Research Article - Biomedical Research (2017) Volume 28, Issue 5
The application of polyetheretherketone cage for lumbar fusion and the pedicle screw-based internal fixation in senile lumbar degenerative diseases
Ping Wang1*, Huiping Zhang2, Litong Liu1, Chunlei Wu1 and Hao Wang11Department of Orthopaedic, Tianjin 254th Hospital of People's Liberation Army, PR China
2Department for Aircrew, Tianjin 254th Hospital of People’s Liberation Army, PR China
- *Corresponding Author:
- Ping Wang
Department of Orthopaedics
Tianjin 254th Hospital of People's Liberation Army
PR China
Accepted date: June 23, 2016
Abstract
Objective: Our objective is to analyse the clinical effect and safety of Polyetheretherketone (PEEK) cage for lumbar fusion and the pedicle screw-based internal fixation in senile lumbar degenerative diseases, and further discuss the value of clinical application.
Methods: 172 patients with senile lumber degenerative diseases admitted in our hospital during March, 2013-March, 2016 were selected, which were divided into the observation group and control group according to the random number method with 86 cases in either group. All the patients received lumbar inter-body fusion and pedicle screw-based internal fixation, in the observation group the material for inter-body infusion was PEEK and in the control group was titanium alloy. The surgery condition and complications in two groups were compared, and Japanese Orthopaedic Association (JOA) scores, Oswestry disability index (ODI) scores, ranges of joint motion, disc space heights and fusion rates were also observed to explore the applicable value of PEEK cage for lumbar fusion in senile lumbar degenerative diseases.
Results: The operation time and intraoperative blood loss in two groups were not statistically different (P>0.05); there was no infection or nerve root injury and no looseness or breakage of internal fixation during follow-up, the bone graft recovered well. Compared with before surgery, the JOA scores were increased and ODI scores were decreased at 3 and 6 months after surgery, which were statistically significant (P<0.05), JOA and ODI scores between two groups at the same stages after surgery were not statistically different (P>0.05). Compared to before surgery, the motion ranges of instrumented segments in two groups were both decreased, and the motion ranges and the disc space heights of adjacent segments were both increased. After 6 months, the motion ranges of instrumented segments and adjacent segments and the disc space heights in the observation group were higher than the control group, which were statistically significant (P<0.05); The fusion rates of bone graft between two groups at the same stages after surgery were not statistically different (P>0.05).
Conclusion: The clinical effects and safety of PEEK for lumbar fusion and the pedicle screw-based internal fixation in senile lumbar degenerative diseases are good. PEEK cage can better improve the range of joint motion and disc space height compared with titanium alloy cage, which is worthy of further application.
Keywords
Polyetheretherketone, Interbody fusion cage, Pedicle screw-based internal fixation, Senile, Lumbar degenerative diseases
Introduction
The lumbar degenerative diseases include lumbar intervertebral disc protrusion, lumbar degenerative spondylolisthesis and lumbar spinal stenosis et al. which are a common orthopaedic disease. The nerve compression symptoms including osphyalgia and lumbocrural pain caused by lumbar degenerative diseases can significantly affect the work and life of patients [1,2]. Decompression, internal fixation and bone graft fusion are the preferred methods to treat lumbar degenerative diseases. The conventional rigid fixation is good at firmly fixing the spine, however, it causes stress shielding which may cause exercise capacity loss of some segments and further accelerate the degenerative disorder of the adjacent segments. Thus, in the recent years, pedicle screw combined with intervertebral fusion in treating lumbar degenerative diseases has been widely applied, and more and more people choose semi-rigid fixation to improve the stress conduction and distribution to further promote the intervertebral fusion [3,4]. Polyetheretherketone (PEEK) cage is a semi-rigid dynamic lumbar stability instrument, which has been widely applied in the treatment of lumbar degenerative diseases. However, in our country titanium alloy cage is mainly applied and the application of PEEK cage is still not extensive. In this study, the clinical effects and safety of PEEK cage for lumbar fusion and the pedicle screw-based internal fixation in treating lumbar degenerative are discussed to provide a theoretical basis for the application of PEEK cage [5-9].
