Research Article - Journal of Public Health Policy and Planning (2022) Volume 6, Issue 10
The Editorials: Personalized and Precision Medicine (PPM) as a Unique Healthcare Model of the Next Step Generation Through the View of Public Health Resources
Sergey Suchkov1-3,6, 13*, Tatiana Makarova1, Marina Moiseyakh2, Noel Rose4,5, Holland Cheng7, Elena Suchkova8, Hiroyuki Abe9,10, Elena Martynova1,11, Sofia Blokh2,12, Steven Dooley14, Mikhail Kovalev151Institute for Global Health, RosBioTech National University, Russia
2A.I. Evdokimov Moscow State Medical & Dental University (MGMSU), Russia
3EPMA (European Association for Prediction, Prevention and Personalized Medicine), Brussels, EU, Belgium
4Johns Hopkins Center for Autoimmune Disease Research and PAHO/WHO Collaborating Center for Autoimmune Disorders, Johns Hopkins Medical Institutions, Baltimore, MD, United States
5Harvard Medical School, Boston, MA, USA
6New York Academy of Sciences, New York, NY, United States
7Department of Molecular and Cellular Biology, College of Biological Sciences, UC Davis, Davis, CA, USA
8Faculty (School) for Ecotechnologies, ITMO, S-P, Russia
9International Society for Personalized Medicine (ISPM), Japan
10Abe Cancer Clinic, Tokyo, Japan
11Self-Employed Physician, Moscow, Russia
12N.F. Filatov Moscow Clinical Pediatric Hospital, Moscow, Russia
13Personalized Medicine Coalition, Washington, DC, United States
14Medical Faculty Mannheim of the University of Heidelberg, Germany
15Department for Obstetrics & Gynecology, Sechenov University, Moscow, Russia
- *Corresponding Author:
- Sergey Suchkov
Department of Personalized Medicine
Precision Nutriciology & Biodesign of The Institute for Global Health & Biotechnology of MGUPP
Moscow, Russia
E-mail: ssuchkov57@gmail.com
Received: 17-Sep-2022, Manuscript No.AAPHPP-22-74961; Editor assigned: 20-Sep-2022, PreQC No. AAPHPP-22-74961 (PQ); Reviewed: 01-Oct-2022, QC No.AAPHPP-22-74961; Revised: 07-Oct-2022, Manuscript No.AAPHPP-22-74961 (R); Published: 15-Oct-2022, DOI: 10.35841/aaphpp-6.10.146
Citation: Suchkov S, Makarova T, Moiseyakh M, et al. The editorials: Personalized and precision medicine (ppm) as a unique healthcare model of the next step generation through the view of public health resources. J Public Health Policy Plan. 2022;6(10):146
Abstract
The medicine of the XXI century being as PPM is able to protect and preserve human health throughout the life. In this regard, an upgraded model of healthcare service, which includes the philosophy, principles and armamentarium of PPM and aimed at identifying the disorder at its pre-early (subclinical) stage, is being created and set up. And healthcare delivery systems are facing fundamental challenges. New ways of organiz-ing those systems based on the different needs of stakeholders’ standards are required to meet these challenges. For instance, while medicine is currently undergoing remarkable developments from its morphological and phenotype orientation to a molecular and genotype orientation, promoting the importance of prognosis and prediction, the discussion about the relevance of genome-based information and technologies for the health care system as a whole and especially for public health is still in its infancy.
Keywords
Personalized and precision medicine (PPM), Healthcare, Public health resources, Morphological and phenotype orientation.
Introduction
No comments but policy formation in the field of individual health promotion and protection is one of the priority tasks of national healthcare systems. Over the course of its history, medicine has given special attention to the already diseased individual, focusing on a type of disorder (nosology) rather than on one’s health or the so-called pre-nosological (or preillness) conditions, the latter being left in the shade.
