Case Report - Ophthalmology Case Reports (2021) Volume 5, Issue 6
Spontaneous separation of epiretinal membrane secondary to branch retinal vein occlusion after a series of intravitreal injection
Altintas AGK*
Saglik Bilimleri University Ulucanlar Eye Hospital, Ankara ,Turkey
- Corresponding Author:
- Ayse Gul Kocak ALTINTAS
Saglik Bilimleri University Ulucanlar Eye Hospital,
Ankara ,Turkey
Email: aysegulkaltintas@hotmail.com
Phone: 00905327988488
Accepted date: September 21 2021
Citation: Altintas AGK. Spontaneous separation of epiretinal membrane secondary to branch retinal vein occlusion after a series of intravitreal injection.Ophthalmol Case Rep. 2021;5(6):1-5.
Abstract
A rare case with developing and spontaneous separation of Epiretinal Membrane (ERM) during the treatment of Branch Retinal Vein Occlusion (BRVO) and its clinical progression was presented. A 63-year-old man underwent a series of Intravitreal (IV) injections for treatment of macular edema secondary to BRVO. ERM developed after the Posterior Vitreous Detachment (PVD) during treatment with IV anti-Vascular Endothelial Growth Factor (anti-VEGF) injections. After the total of 23 Anti VEGF injections cystoid, ME, and ERM were persisted. Then subsequently, the ERM separate spontaneously from the inner retinal surface following the consecutive Intravitreal Dexamethasone implantations. Keywords: Epiretinal membrane, Posterior vitreous detachment, Branch retinal vein occlusion, Antivascular endothelial growth factor, Dexamethasone implantation.
Keywords
Epiretinal membrane, Posterior vitreous detachment, Branch retinal vein occlusion, Antivascular endothelial growth factor, Dexamethasone implantation.
Introduction
Branch retinal vein occlusion (BRVO) is one of the most common retinal diseases that can affect nearly four to five subjects per 1,000 adult populations. Macular involvement either with hemorrhage, edema, or ischemia cause decreased in visual acuity. Macular Edema (ME) is the main reason for visual impairment in BRVO. If it is not being treated in time, it may cause several complications such as macular epiretinal membrane and macular hole [1-5].
ERM is a common disease characterized by avascular, translucent fibro cellular proliferation on the retinal surface. It is classified as idiopathic and secondary ERM. Secondary ERM develops associated with other ocular pathologies such as posterior vitreous detachment (PVD), central or branch retinal vein occlusion, laser photocoagulation, retinal detachment (RD), vitreoretinal surgery, and ocular trauma [6,7].
Spontaneous separation of ERM from the macular surface is a rare occasion. This self-release generally occurs during the development of an acute PVD that simultaneously separate the attachment between the internal limiting membrane and ERM [8,9].
In the presenting article, a rare case developing ERM after PVD during the intravitreal (IV) anti-Vascular Endothelial Growth Factor (anti-VEGF) injections for ME secondary to BRVO was reported. During the treatment, the ERM spontaneously released from the inner retinal surface following the consecutive Intravitreal Dexamethasone implantations (IVD).
Case
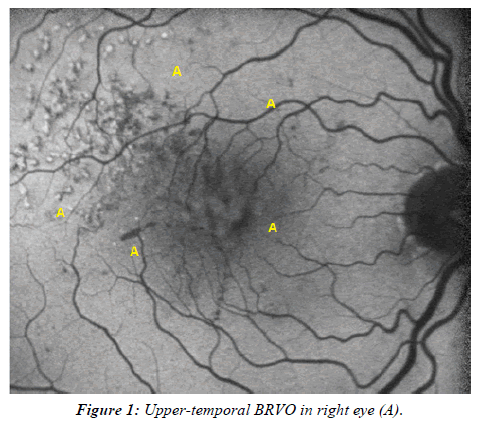
A 63-year-old man presented to the hospital with a complaint of a decrease in vision in the Right Eye (RE) for four days in October 2015. He had only a history of systemic hypertension but no history of any eye problems or ocular trauma before the presentation. On his examination, Best-Corrected Visual Acuity (BCVA) was 0.1 and 10/10 in the RE and Left Eye (LE), respectively. Intraocular Pressure (IOP) was 16 mmHg in RE and 18 mm Hg in LE. Anterior segment examination was normal with a clear lens of both eyes. The fundus examination of the RE revealed upper-temporal BRVO with intraretinal hemorrhage in the upper quadrants, and Macular edema was observed (Figure 1). LE examination was normal.