Materials and Methods
General data
172 patients with senile lumbar degenerative diseases admitted in our hospital during March, 2013~March, 2016 were selected, which were divided into the observation group and control group according to the random number method with 86 cases in either group. The age, gender, disease type, disease segment and fusion type in two groups were not statistically different (P>0.05), which were statistically comparable, as shown in Table 1. This study has been approved by the Ethics Committee of our hospital, and the patients or their surrogates were informed and signed the informed consent form.
| Index | Observation group (n=86) | Control group (n=86) | P value | |
|---|---|---|---|---|
| Age (year) | 68.15±4.81 | 68.23±4.37 | >0.05 | |
| Gender | Male | 35 (40.70) | 39 (45.35) | >0.05 |
| Female | 51 (59.30) | 47 (54.65) | ||
| Type | Lumbar intervertebral disc protrusion | 44 (51.16) | 46 (53.49) | >0.05 |
| Lumbar spinal stenosis | 21 (24.42) | 18 (20.93) | ||
| Lumbar degenerative spondylolisthesis | 12 (13.95) | 11 (12.79) | ||
| Lumbar spine instability syndrome | 9 (10.47) | 11 (12.79) | ||
| Segment | L2/3 | 15 (17.44) | 14 (16.28) | >0.05 |
| L3/4 | 26 (30.23) | 25 (29.07) | ||
| L4/5 | 44 (51.16) | 39 (45.35) | ||
| L5/S1 | 19 (22.09) | 22 (25.58) | ||
| Fusion type | Single segmental fusion | 68 (79.07) | 72 (83.72) | >0.05 |
| Double segmental fusion | 18 (20.93) | 14 (16.28) | ||
Table 1: Comparison of general data between two groups (n/%).
Inclusion criteria and exclusion criteria
Inclusion criteria: Patients meet the diagnostic criteria of lumbar degenerative diseases and conservative treatment could not improve the symptoms; Age higher than 60 complicated with severe lumbar spine instability, the vertebral body shifting more than 4 mm or the change of intervertebral angle more than 10; Patients and their surrogates both understood the methods and objectives in this study and voluntarily participated in this study.
Exclusion criteria: Patients complicated with lumbar vertebra fracture or severe osteoporosis (T<2.5); Patients complicated with severe heart, liver or lung dysfunction; Patients have lumbar surgery history; Body Mass Index (BMI) higher than 30 kg/m2, Meyeding grade of lumbar spondylolisthesis higher than 2, or the scoliosis angle higher than 20°.
Methods
Surgical regimen: The patients in both groups received lumbar intervertebral fusion and the pedicle screw-based internal fixation. The patients received intubation and general anaesthesia at prone position, and then the diseased location and instrumented segment were confirmed under C-arm X-ray machine [10]. The skin and subcutaneous tissue were opened up through post middle approach of the diseased spine location, and subperiosteal bilateral paravertebral muscles were peeled to sufficiently explore the spinous process, vertebral plate and bilateral zygapophysis of instrumented segment. The suitable pedicle screw was selected according to the type and diseased segment. The spinous process and the bilateral paravertebral of the diseased segment were removed, and the surrounding proliferated tissue and fibrous tissue were removed [11,12]. After decompressing the interbody fusion was completed, and the different interbody fusion materials were selected in different groups: in the observation group PEEK cage was selected (Figure 1), in the control group titanium alloy cage was selected. After that the vertebral body was opened up and bone graft was implanted, the bone was compacted and the operation was confirmed again. After that, patients received routine flushing; indwelling drainage and then the incision was closed. Antibiotics were routinely administrated for 24-72 hours after the surgery, and patients were requested to lie down at horizontal position without pillow [13-17]. At 1 day after the surgery the drainage tube was removed, at 3 weeks after the surgery patients could get out of bed with waistline to do exercise and recover the function, and 3 months after the surgery the patients could do normal exercise without waistline.