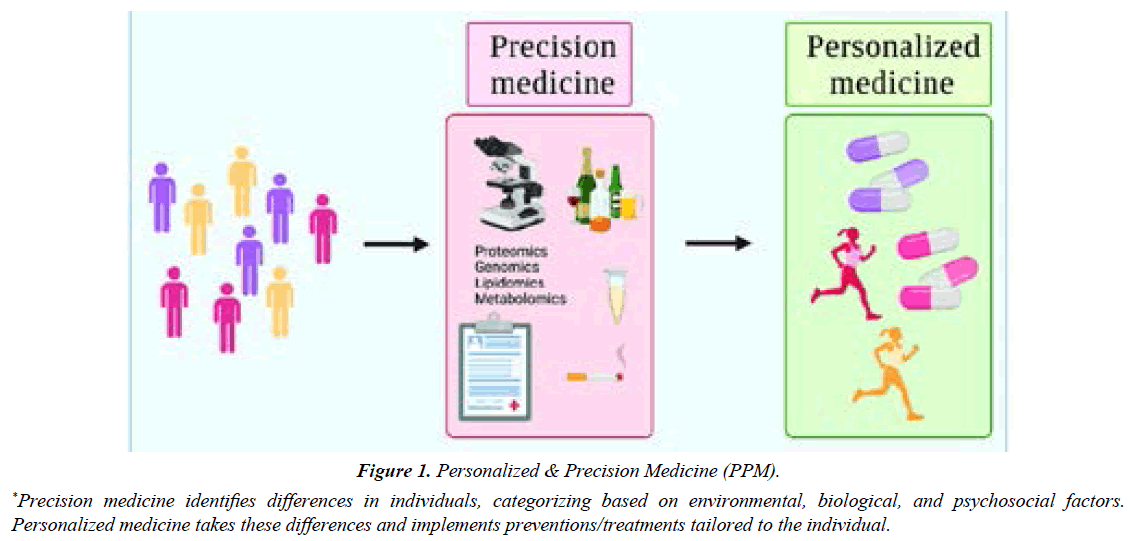
Those speculations along with latest advances in science and technology combined with worldwide practice and personal experience have led us to conclude that the key link in the modern healthcare strategy, namely, a link of Personalized & Precision Medicine (PPM), is missing [1] (Figure 1).
The latter that might exert reliable control over morbidity, mortality and disabling rates and significantly reduce the cost of treatment for those who had fallen ill.
So, canonical health care is becoming increasingly unaffordable in most of the countries, yet it remains ineffective in preventing or effectively treating chronic diseases. The necessity of assessing health services as well analyzing complex new problems, such as ‘genomic inequalities’ in health or the role of biobanks in surveillance systems, support the idea that public health should get involved and moreover take a leading role. Likely benefits as well as potential risks of the integration of personalized and precision genomics into public health interventions (assessment) should be identified [1,3].
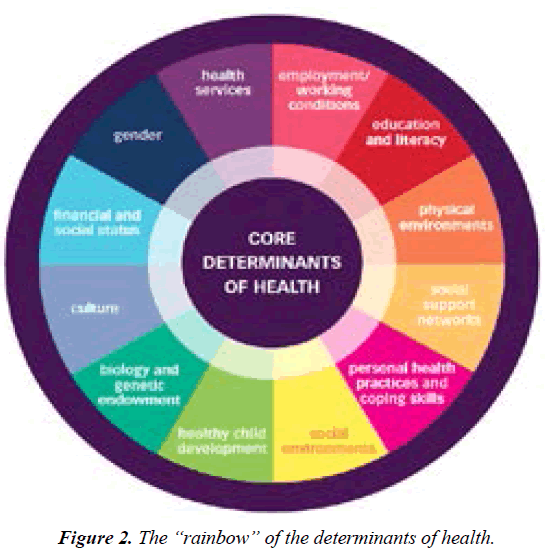
Whilst analyzing and pre-selecting Determinants of Health (Figure 2).
A group of the well-known and recognized experts in the area has presented an evidence-based and well-documented assessment of global trends in medicine and healthcare development. It was noticed that the exclusive value of the next-step model of healthcare services being entitled as PPM, significantly optimizing the cost and efficacy of treatment for those who had fallen ill (a category of patients) and for a category of persons-at-risk [1,2]. This strategy would give a real opportunity to secure preventive, prophylactic, therapeutic and rehabilitative measures whose personalization could have a significantly positive influence on demographics.
