associated with recognizing Left Ventricle (LV) dysfunction and the Ejection Fraction (EF) evaluation [11]. However, in CAD patients without a history of myocardial infarction, no abnormality in LV wall motion was observed in angiography at rest position [12].
Speckle-tracking imaging is a new sono-graphic technique established in recent years [13]. It can track the myocardial tissue's motion frame by frame in 2D speckles form in the area of interest, it reflects the motion and deformation and obtains the speed, movement, strain, and strain rate of myocardial tissues to evaluate the myocardial motion [14]. STE evaluates the myocardial deformation and follows the abnormalities of ventricular wall motion [15]. STE can distinguish between normal and abnormal myocardial deformation and LV dysfunction [16].
Strain is the percentage alteration in the myocardial segment length compared to its resting length, and Strain Rate (SR) is the rate at which this deformation happens [17]. There is a correlation between longitudinal strain and the LV Ejection Fraction (EF) [14]. In addition, a proper quantitative myocardial deformation evaluation of LV segments is provided by longitudinal strain [18]. The STE longitudinal strain use can determine CAD with good accuracy [19]. Strain and strain rates are homogeneously diffused throughout the myocardium, and slight alterations suggest myocardial dysfunction [20].
Due to the lack of comprehensive research concerning CABG and myocardial dysfunction by STE, the present study sought to gain a novel insight by using speckle tracking echocardiography to assess global and regional changes in myocardial function before and after CABG.
Materials and Methods
Patient selection: In this cross-sectional study, the convenience sampling method was used to obtain the total volume of the sample. Fifty-four CABG candidate patients who were eligible for the study and referred to the cardiovascular clinics of Shahid Faghihi, Namazi, and Alzahra hospitals were selected for the study.
Inclusion and exclusion criteria: Patients with the age between 30 and 70 years who had informed consent to participate in the study with no previous history of angioplasty, myocardial infarction, use of a pacemaker, and CABG entered the study. Exclusion criteria included dissatisfaction to continue the study, history of myocardial infarction, chronic obstructive pulmonary disease, congenital heart disease, and valvular heart disease.
Two-dimensional speckle-tracking echocardiography: After selecting the study population, dyspnea at rest, dyspnea on exertion, chest pain on exertion, function class and 2D-speckle tracking echocardiography was recorded from apical 4-chamber view (General Electric Vivid E9) were performed in patients in two stages: First stage prior the CABG operation and the second stage at least 8-12 weeks after the surgery. In both stages, left ventricular function indices including general parameters such as Ejection Fraction (EF), End-Systolic Volume (ESV), left ventricular end-diastolic volume (EDV), Global 2D Longitudinal LV Strain (GLS), and Segmental 2D Longitudinal LV strain of left ventricular wall and regional parameters in different areas of the myocardial wall such as inferoseptal, anterolateral, anterior, inferior, anteroseptal, and inferolateral were measured.
Speckle tracking analysis: Following the measurement of the standard echocardiographic parameters, all parameters mentioned in the previous section were measured by STE in CABG at both pre- and post-operative times. The software for 2D wall motion tracking (QLAB 9.0 software; Philips Medical Systems, Andover, MA, USA) was used to automatically collect the 2D strain data and analyze the 2D data offline. Furthermore, based on the time-strain curves for each LV segment, the Global Longitudinal Strain (GLS), ESV, EDV, and EF 2D STE parameters were calculated. The LV Systolic Dyssynchrony Index (SDI) was determined by multiplying the Standard Deviation (SD) of the time to peak strain for each of the 16 segments by the RR interval. To create the LV global performance plot, the peak global strain based on all 16 segments was plotted against SDI.
Follow-up: All patients were followed from the date of preoperation to the last available follow-up after CABG or to the 8-12 weeks after discharging of hospital.
Statistical analysis
SPSS statistical v.22 was used for data analysis. Descriptive statistics, including mean and standard deviation for quantitative and frequency variables and percentage for qualitative variables were used to describe the data. After checking the data distribution and non-normality, we used nonparametric tests. Data analysis was performed using Wilcoxon and McNemar's tests. McNemar's test is used to evaluate the similarity of two dependent samples in terms of a dichotomous nominal variable and the Wilcoxon test is used to evaluate the similarity of two dependent samples with a rank and distance scale. A P-value less than 0.05 were considered statistically significant.