Observational indexes: The surgery condition and the postoperative complications were recorded, and the patients were followed up for 6 months by telephone follow-up and outpatient follow-up. Japanese Orthopaedic Association (JOA) scores, Oswestry disability index (ODI) scores, range of joint motion, disc space heights and fusion rates before surgery, at 3 and 6 months after surgery were recorded and compared. The criterion of bone graft fusion is that X-Ray shows the bone graft space is completely filled by bone trabecula and there was no light transmitting.
Statistical analysis
All the data in this study were analysed by SPSS18.0. The numeration data were presented as (n/%) and analysed by χ2 test. The measurement data were presented as (x ± s). When the data fit a normal distribution, independent t-test was used for analysis if the variances are equal and adjusted t-test was used for analysis if the variances were unequal. When the data don't fit a normal distribution the data were presented as M (Q1, Q3), and Wilcoxon rank-sum test was used for analysis. P<0.05 was considered as statistically significant.
Results
The surgery condition and complications
The operation time and intraoperative blood loss in two groups were not statistically different (P>0.05) , as shown in Table 2; there was no infection or nerve root injury and no looseness or breakage of internal fixation during follow-up, the bone graft recovered well.
| Group | Case number | Operation time (min) | Intraoperative blood loss (ml) |
|---|---|---|---|
| Observation group | 86 | 109.83 ± 21.24 | 273.96 ± 81.50 |
| Control group | 86 | 110.42 ± 25.53 | 280.75 ± 80.34 |
| P value | -- | >0.05 | >0.05 |
Table 2: Comparison of the condition during surgery (͞x ± s).
The changes of JOA scores and ODI scores
Compared with before surgery, the JOA scores were increased and ODI scores were decreased at 3 and 6 months after surgery, which were statistically significant (P<0.05), JOA and ODI scores between two groups at the same stages after surgery were not statistically different (P>0.05) (Table 3).
| Group | Stage | JOA score | ODI score |
|---|---|---|---|
| Observation group (n=86) | Before surgery | 5.31 ± 1.26 | 35.39 ± 7.44 |
| 3 months after surgery | 20.37 ± 6.58* | 20.15 ± 5.39* | |
| 6 months after surgery | 24.17 ± 6.34* | 12.17 ± 3.05* | |
| Control group (n=86) | Before surgery | 5.29 ± 1.33 | 35.47 ± 6.25 |
| 3 months after surgery | 20.45 ± 6.22* | 22.46 ± 5.52* | |
| 6 months after surgery | 24.08 ± 6.08* | 12.24±3.17* | |
| Note:*P<0.05 compared with before surgery. | |||
Table 3: Comparison of JOA scores and ODI scores between two groups before and after surgery (score, ͞x ± s).
The changes of motion range and the disc space height
Compared to before surgery, the motion ranges of instrumented segments in two groups were both decreased, and the motion ranges and the disc space heights of adjacent segments were both increased. After 6 months, the motion ranges of instrumented segments and adjacent segments and the disc space heights in the observation group were higher than the control group, which were statistically significant (P<0.05) (Table 4).
| Group | Stage | Motion angles of instrumented segment (°) | Motion ranges of adjacent segments (°) | Disc space height (mm) |
|---|---|---|---|---|
| Observation group (n=86) | Before surgery | 7.83 ± 2.01 | 7.63 ± 1.55 | 5.89 ± 1.30 |
| 3 months after surgery | 3.96 ± 1.48* | 8.79 ± 2.04* | 11.46 ± 1.55* | |
| 6 months after surgery | 4.23 ± 1.55* | 9.35 ± 2.26* | 10.37 ± 0.82* | |
| Control group (n=86) | Before surgery | 7.91 ± 2.23 | 7.60 ± 1.58 | 5.88 ± 1.26 |
| 3 months after surgery | 1.85 ± 0.47*# | 8.41 ± 1.39* | 11.50 ± 1.63* | |
| 6 months after surgery | 2.04 ± 0.65*# | 8.52 ± 1.43*# | 9.08 ± 0.92*# | |
| Note:*P<0.05 compared with before surgery; #P<0.05 compared with the observation group at the same stage. | ||||
Table 4: Comparison of motion range and the disc space heights between two groups before and after surgery (͞x ± s).