Methodological foundations and the Arsenal of PPM
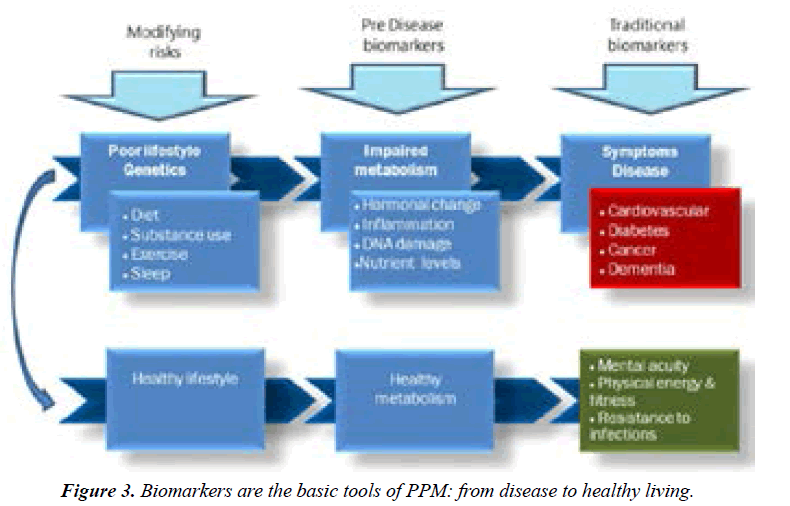
Globally, PPM focuses on predictive and preventive measures that contribute to the development of individualized strategies for managing a healthy lifestyle that stabilize morbidity rates and can help to improve the working capacity of the population. To achieve the goals of value-based healthcare and the implementation of the PPM concept, it is necessary to combine the assets of the newest advances in basic science with clinical medicine, followed by the introduction and promotion of new generation’s translational applications like biomarkers (Figure 3) [2].
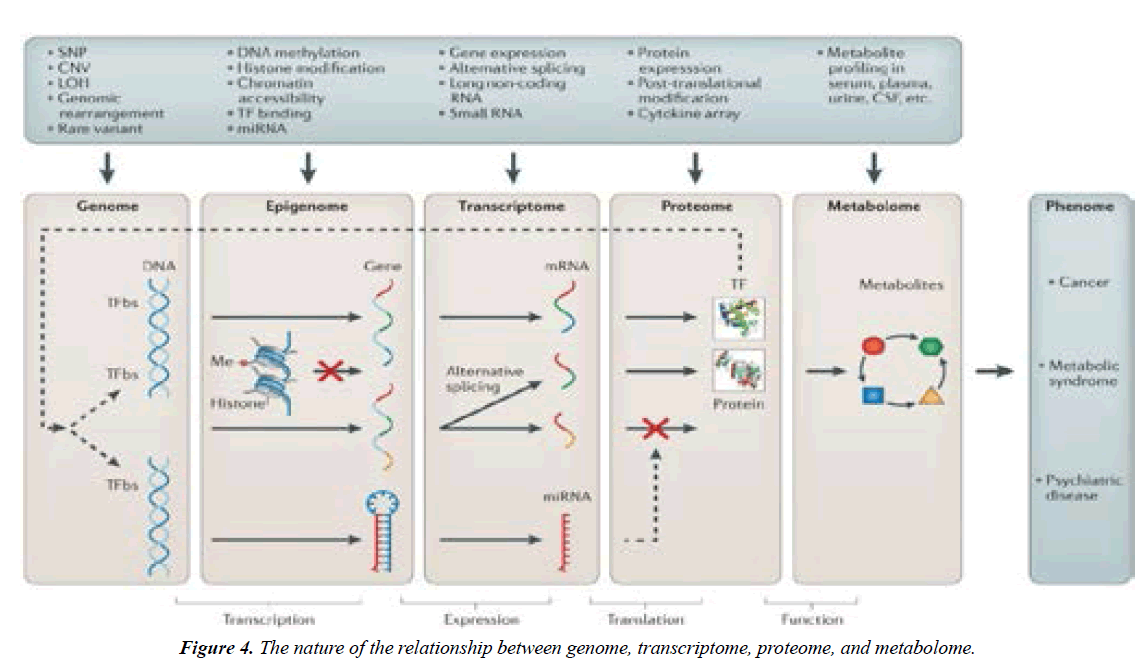
PPM as the big change to forecast, to predict and to prevent is rooted in a big and new science to be rooted from the achievements of OMICS-technologies and bioinformatics which are being implemented into the daily practice to secure visualizing of lesion foci that was previously unknown to clinicians (Figure 4) [2,4].