Results
In this study, 54 patients who were candidates for CABG surgery and met inclusion criteria were included. The mean and standard deviation of the age of these people was 55.63 ± 5.77, the lowest age included in the study was 45 years, and the highest age was 65 years. Further, 38 men and 16 women participated in this study.
Comparison of parameters before and after CABG surgery
To evaluate CABG surgery effect on general and regional parameters, a paired T-test was used to compare the mean of parameters before and after surgery, and a P-value was reported for each pair of these parameters. The parameters were examined in two categories: General parameters and regional parameters.
General parameters
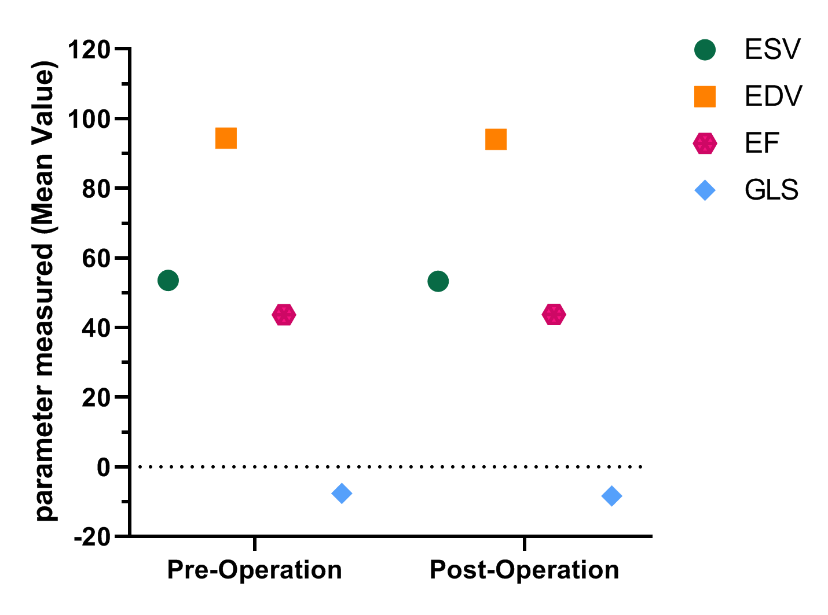
Based on the findings, none of the parameters of ESV, EDV, EF, and GLS were significantly changed before and after CABG surgery (P>0.05), and also illustrate schematically in Figure 1 and Table 1.
Figure 1. The general parameters before and after CABG surgery.
|
|
Mean ± SD |
P-value |
|---|---|---|
|
ESV |
|
0.945 |
|
Pre-operation |
53.49 ± 10.46 |
|
|
Post-operation |
53.24 ± 10.53 |
|
|
EDV |
|
0.816 |
|
Pre-operation |
94.35 ± 15.63 |
|
|
Post-operation |
94.01 ± 15.90 |
|
|
EF |
|
0.968 |
|
Pre-operation |
43.66 ± 8.01 |
|
|
Post-operation |
43.71 ± 7.94 |
|
|
GLS |
|
0.941 |
|
Pre-operation |
-10.03 ± 5.15 |
|
|
Post-operation |
-10.18 ± 5.15 |
|
|
Note: EF: Ejection Fraction; ESV: End-Systolic Volume; EDV: Left Ventricular End-Diastolic Volume; GLS: Global Longitudinal Strain |
||
Table 1. Comparison of general parameters before and after CABG surgery.