The change of bone graft fusion rate
The fusion rates of bone graft between two groups at the same stages after surgery were not statistically different (P>0.05) (Table 5).
| Group | Case number | 1 month after surgery | 3 months after surgery | 6 months after surgery |
|---|---|---|---|---|
| Observation group | 86 | 48 (55.81) | 63 (73.26) | 86 (100.00) |
| Control group | 86 | 47 (54.65) | 60 (69.77) | 86 (100.00) |
| P value | -- | >0.05 | >0.05 | >0.05 |
Table 5: Comparison of bone graft fusion rate between two groups after surgery (n/%).
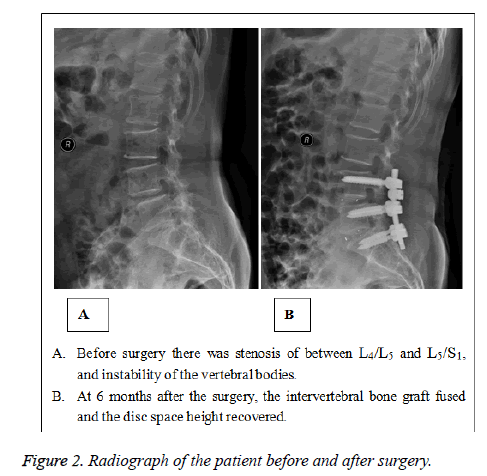
Typical case
A 67-year old female patient, before surgery the X-Ray showed that there was instability of L4/L5 and L5/S1.
Diagnosis: lumbar spinal stenosis, lumbar spondylolisthesis. The patient received PEEK cage for lumbar fusion and pedicle screw-based internal fixation. After 6 months, the bone graft fused, the internal fixation was stable, the motion range of instrumented segment was 4.31°, the motion range of the adjacent segment was 9.40°, and the disc space height was 10.52 mm. As shown in Figure 2.
Discussion
To the senile degenerated lumbar disease patients with mild symptoms, conservative treatment or rehabilitation treatment can effectively relieve the symptoms. However, some patients still cannot be improved by comprehensive treatment after 3-6 months, and then surgical treatment is the key to improve the prognosis. Decompression is the central link in treating degenerated lumbar diseases; however, decompression can damage the mechanical structure of the lumbar vertebra and lumbar instability [18-22]. Thus, in the recent years the application of internal fixation and bone graft fusion is getting more attention.
Titanium alloy cage is a common instrument used in lumbar fusion, the component of which is Ti6AI4V titanium alloy. It has several advantages including good biocompatibility and biomechanical characteristics, and the elasticity modulus is close to human skeletal system which has positive significance in ensuring the lumbar segment fixation and stability [23,24]. However, some scholars point out that the application of titanium cage may cause negative effects on instrumented segment and adjacent segment, furthermore, after the surgery the stress concentrates at the titanium alloy cage and pedicle screw, which may aggravate the degeneration of adjacent segments. Besides, senile patients usually have osteoporosis; titanium alloy cage can cause the progress of osteoporosis of upper and lower segments, which further increases the risk of lumbar vertebra fracture [25,26]. Thus, how to find a safe and effective intervertebral fusion cage to replace titanium alloy cage has always been the key point of clinical research.
PEEK has several advantages including high intensity, high sluggishness and good biocompatibility, the elasticity modulus is close to the bone, and the fictional characteristics and its resistance to corrosion are good. Compared with titanium cage, PEEK cage has better elasticity, and the bone can better share the burden on intervertebral fusion. Thus it cannot only ensure the fixation but also increase the pressure stress of intervertebral bone graft to decrease the degeneration risk of adjacent segments [27-30]. In this study, the patients in the observation group and control groups received PEEK cage and titanium alloy cage for lumbar fusion respectively, and the results showed that postoperative JOA and ODI scores between two groups were not statistically different. However, the motion ranges and the disc space heights in the observation group were better than the control group, which further verified the above conclusion. Besides, in this study, we found that the disc space heights after 3 months in two groups were obviously increased, and decreased after 6 months. This is also called height loss of intervertebral space, it is considered to be related to the limited rigidity of intervertebral fusion cage. Meanwhile, excessive abrasion of bony end plate and early postoperative mobility can also cause the height loss of intervertebral space. Thus, in the further clinical practice, on the premise of the consistent material characteristics, we should pay more attention to the operation and postoperative strict bed rest to ensure the operation outcomes and improve the prognosis.