Meanwhile, a combination of genomic, phenotypic and exposomal (environment-related) biomarkers are becoming of great significance to predict risks of the chronification and thus of disabling since chronic diseases are preceded by a long subclinical (symptom-free) phase or a period of latency [4].
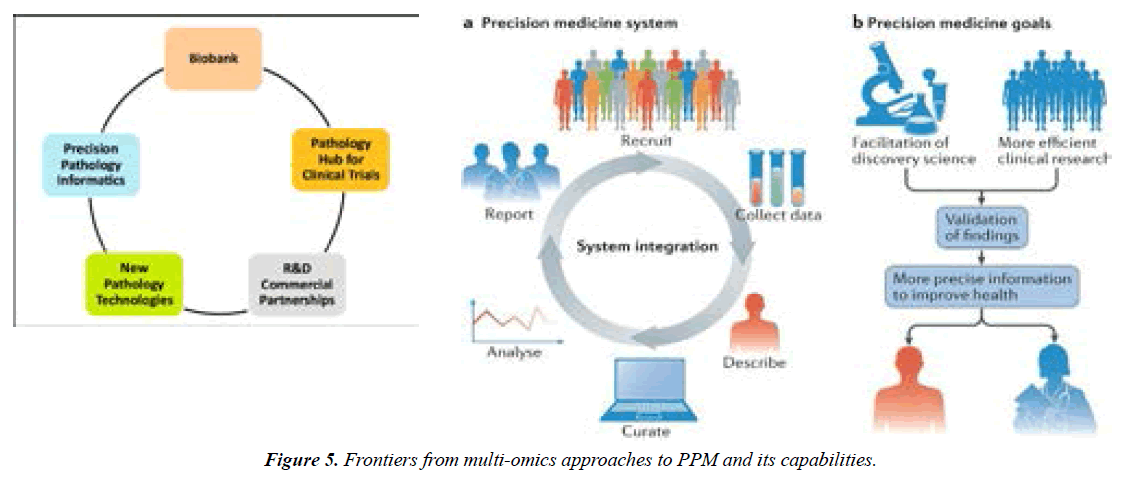
And, for sure, bioinformatics and one more strategic tool, biobanks would provide the proper information about patient's multi-level profiles to be used to tailor precision medical care and thus the health (Figure 5) due to the individual's needs and personalized scenarios [1-3,5].
A global understanding of the factors underlying the burden of a disorder and later on of the clinical illness would provide policymakers, healthcare providers and medical educators with an opportunity to guide preventive initiatives at both individual and community levels.
So, PPM-oriented survey should be based on biomarkers and algorithms to differ essentially from those employed in traditional clinical strategies:
Algorithms for predictive and subclinical diagnostics being individualized, on one hand, and
i. Algorithms for individualized preventive therapy, on the other one.