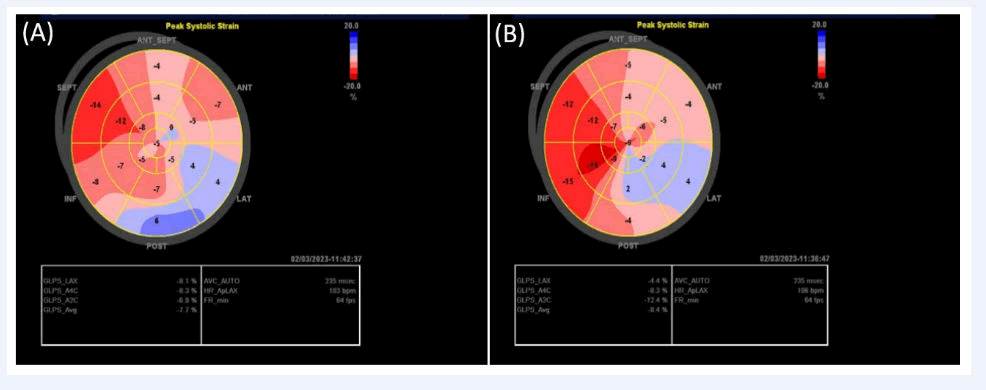
The Global Longitudinal Strain (GLS), is one of important parameter, before and after CABG are shown at Figure 2A and B, respectively. This results indicated in a patient with previous history of inferolateral infacrtion, and moderate LV systolic dysfunction; severely reduced GLS (-7.7%) was noted prior to operation with severely reduced strain of inferolateral and anterolateral wall. After operation some improvement was detected in inferior wall and basal inferolateral wall, with GLS of -8.4%.
Figure 2. Global Longitudinal Strain (GLS), before (2A) and after (2B) CABG, in a patient with previous history of inferolateral infarction, and moderate LV systolic dysfunction; severely reduced GLS (-7.7%) was noted prior to operation with severely reduced strain of inferolateral and anterolateral wall. After operation some improvement was detected in inferior wall and basal inferolateral wall, with GLS of -8.4%.
Regional parameters
The STE findings (before and after surgery) were compared in each area of the myocardial wall, but no significant changes were observed in any of these areas before and after CABG surgery (P>0.05) (Table 2).
|
|
Pre-operation |
Post-operation |
P-value |
|---|---|---|---|
|
Inferoseptal |
|||
|
A. Inferoseptal |
-12.54 ± 5.17 |
-12.35 ± 5.07 |
0.892 |
|
M. Inferoseptal |
-11.92 ± 4.08 |
-11.79 ± 4.03 |
0.901 |
|
B. Inferoseptal |
-9.98 ± 4.35 |
-9.88 ± 4.45 |
0.906 |
|
Anterolateral |
|||
|
A. Anterolateral |
-10.69 ± 3.96 |
-10.52 ± 3.91 |
0.900 |
|
M. Anterolateral |
-9.62 ± 4.42 |
-9.60 ± 4.49 |
0.990 |
|
B. Anterolateral |
-9.56 ± 3.68 |
-9.49 ± 3.72 |
0.958 |
|
Anterior |
|||
|
A. Anterior |
-13.15 ± 6.35 |
-13.11 ± 6.51 |
0.976 |
|
M. Anterior |
-12.86 ± 5.89 |
-13.01 ± 5.87 |
0.884 |
|
B. Anterior |
-13.09 ± 4.94 |
-13.12 ± 4.97 |
0.989 |
|
Inferior |
|||
|
A. Inferior |
-13.49 ± 5.93 |
-13.32 ± 5.98 |
0.972 |
|
M. Inferior |
-14.33 ± 4.69 |
-14.18 ± 4.76 |
0.863 |
|
B. Inferior |
-12.03 ± 5.29 |
-11.94 ± 5.31 |
0.950 |
|
Anteroseptal |
|||
|
M. Anteroseptal |
-11.58 ± 4.06 |
-11.47 ± 4.01 |
0.931 |
|
B. Anteroseptal |
-10.75 ± 5.89 |
-10.73 ± 5.91 |
0.985 |
|
Inferolateral |
|||
|
M. Inferolateral |
-10.77 ± 4.20 |
-10.56 ± 4.10 |
0.873 |
|
B. Inferolateral |
-9.98 ± 5.99 |
-9.92 ± 5.95 |
0.969 |
|
Note: McNemar's test investigated the relationship between rest at dyspnea before and after surgery. |
|||
Table 2. Comparison of the mean of longitudinal strain in walls.
A statistically significant difference was observed before and after surgery (p>0.004) in the below table. In this way, out of 19 people who had rest at dyspnea before the operation, only six people had not improved and 13 people had improved (Table 3).
| Pre rest. at dyspnea | Dyspnea at rest. post | p-value | |
|---|---|---|---|
| Yes | No | ||
| yes | 3 | 16 | .004 |
| no | 3 | 32 | |
Table 3. Relationship between pre and post-operation in dyspnea at rest.