It’s worthy of mention that some scholars consider that due to the high elasticity of PEEK, the postoperative fusion rate of bone graft might be affected. However, our results demonstrated that the fusion rates between two groups at 1 and 3 months after surgery were not statistically different. And the fusion rate in the observation group after 6 months was up to 100.00%, verifying that it can ensure the bone graft fusion. We consider that this is related to that elasticity modulus of PEEK can decrease stress shielding and promote intervertebral fusion [31]. Meanwhile, PEEK cage has several rows of jigsaw shape bumps on the surface that contacts with the vertebral body, thus after implanting cage, the diagonal jigsaw bumps can directly embed into the vertebral plate of fused vertebral body to avoid the implanted bone graft and smashed bone pieces coming out or entering the spinal canal. It can decrease the risk of nerve compression, and the safety should be affirmed.
Conclusion
In conclusion, PEEK cage for lumbar fusion and pedicle screw-based internal fixation can not only ensure the safety, but also improve the function, motion range and disc space height in senile lumbar degenerative diseases. The clinical effects are close to titanium cage intervertebral fusion, however it has less effects on the motion range and disc space height, thus it is considered that it has optimal clinical effects and is worthy of wide application.
References
- Jacobs WCH, Rubinstein SM, Koes B. Evidence for surgery in degenerative lumbar spine disorders. Best Pract Res Clin Rheumatol 2013; 27: 673-684.
- Mannion AF, Fekete TF, Porchet F, Haschtmann D, Jeszenszky D. The influence of comorbidity on the risks and benefits of spine surgery for degenerative lumbar disorders. Eur Spine J 2014; 23: 66-71.
- Kai Z, Wei S, Changqing Z. Unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in two-level degenerative lumbar disorders: a prospective randomised study. IntOrthop 2014; 38: 111-116.
- Saleem S, Aslam HM, Rehmani MA, Raees A, Alvi AA. Lumbar disc degenerative disease: disc degeneration symptoms and magnetic resonance image findings. Asian Spine J 2013; 7: 322-334.
- Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 2013; 13: 734-743.
- Brodano GB, Martikos K, Lolli F. Transforaminal lumbar interbody fusion in degenerative disk disease and spondylolisthesis grade I: minimally invasive versus open surgery. J Spinal Disord Tech 2015; 28: 559-564.
- Zigler JE, Delamarter R, Murrey D. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine 2013; 38: 203-209.
- Dagostino PR, Whitmore RG, Smith GA, Maltenfort MG, Ratliff JK. Impact of bone morphogenetic proteins on frequency of revision surgery, use of autograft bone, and total hospital charges in surgery for lumbar degenerative disease: review of the Nationwide Inpatient Sample from 2002 to 2008. Spine J 2014; 14: 20-30.
- Phan K, Rao PJ, Kam AC. Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: systematic review and meta-analysis. Eur Spine J 2015; 24: 1017-1030.
- Han YC, Liu ZQ, Wang SJ. Comparison of unilateral versus bilateral pedicle screw fixation in degenerative lumbar diseases: a meta-analysis. Eur Spine J 2014; 23: 974-984.
- Schatlo B, Molliqaj G, Cuvinciuc V. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison: clinical article. J Neurosurg Spine 2014; 20: 636-643.
- Dong J, Rong L, Feng F. Unilateral pedicle screw fixation through a tubular retractor via the Wiltse approach compared with conventional bilateral pedicle screw fixation for single-segment degenerative lumbar instability: a prospective randomized study: Clin ical article. J Neurosurg Spine 2014; 20: 53-59.