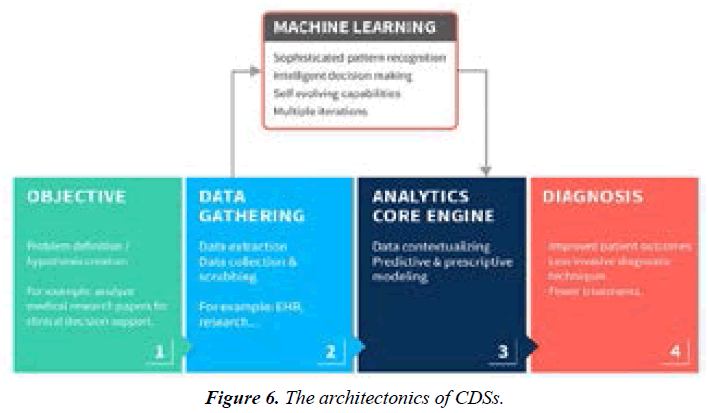
ii. Improved patient outcomes with the use of the biomarker tests must consider not only increased survival or quality of life, but also improved clinical decision support (CDS) & making (Figure 6).
Moreover, biomarkers, potential targets and molecular tools of the latest generation are able to control the latent stages of disease progression and thus to monitor the patients at any stages. For instance, the molecular profile of an individual patient and their disease influences the effect of a medicine; and biomarker diagnostics help to target the right medicine to the right patient. So, across a variety of therapeutic areas, an increasing number of treatments are becoming personalized, being based on principles of precision biomarker-based targeting whilst getting the treatment targeted.
Personalized Health Management: A new format of interaction between a person-at-risk and medical advisor
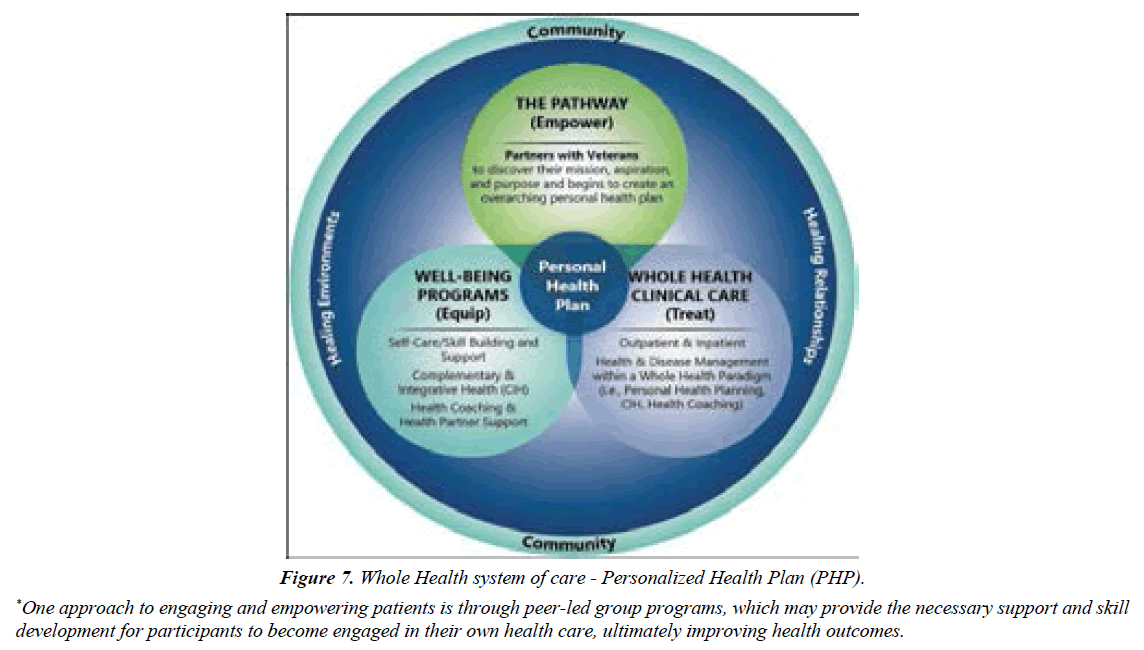
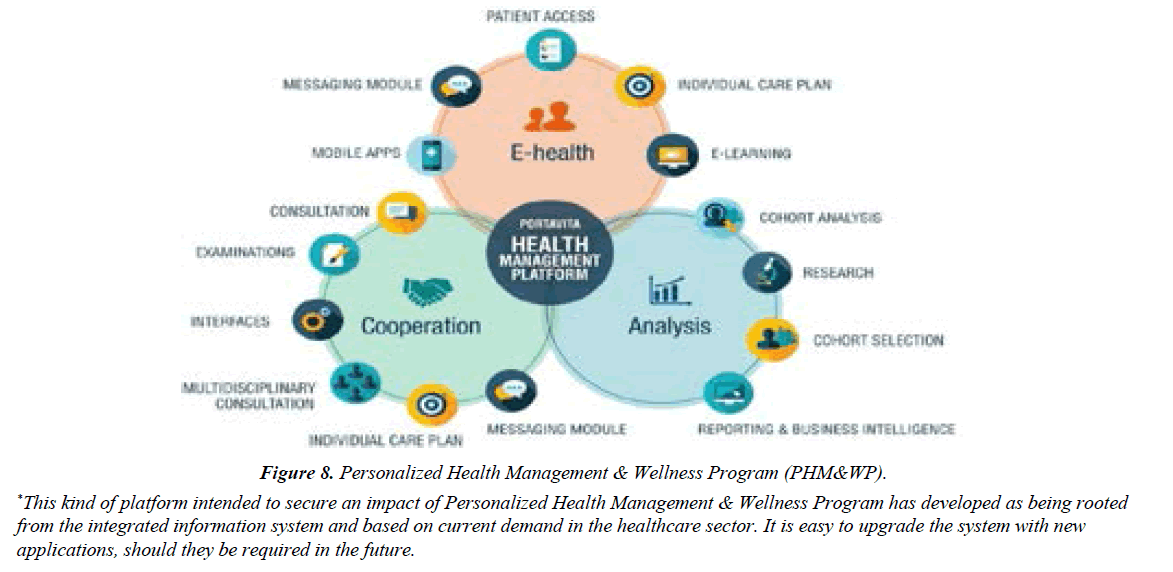
Opportunities for both patients and their physicians exist at every stage of disease initiation and progression to develop an evidence-based Personalized Health Plan (PHP) addressing lifestyle, risk modification and disease management (Figure 7), and later, Personalized Health Management & Wellness Program (PHM&WP) (Figure 8).
Figure 7: Whole Health system of care - Personalized Health Plan (PHP).
*One approach to engaging and empowering patients is through peer-led group programs, which may provide the necessary support and skill development for participants to become engaged in their own health care, ultimately improving health outcomes.
Figure 8: Personalized Health Management & Wellness Program (PHM&WP).
*This kind of platform intended to secure an impact of Personalized Health Management & Wellness Program has developed as being rooted from the integrated information system and based on current demand in the healthcare sector. It is easy to upgrade the system with new applications, should they be required in the future.