McNemar's test was used to investigate the relationship between dyspnea on exertion before and after the operation; a statistically significant difference was observed before and after the operation (p>0.000). In this way, out of 42 people with dyspnea on exertion before the operation, only 6 had not improved and 36 had improved (Table 4).
| Dyspnea on exertion. pre | Exertion. post dyspnea on | p-value | |
| Yes | No | ||
| yes | 2 | 40 | .000 |
| no | 4 | 8 | |
Table 4. Relationship between pre and post-operation in dyspnea on exertion.
McNemar's test was used to check the relationship between Cp on exertion before and after the operation; a statistically significant difference was observed before and after the operation (p>0.035). In this way, out of 18 people with Cp on exertion before surgery, 9 had not improved and 9 had improved (Table 5).
| Cp on exertion. pre | Cp on exertion. post | p-value | |
|---|---|---|---|
| Yes | No | ||
| yes | 6 | 12 | .035 |
| no | 3 | 33 | |
Table 5. Relationship between pre and post-operation in cp on exertion.
Wilcoxon test was used to check the relationship between function classes before and after the operation. Below table displays a statistically significant difference before and after the operation (p>.000). In this way, most people improved at least one class after the operation (Table 6).
| Function class. pre | Function class. post | p-value | ||
| I | II | III | .000 | |
| II | 24 | 14 | 0 | |
| III | 0 | 12 | 2 | |
| IV | 0 | 0 | 2 | |
Table 6. Relationship between pre and post-operation in function class.
Discussion
STE is a non-invasive imaging technique and a new method for assessing myocardial activity. In addition to assessing the overall activity of the heart, the activity of different myocardial regions can be determined using the longitudinal strain of that region. Very few studies focus on LV function before and after CABG surgery and have shown the function of different parts of the heart tissue using two-dimensional STE. Considering the lower cost and good efficiency of echocardiography, the present study was performed to evaluate the role of STE and compare general and regional parameters of the myocardial wall in CAD patients before and after CABG.
In the present study, 54 candidates for CABG surgery were evaluated and their echocardiographic findings were reported as mean before and after surgery, in addition, their differences before and after surgery was statistically evaluated.
Comparison of the mean of ESV, EDV, EF, and GLS values for each parameter was performed before and after surgery and it was not statistically significant. In evaluating the regional echocardiographic findings of different parts such as the inferoseptal, anterolateral, anterior, inferior, anteroseptal, and inferolateral regions of the myocardium, comparing the results before and after surgery in all parts of the myocardium showed no statistically significant difference.
Scharrenbroich et al. evaluated the use of 2D-STE in the prognosis of Acute Myocardial Infarction (AMI) and chronic Coronary Artery Disease (CAD). In CAD patients, ROC analysis showed that adding endocardial GCS to baseline characteristics and EF to a regression model significantly increased the prediction of cardiac events. However, adding parameters of strain in AMI patients did not improve the prediction of cardiac events.
In a study by Civieri et al., the ventricular dysfunctions were evaluated by the time using STE in juvenile systemic sclerosis patients. At Time 0, electrocardiography was abnormal in three patients, EF has decreased in one patient, LV-GLS was abnormal in three, and RV-GLS was abnormal in five patients. After 18 months, EF remained stable, whereas, at 36 months, the result reduced in seven of nine patients. Moreover, LV-GLS deteriorated. STE was more sensitive than standard echocardiography to detect cardiac involvement. Over time, they observed a gradual deterioration of LV-GLS, an indication of LV dysfunction that is expected by several months the reduction of EF.
In a study by Xu et al., the value of multi-directional strain parameters derived from three-D STE for predicting LV remodeling after ST-Elevation Myocardial Infarction (STEMI) treated with primary Percutaneous Coronary Intervention (PCI) was compared with that of 2D-GLS. In these patients, 2D GLS, 3D GLS, 3D GAS, and 3D GRS but not 3D GCS were determined as independent predictors of LV remodeling after primary PCI, and among them, 3D GLS was the most potent predictor.