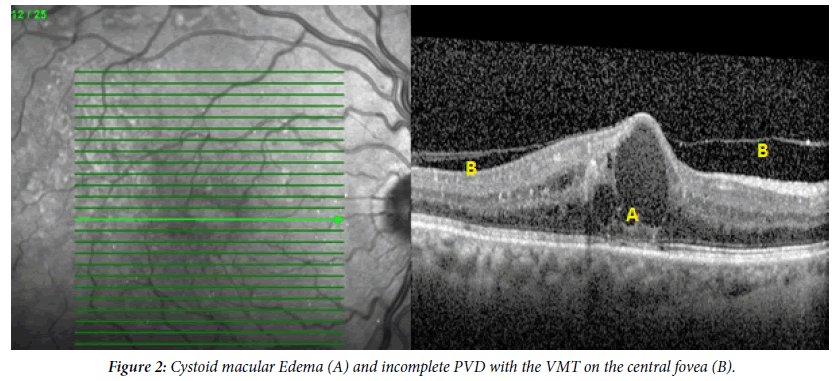
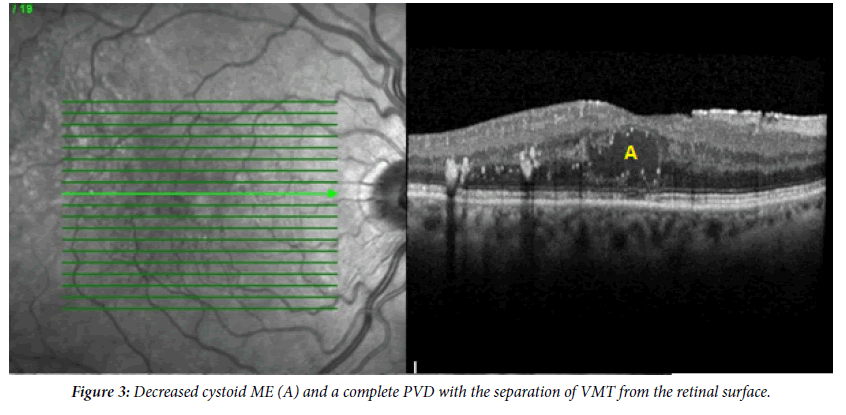
Optical coherence tomography (OCT) of RE revealed Cystoid Macular Edema (CME) and incomplete PVD with the Vitreo- Macular Traction (VMT) on the central fovea (Figure 2). Since he had a clear lens, IV Anti-VEGF treatment was preferred as a first-line treatment for ME. He underwent a series of anti-VEGF injections monthly and a regular examination with both clinically and OCT for six months. His BCVA had a minimal increment and reached to 0.2. A slight decrement of ME and persistence of VMT was observed by OCT in the same period. Anti-VEGF treatment was continued subsequent period. One and a half years after the occurrence of BRVO and regular treatment, his BCVA improved to 0.5. A moderate residual cystoid ME and complete PVD with the separation of VMT from all macular points was observed by OCT in the same period (Figure 3). Due to his satisfaction with the increment of VA, he refused to receive any more intravitreal injection, but I continued observing the patient regularly. His BCVA and OCT findings stayed stable for eight months. Then he did not continue regular examination for a few months.
Six months later, VA decreased by 0.1. His fundus examination of the affected eye revealed a semi-transparent wrinkling membrane of the inner macular surface. On OCT evaluation, re-occurrence of cystoids ME combined with diffuse ERM was observed. Due to decreased VA and increment of foveal thickness combined with the development of cystoid ME, anti- VEGF treatment started again. Even with the repeated Anti- VEGF injections, VA improvement was not achieved, and ERM remained stable throughout subsequent examinations. But he refused the surgical removal of ERM.