Individuals to be under regular monitoring that helps to detect pathological shifts at subclinical stages have a higher life expectancy and are able-bodied up to 8–15 years more than those under traditional treatment. This means that the society would save more than US$20,000–40,000 per person annually. At the community level, the annual savings from each individual may vary from several thousands to several tens of thousands U.S. dollars. In the area of oncology, for instance, the latter means that as little as a 10 percent reduction in cancer would translate into a savings of 4.4 trillion US dollars to society. As you might feel, besides the scientific and clinical challenges, there are economic hurdles.
Meanwhile, implementation of PPM would require the adjusted technology for proper interpretation of diagnostic and predictive data before the current model “physician-patient” could be gradually displaced by a “medical advisor-healthy persons-at-risk” model. This approach should be based on postulates which will change the incarnate culture and social mentality. Due to our viewpoint, all healthcare professionals of the future should be educated to deliver patient-centric care as members of interdisciplinary teams, emphasizing evidence-based practice, quality improvement approaches and bioinformatics.
That concerns the need for novel training programs since the society is in bad need of large-scale dissemination of novel systemic thinking and minding. And upon construction of the new educational platforms in the rational proportions, there would be not a primitive physician created but a medical artist to be able to enrich flow-through medical standards with creative elements to gift for a patient a genuine hope to survive but, in turn, for a person-at-risk – a trust for being no diseased.