In the study of Altiok et al., 2D-STE allowed the prediction of global functional recovery and LV remodeling after AMI with precision similar to that of Late Gadolinium Enhancement (LGE) Cardiac Magnetic Resonance (CMR). Accuracy for predicting segmental functional recovery by transmural deformation analysis using 2D-STE was inferior compared to LGE CMR.
Radwan et al., evaluated the value of GLS in predicting the severity of Coronary Artery Disease (CAD) by two 2D-STE. There was a significant decrease in GLS in a group with significant CAD compared to the group with non-significant CAD. GLS has dramatically decreased by increasing the number of involved vessels.
Limitations
We lack data on patient follow-up because the study was crosssectional. Another limitation of the present study is the measurement of longitudinal strain, not radial and circumferential strains. Another drawback is the absence of a comparison of 3D and 2D-STE. The 2D-derived GLS has been sufficiently shown to be a marker for subclinical myocardial dysfunction, and the earlier studies on 3D-derived GLS has shown similar results to the 2D-derived GLS in terms of the linear relationship between CABG and systolic LV longitudinal dysfunction. These data suggest that subclinical myocardial function in cardiovascular patients can be evaluated using both 2D and 3D-derived GLS. The evaluation of radial and circumferential strains may probably add practical information to the data acquired for future study. By contrasting direct cardiac sympathetic denervation with 3D-STE measurements, future prospective studies should ascertain whether GLS is related to the morbidity and mortality of after CABG during a long period of time.
Clinical implications
Although the CABG procedure is one of the preferred treatment options, it is also one of the main causes of death in patients with cardiovascular disease. Additionally, postoperative patient management is crucial for achieving the best results. Due to the current study's findings, which show that co-existing disease significantly contributes to subclinical EDV and ESV complications and impaired GLS, these patients may be the targets of effective therapy in addition to close observation of the progression of their illness.
Conclusion
Our research is the newly study to investigate the association between myocardial function, CABG surgery, and regional and global functional parameters in patients with CAD. In the present study, although the quality of cardiac function of patients after CABG surgery is improved clinically, it was not statistically significant in ESV, EDV, EF and GLS parameters. We have suggested that further studies are required to further evaluate whether 3D-derived parameters may provide earlier diagnosis and improve the specific management of patients with CAD.
Availability of Data and Materials
All of the data are demonstrated in the study.
Funding
There is no funding for the present study.
Consent for Publication
Not applicable.
Competing Interests
The authors declared no potential conflicts of interest.
Credit Authorship Contribution Statement
Mansour Jannati: MD, Cardiovascular Surgeon, Associated Professor, Study design and Conceptualization, Investigation, sample collection, Data Analyzing, Writing-original draft, Writing-review and editing. Firoozeh Abtahi: MD, Cardiologist, Associated Professor, Corresponding Author, Study design and concept, Investigation, and Writing-original draft. Khalil Zarrabi: MD, Cardiovascular Surgeon, Associated Professor, sample collection and performing the study. Iman Pourgholami: MD, Cardiologist, Assistance Professor, Investigation, literature research and analysis. Mehdi Atari: P.h.D of Biomedical Engineering-Biomaterials and Tissue Engineering, Investigation, data analysis, review & editing. The study is approved by all authors.
Ethics Approval and Consent to Participate
The ethics committee of Shiraz University of Medical Sciences has approved the study (IR.SUMS.MED.REC.1398.389). Informed consent was obtained from all patients to use the patients' clinical information.
References
- Elshafay A, Bendary AH, Vuong HT, et al. Does no-touch technique better than conventional or intermediate saphenous vein harvest techniques for coronary artery bypass graft surgery: a systematic review and meta-analysis. J Cardiovasc Transl Res. 2018;11:483-94.
[Crossref] [Google Scholar] [PubMed]
- Keddeas VW, Swelim SM, Selim GK. Role of 2D speckle tracking echocardiography in predicting acute coronary occlusion in patients with non ST-segment elevation myocardial infarction. Egypt Heart J. 2017;69(2):103-10.
[Crossref] [Google Scholar] [PubMed]
- Enomoto M, Ishizu T, Seo Y, et al. Myocardial dysfunction identified by three-dimensional speckle tracking echocardiography in type 2 diabetes patients relates to complications of microangiopathy. J Cardiol. 2016;68(4):282-7.