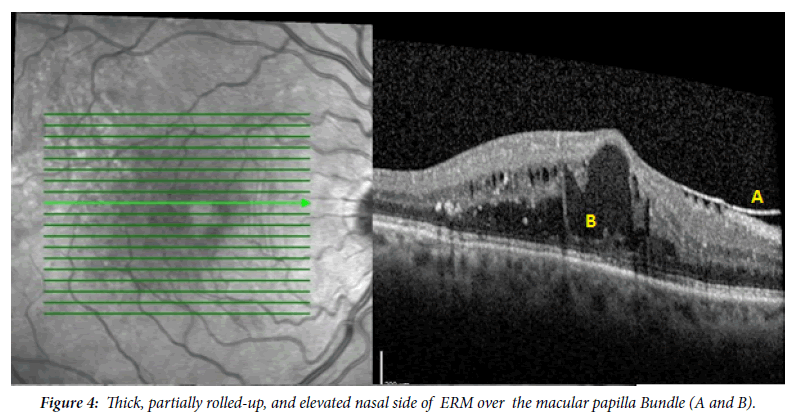
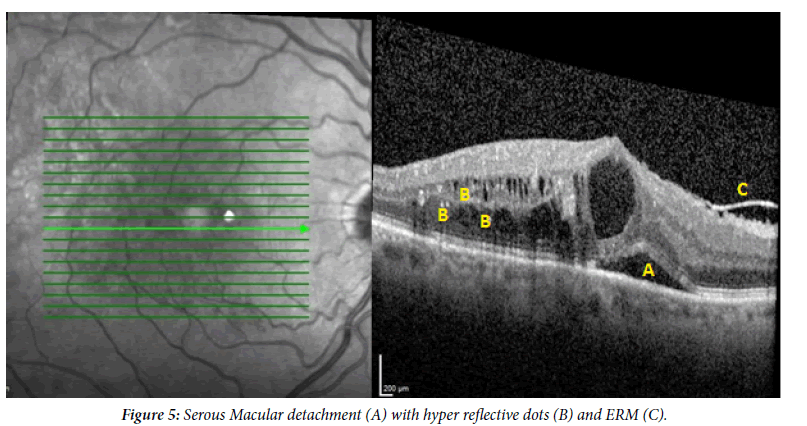
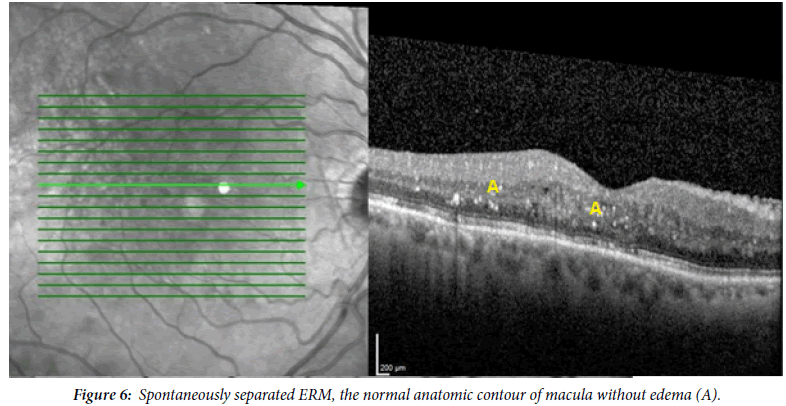
One year later, a very thick, undulating, partially rolled-up, and elevated nasal side of ERM over the macular papilla bundle was observed on OCT scans (Figure 4). Although continuous regular treatment and after the total of 23 Anti VEGF injection cystoid ME was persisted. Furthermore serous Macular detachment was developed in addition hyperreflective dots as the sign of inflammation were occurred (Figure 5). Therefore intravitreal slow-released dexamethasone (Ozurdex) implant was administered. Two months later, serous macular detachment was disappeared, and foveal thickness was decreased. But the persistence of ERM and its tangential traction has remained the same on OCT evaluation. Four months after the first IVD implantation, minimal ME reoccurred, and second IVD implantation was performed. Two months after the second IVD, his VA had improved to 0.4. The OCT revealed spontaneous separation of ERM associated with minimal retinal folds on the nasal side of the fovea, the persistence of cystoid parafoveal edema, and outer retinal changes such as interruption of the retina pigment epithelium. Two months later, the retinal folds and cystoid parafoveal edema were disappeared, foveal thickness decreased, and normalization of the anatomic contour of the macula only with few intraretinal hyperreflective dots were seen on OCT examination (Figure 6).
In the last examination ten months after the second IVD implantation, smooth retinal surface with reduced foveal thickness remain the same without any recurrence of ME but VA was unchanged in the affected eye.