So, the existing medical education would strongly need to be restructured to involve along with traditional graduate and post-graduate training, pre-graduate preliminaries to disclose for schoolchildren the mysteries of the evidence-based medicine and PPM as the entity. For doctors, PPM poses major medical education and clinical practice challenges.
The next decade will provide a window of opportunity to establish infrastructures, across Europe and the globe, that will enable the scientific advances to be effectively and efficiently translated into evidence-based policies and interventions that improve population health. Policymakers now have the opportunity to protect consumers, to monitor the implications of OMICS-technologies, and genomics, in particular, for health services, and to assure that the latest advances will be taped to prevent disease and improve health. We now have the chance to prepare public health professionals, the public and policymakers for the changes to come [1-3,6].
Interdisciplinary approach to the implementation of the PPM model in real life
In the era of PPM, digital technologies, drug discovery and development face unprecedented opportunities for product and business model innovation, fundamentally changing the traditional approach of how drugs are discovered, developed and marketed [1,7]. Critical to this transformation is the adoption of new technologies in the drug development process, catalyzing the transition from serendipity-driven to data-driven medicine. This paradigm shift comes with a need for both translation and precision, leading to a modern Translational Medicine (TraMed) approach to Drug Discovery, Diagnostic Biotech, Personalized Nutriciology and Precision Foodomics, and development [5,8,9].
This tremendous revolution aimed to unveil the global secrecy of the Hi Tech has come in the late 20th and then continued in the 21st century, with smart cross- and transdisciplinary technologies and PPM has witnessed interdisciplinary technology innovations in healthcare with a continuous growth in life expectancy across the globe.
PPM holds tremendous potential to remake the healthcare industry. By applying a deeper understanding of diseases with richer patient data and advanced analytics and then modeling the pathologies, PPM can help physicians tailor medicines and nutriceutics to the needs of individual patients, rather than by broader populations, leading to better outcomes at potentially lower costs [1,8,9].
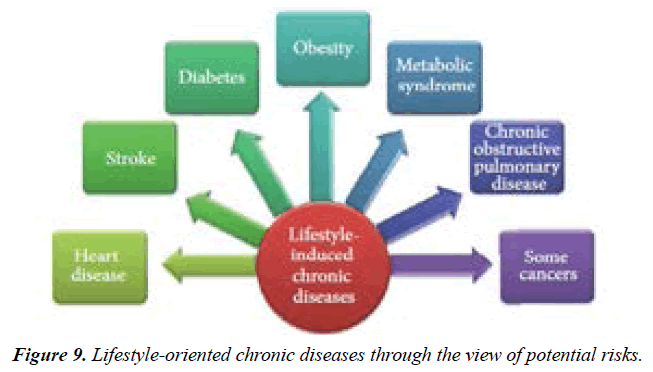
Meanwhile, exchange of ideas and information is vital in promoting and sustaining research and development. It helps in innovation and in finding newer solutions to long battled challenges. The collaboration to be included would also include private players for attaining competitive advantage. PPM is thus a newly developed term referring to an approach in which an individual’s health metrics from point-of-care diagnostics are used to develop Lifestyle Medicine-oriented Preventive, Prophylactic, Therapeutic and Rehabilitative Strategies for improving individual health outcomes in managing chronic disease and thus getting them cured (Figure 9).
In coming year’s next generation biotechnologies and PPMbased approaches, modes and trends will reorient medical practice more towards disease prediction and prevention approaches rather than treating at wider population level(s) for general public healthcare system [3,7].
Honestly, partnership needs to be based on co-production of health and well-being in a delivery model that shifts the balance of power towards local people and communities and away from professionals and formal institutions. Evidence from implementation suggests that the above approach frees up local policymakers, citizens and communities to tailor specific solutions to local problems. Achieving the synergy needed to sustain progress requires coherence of strategy, policy and delivery across the whole system consistent with the values and principles of social justice [7-9].
As you might see from the above-mentioned, PPM has drastically changed and is keeping on changing the landscape of healthcare. And putting PPM-tools in a public health perspective requires an apprehension of the current and future public health challenges. In the future, biological data from individuals can be analyzed with environmental data to determine the drivers of health, lifestyle and well-being.