[Crossref] [Google Scholar] [PubMed]
- Abd El Moneum MS, Elkeshk ES, El-Rabbat KE, et al. (2019) Comparative assessment of left ventricular function after coronary artery bypass grafting and percutaneous coronary intervention to LAD by speckle tracking echocardiography study. Int J Cardiovasc Acad. 2019 5(4):109.
- Pieri M, Belletti A, Monaco F, et al. Outcome of cardiac surgery in patients with low preoperative ejection fraction. BMC Anesthesiol. 2016;16:1-10.
[Google Scholar] [PubMed]
- Ballo H, Doghman F, Hartikainen J, et al. Speckle-tracking echocardiography for predicting improvement of myocardial contractile function after revascularization: A meta-analysis of prospective trials. Int J Cardiovasc Imaging. 2023;39(3):541-53.
[Crossref] [Google Scholar] [PubMed]
- Marwick TH. Measurement of strain and strain rate by echocardiography: Ready for prime time?. J Am Coll Cardiol. 2006;47(7):1313-27.
[Crossref] [Google Scholar] [PubMed]
- Opdahl A, Helle-Valle T, Skulstad H, et al. Strain, strain rate, torsion, and twist: echocardiographic evaluation. Curr Cardiol Rep. 2015;17:1-4.
[Crossref] [Google Scholar] [PubMed]
- Notomi Y, Shiota T, Popovic ZB, et al. Measurement of ventricular torsion by two-dimensional ultrasound speckle tracking imaging. J Am Coll Cardiol. 2005;45(12):2034-41.
[Crossref] [Google Scholar] [PubMed]
- Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886-95.
[Crossref] [Google Scholar] [PubMed]
- Surkova E, Muraru D, Aruta P, et al. Current clinical applications of three-dimensional echocardiography: when the technique makes the difference. Curr Cardiol Rep. 2016;18:1-3.
[Crossref] [Google Scholar] [PubMed]
- Elhendy A, van Domburg RT, Bax JJ, et al. Significance of resting wall motion abnormalities in 2-dimensional echocardiography in patients without previous myocardial infarction referred for pharmacologic stress testing. J Am Soc Echocardiogr. 2000;13(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Hoit BD. Assessment of left atrial function by echocardiography: Novel insights. Curr Cardiol Rep. 2018;20:1-1.
[Crossref] [Google Scholar] [PubMed]
- Hammoudi N, Watanabe S, Bikou O, et al. Speckle-tracking echocardiographic strain analysis reliably estimates degree of acute LV unloading during mechanical LV support by Impella. J Cardiovasc Transl Res. 2019;12:135-41.
[Crossref] [Google Scholar] [PubMed]
- Wang H, Zhang B, Wu WC, et al. Change of left ventricular geometric pattern in patients with preserved ejection Fraction undergoing coronary artery bypass grafting. J Cardiovasc Transl Res. 2022;15(6):1444-54.
[Crossref] [Google Scholar] [PubMed]
- Saha SK, Kiotsekoglou A, Toole RS, et al. Value of two-dimensional speckle tracking and real time three-dimensional echocardiography for the identification of subclinical left ventricular dysfunction in patients referred for routine echocardiography. Echocardiography. 2012;29(5):588-97.
[Crossref] [Google Scholar] [PubMed]
- D’Andrea A, Sperlongano S, Pacileo M, et al. New ultrasound technologies for ischemic heart disease assessment and monitoring in cardiac rehabilitation. J Clin Med. 2020;9(10):3131.
[Crossref] [Google Scholar] [PubMed]
- Shivu GN, Abozguia K, Phan TT, et al. Increased left ventricular torsion in uncomplicated type 1 diabetic patients: the role of coronary microvascular function. Diabetes Care. 2009;32(9):1710-2.
[Crossref] [Google Scholar] [PubMed]
- Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: A consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018;19(6):591-600.
[Crossref] [Google Scholar] [PubMed]
- Jamal F, Kukulski T, Sutherland GR, et al. Can changes in systolic longitudinal deformation quantify regional myocardial function after an acute infarction? An ultrasonic strain rate and strain study. J Am Soc Echocardiogr. 2002;15(7):723-30.
[Crossref] [Google Scholar] [PubMed]