- Olivares-Navarrete R, Hyzy SL, Slosar PJ, Schneider JM, Schwartz Z. Implant materials generate different peri-implant inflammatory factors: poly-ether-ether-ketone promotes fibrosis and microtextured titanium promotes osteogenic factors. Spine (Phila Pa 1976) 2015; 40: 399-404.
- Tateishi T, Kyomoto M, Kakinoki S. Reduced platelets and bacteria adhesion on poly (ether ether ketone) by photoinduced and self-initiated graft polymerization of 2-methacryloyloxyethyl phosphorylcholine. J Biomed Mater Res 2014; 102: 1342-1349.
- Nemoto O, Asazuma T, Yato Y. Comparison of fusion rates following transforaminal lumbar interbody fusion using polyetheretherketone cages or titanium cages with transpedicular instrumentation. Eur Spine J 2014; 23: 2150-2155.
- Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 2013; 13: 734-743.
- Ohtori S, Mannoji C, Orita S. Mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J 2015; 9: 565-572.
- Di Silvestre M, Lolli F, Bakaloudis G. Degenerative lumbar scoliosis in elderly patients: dynamic stabilization without fusion versus posterior instrumented fusion. Spine J 2014; 14: 1-10.
- Ikegami D, Matsuoka T, Miyoshi Y. Proximal junctional failure after long-segment instrumentation for degenerative lumbar kyphosis with ankylosing spinal disorder. Spine 2015; 40: 740-743.
- Ailon T, Shaffrey CI, Lenke LG, Harrop JS, Smith JS. Progressive Spinal Kyphosis in the Aging Population. Neurosurgery 2015; 77: 164-172.
- van Engelen SJ, Bisschop A, Smit TH, van Royen BJ, van Dieen JH. The effect of neighboring segments on the measurement of segmental stiffness in the intact lumbar spine. Spine J 2015; 15: 1302-1309.
- Ikegami D, Matsuoka T, Miyoshi Y. Proximal junctional failure after long-segment instrumentation for degenerative lumbar kyphosis with ankylosing spinal disorder. Spine 2015; 40: 740-743.
- Torrie A, Adams MA. Basic science of spinal degeneration. Surgery (Oxford) 2015; 33: 233-237.
- Duhon BS, Cher DJ, Wine KD. Triangular titanium implants for minimally invasive sacroiliac joint fusion: a prospective study. Glob Spine J 2016; 6: 257-269.
- Lee YH, Chung CJ, Wang CW, Peng YT, Chang CH. Computational comparison of three posterior lumbar interbody fusion techniques by using porous titanium interbody cages with 50% porosity. ComputBiol Med 2016; 71: 35-45.
- Chou WK, Chien A, Wang JL. Biomechanical analysis between peek and titanium screw-rods spinal construct subjected to fatigue loading. Clin Spine Surg 2015; 28: 121-125.
- Abode-Iyamah K, Kim SB, Grosland N. Spinal motion and intradiscal pressure measurements before and after lumbar spine instrumentation with titanium or PEEK rods. J Clin Neurosci 2014; 21: 651-655.
- De Iure F, Bosco G, Cappuccio M, Paderni S, Amendola L. Posterior lumbar fusion by peek rods in degenerative spine: preliminary report on 30 cases. Eur Spine J 2012; 21: 50-54.
- Colangeli S, BarbantiBrodano G, Gasbarrini A, Bandiera S, Mesfin A. Polyetheretherketone (PEEK) rods: short-term results in lumbar spine degenerative disease. J NeurosurgSci 2015; 59: 91-96.
- Chang TK, Huang CH, Liu YC. Biomechanical evaluation and comparison of polyetheretherketone rod system to traditional titanium rod fixation on adjacent levels. Formosan Journal of MusculoskelDisord 2013; 4: 42-47.
- Abode-Iyamah K, Kim SB, Grosland N. Spinal motion and intradiscal pressure measurements before and after lumbar spine instrumentation with titanium or PEEK rods. J Clin Neurosci 2014; 21: 651-655.