Discussion
Spontaneous release of ERM from the retinal surface is a rare clinical phenomenon. This article presents a case that developed ERM during the IV AntiVEGF treatment in the eye with BRVO and subsequently separated spontaneously without any surgical intervention. ERM as a pathologic membrane grows on Internal Limiting Membrane (ILM). It may be idiopathic or proliferate in connection with other ocular diseases such as retinal vein occlusions or during the its treatment [6,7].
In Chehaibou, et al. [6] study about identifying ERM proliferation in various vitreoretinal diseases, they found six eyes with ERM had BRVO, all of them underwent treatment for ME. Five eyes had a history of Anti-VEGF therapy, 1 had dexamethasone implant, and 1 eye underwent both treatments similar to our case. Marticorena, et al. [10] examined 25 eyes with retinal vein occlusions, and ERM developed in four eyes within 6-7 weeks after IV Ani-VEGF injection. Kang, et al. [11] evaluated the incidence of ERM following IV injection for diabetic ME and found 9.5 % secondary ERM proliferation in the meantime of 19.3 ± 12.4 months. They observed that 6.5% of eyes had received Anti-VEGF while 24.0% of them had IVD implantation.
IV injections could cause alteration of vitreous structures, such as induced vitreous liquefaction and partial or complete PVD. PVD is significantly correlated with ERM development which can damage the ILM in that way, permitting the migration and proliferation of glial cells in the retinal surface. The increased number of IV injections could increase the risk of PVD development, thereby increased the ERM incidence.
PVD is associated with ERM in 80%-95% of cases [12-15]. Incomplete PVD with VMT had already been developed when BRVO first diagnosed in presenting case. IV Anti-VEGF treatment started as soon as the ME secondary to BRVO was diagnosed. ERM developed after the series of treatment with IV Anti-VEGF agents, before the IVD implantation. Therefore in the presenting case, ERM proliferation may be part of the natural course of BRVO or correlated with IV Anti-VEGF injection. VMT can resolve spontaneously as a result of complete PVD in 11%-53% of cases [16,17].
The patient’s VA improved, and foveal thickness decreased with a total resolution of the VMT during the Anti-VEGF injections. Therefore it is difficult to know, whether the complete separation of VMT occurred spontaneously or induced by the IV injection in our case. VA remained stable after PVD without treatment until the development of ERM. His VA decreased again due to the development of ME secondary to tangential traction and distraction of fovea by the ERM. ME and the deterioration of visual function persisted despite the IV Anti-VEGF injections. The contractive forces of ERM can cause ME resistance to IV treatment. Spontaneous ERM separation was developed after the two successive IVD implantation in presented case.
Self-separation of ERM occurs occasionally all eyes with and without the PVD [8,9]. Yang, et al. [18] reported 13.4% self separation of ERM occurred in eyes without pre-existing PVD while only 1.5% in eyes with pre-existing PVD. Similarly, Meyer, et al. [19] observed spontaneous release of ERM in 2.3% of eyes without pre-existing PVD compared to 0.47% in eyes with pre-existing PVD. Our patient had pre-existing PVD when spontaneous separation of ERM occurred.
Several ERM separation mechanisms had been described. The most common mechanism is associated with complete PVD that simultaneously separates ERM from the retinal surface [8,16]. Another one is increased tangential traction, that produced by contracting forces inside of ERM, when becomes stronger than the adhesions between ERM and ILM, it causes spontaneously release of attached ERM [18,19]. The last and the less frequent mechanism is rupture of the weakest part of attachment between ERM and retinal surface, mainly above blood vessels by a combination of severe elevation in intrathoracic, intracranial, and blood pressure during by lifting heavy objects [8,9,18-20].
In the presenting case with pre-existing PVD, the first common mechanisms of spontaneous self separation of ERM are excluded. In addition, our patient had no history of lifting heavy objects.
Dexamethasone implant has a very high initial injection speed, which exponentially diminishes in the vitreous due to intraocular drag force. IVD implantation may cause physically induce focal stress opponent side of the injection [11]. We prefer the superior temporal side for injection, so that IVD implantation may cause focal mechanical stress in the nasal side where the attachment of ERM on the retinal surface in this patient. Therefore IVD may initiate spontaneous separation of ERM in presenting the case.
Even though the ERM separation was correlated with VA improvement, the VA of the presenting case could not be totally restored. Long duration of ME may cause some degree of damage to retinal cells functional.
In conclusion, in this report, a rare case that developed ERM after PVD, during IV Anti-VEGF injections and subsequently separate it spontaneously following the consecutive IVD injection, for treatment of BRVO is presented. IVD implantation may cause directly or has an additional effect on the spontaneous release of ERM. To the best of my knowledge self-separation of ERM following IVD implantation was not reported previously. As far as I know self separation of ERM following IVD implantation was not reported previously.
References
- Iijima H.Mechanisms of vision loss in eyes with macular edema associated with retinal vein occlusion.Jpn J Ophthalmol. 2018;62:265-73.
- Chen G, Chen P, Chen X, et al. The laser combined with intravitreal injection of ranibizumab for the treatment of macular edema secondary to branch retinal vein occlusion. A protocol for systematic review and meta-analysis Medicine (Baltimore). 2021; 100(4):e23675.
- Coscas G, Cunha-Vaz J, Soubrane G.Macular edema: definition and basic concepts.Dev Ophthalmol.2017;58:1-9.
- Spaide RF.Retinal vascular cystoid macular edema: review and new theory.Retina.2016;36:1823-42
- Tsotridou E, Loukovitis E, Zapsalis K, et al. A Review of Last Decade Developments on Epiretinal Membrane Pathogenesis. A Med Hypothesis Discov Innov Ophthalmo. 2020 ;9(2): 91-110
- Chehaibou I, Pettenkofer M, Govetto A, et al. Identification of epiretinal proliferation in various retinal diseases and vitreoretinal interface disorders. Int J Retina Vitreo. 2020;6:31
- Stevenson W, Prospero Ponce CM, Agarwal DR, et al. Epiretinal membrane: optical coherence tomography-based diagnosis and classification.Clin ophthalmol.2016;10:527-34.
- Mentes J, Nalca S. An Unusual Case: Self-separation of an Idiopathic Epiretinal Membrane. Turk J Ophthalmol. 2020;50(1): 56-58
- Oono Y, Nakamura S, Yoshimura K, et al. Recurrence after Spontaneous Resolution of an Idiopathic Epiretinal Membrane Case Rep Ophthalmol. 2011;2(1):55-58.
- Marticorena J, Romano MR, Heimann H, et al. Intravitreal bevacizumab for retinal vein occlusion and early growth of epiretinal membrane: a possible secondary effect?The Briti journ of ophthalmol.2011;95:391-395
- Kang YK, Park HS, Park DH, et al. Incidence and treatment outcomes of secondary epiretinal membrane following intravitreal injection for diabetic macular edema. Sci Rep.2020;10:528.
- Stalmans P. A retrospective cohort study in patients with tractional diseases of the vitreomacular interface (ReCoVit)Graefe’s Archive for Clinic and Experiment Ophthalmol.2016;254(4):617-628.
- Petrou P, Chalkiadaki E, Errera MH, et al. Factors Associated with the Clinical Course of Vitreomacular Traction J Ophthalmol. 2020;2020:9457-570.
- Romano MR, Comune C, Ferrara M, et al. Retinal changes induced by epiretinal tangential forces.J Ophthalmol. 2015:1-13.
- Panjaphongse R, Stewart JM. Vitreomacular Traction after Dexamethasone Intravitreal Implant (Ozurdex) Injection: The Effect of Anomalous Posterior Vitreous Detachment.Retin cases & bri repor.2016;10:55-57.
- Altintas AGK. Spontaneous closure of Macular hole following the separation of vitreomacular traction. J Ophthalmol Adv Res. 2021;2(1): 1-7.
- Altintas AGK. . Spontaneous closure of Stage II idiopathic Macular hole. Experimen and Clinic Ophthalmol .2021;1(1): 1-6.
- Yang HS, Hong JW, Kim YJ, et al. Characteristics of spontaneous idiopathic epiretinal membrane separation in spectral-domain coherence tomography. Retina.2014;34(10):2079-87.
- Meyer CH, Rodrigues EB, Mennel S, et al. Spontaneous separation of epiretinal membrane in young subjects: personal observations and review of the literature.Graefes Arch Clin Exp Ophthalmol.2004;242(12):977-85.
- Mansour A M, Mansour HA, Arevalo JF. Spontaneous release of epiretinal membrane in a young weight-lifting athlete by presumed central rupture and centrifugal pull. Clin Ophthalmol. 2014;8:2243-52.