With a switch to a “fee for value” model, hospitals and healthcare networks already have begun adopting a coordinated-care, team-centered business model with the goal of a cost-effective and efficient health care system. And consumers are doing their part by becoming more proactive in their health care, focusing on prevention and pre-early detection! And as you might see from the above-mentioned, PPM and PPM-based Public Health calls for a transdisciplinary approach to support safe and effective deployment of the new enabling diagnostic and therapeutic technologies not to treat but to get cured!
More accurate methods for measuring disease, pathogens, exposures, behaviors, and susceptibility could allow better assessment of population health and development of policies and targeted programs for preventing disease and managing disorders at the personalized level whilst operating with precision tools and datasets. The initial drive toward PPMbased public health is occurring, but much more work lies ahead to develop a robust evidentiary foundation for use [9].
Conclusion
PPM and PPM-based Public Health call jointly for a transdisciplinary approach to support safe and effective deployment of the new enabling diagnostic, predictive, preventive, prophylactic, therapeutic and rehabilitative technologies not to treat but to get cured!!! So, health policy being based on PPM-based Public Health concept can be the first resource to help us use PPM therapies in a sustainable manner in healthcare systems to secure the public health being the best one.
Since the Grand Change and Challenge to secure our Health and Wellness are rooted not in Medicine, and not even in Science! Just imagine WHERE?! In the upgraded Hi-Tech Culture!
And thus the above-mentioned PPM and PPM-based Public Health model would need for novel training since the society is in bad need of large-scale dissemination of novel systemic thinking and minding. The latter is expected will create the future generation of creative thinkers, entrepreneurs and clinical leaders! And upon construction of the new educational platforms in the rational proportions, there would be not a primitive doctor created but a medical artist to be able to enrich flow-through medical standards with creative elements to gift for a patient a genuine hope to survive but, in turn, for a person-at-risk – a trust for being no diseased. And only Creative Minds would be able to Re-Imagine Healthcare, to Transform Procedures and Prescriptions and to Augment Physician Capabilities to secure the impact of PPM in the near future to come and to re-shape tomorrow’s healthcare whilst doing it today.
Our global challenge is that the new guidelines should create the robust juristic and economic platforms for advanced medical services utilizing the cost-effective models of risk assessments followed by tailored preventive treatments focused on the precursor stages of chronic diseases. And, no doubt, next generations will speak about the XXI century as a time, when medicine became preventive and personalized, and its outcomes predictive and guarantied.
References
- Suchkov SV. Personalized & Precision Medicine as a New Model of the Healthcare Services. InV Russian Congress of Laboratory Medicine 2019 Sep 12.
- Cohrs RJ, Martin T, Ghahramani P, et al. Translational medicine definition by the European Society for Translational Medicine.
- Dzau VJ, Ginsburg GS, Chopra A, et al. Realizing the full potential of precision medicine in health and health care: a vital direction for health and health care. NAM Perspectives. 2016.
- Bodrova TA, Kostyushev DS, Antonova EN, et al. Introduction into PPPM as a new paradigm of public health service: an integrative view. EPMA Journal. 2012 Dec;3(1):1-1.
- Zagotto G, Bortoli M. Drug design: where we are and future prospects. Molecules. 2021;26(22):7061.
- Gorochowski TE, Karr JR, Parmeggiani F, et al. Computer-Aided Biodesign Across Scales. Front Bioeng Biotechnol. 2021;9:700418.
- Augustin DA, Yock CA, Wall J, et al. Stanford’s Biodesign Innovation program: Teaching opportunities for value-driven innovation in surgery. Surg. 2020 Mar 1;167(3):535-9.
- Haines A. Health in the bioeconomy. Lancet Planet Health. 2021 Jan 1;5(1):e4-5.
- Khanal O, Lenhoff AM. Developments and opportunities in continuous biopharmaceutical manufacturing. InMAbs 2021(Vol. 13, No. 1, p. 1903664). Taylor & Francis.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref