Case Report - Journal of Gastroenterology and Digestive Diseases (2018) Volume 3, Issue 3
Retroflexion in the proximal colon in the evaluation and resection of large nonpedunculated polyps.
Goncalo Alexandrino*, Luís C. Lourenco, Rita Carvalho and Jorge Reis
Department of Gastroenterology, Hospital Prof. Doutor Fernando Fonseca, Hospital in Amadora, Portugal
- *Corresponding Author:
- Goncalo Alexandrino
Department of Gastroenterology
Hospital Prof. Doutor Fernando Fonseca
Hospital in Amadora, Portugal
Tel: +351 966199616
E-mail: goncaloalexandrino@gmail.com
Accepted on Juy 13, 2018
Citation: Alexandrino G, Lourenco LC, Carvalho R, et al. Retroflexion in the proximal colon in the evaluation and resection of large nonpedunculated polyps. J Gastroenterol Dig Dis. 2018;3(3):47-48.
Abstract
We present the case of a piecemeal endoscopic mucosal resection of a 40 mm flat lesion of the proximal ascending colon. On the follow-up colonoscopy there was residual lesion which seemed to be not totally visible in direct vision. Retroflexion of the colonoscope was crucial to better characterize the lesion and perform submucosal injection, thus making endoscopic mucosal resection in direct vision effective. Retroflexion in colonoscopy is commonly used for rectal lesions. However, as shown in this case, it can be a very useful technique in the proximal colon to detect lesions that otherwise would not be visible or resect lesions that are difficult to access in the forward view. In conclusion, retroflexion in the proximal colon is simple to perform, safe and can be very useful in the evaluation and resection of lesions with difficult approach in direct vision.
Keywords
Colon, Colorectal polyps, Endoscopy.
Introduction
Retroflexion in colonoscopy is used more frequently to evaluate or resect lesions in the distal rectum that are difficult to assess in direct vision. However, this maneuver can be very usefull also in the proximal colon. Observation of the proximal colon in retroflexion may detect lesions that otherwise are not visible [1,2]. Another advantage of this maneuver is the possibility of removing lesions that are difficult to access in the forward view.
Case Presentation
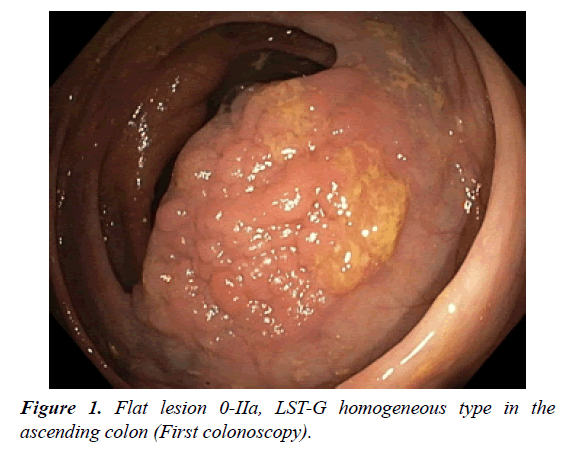
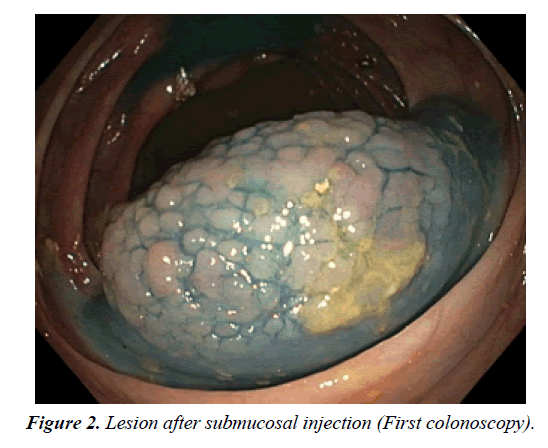
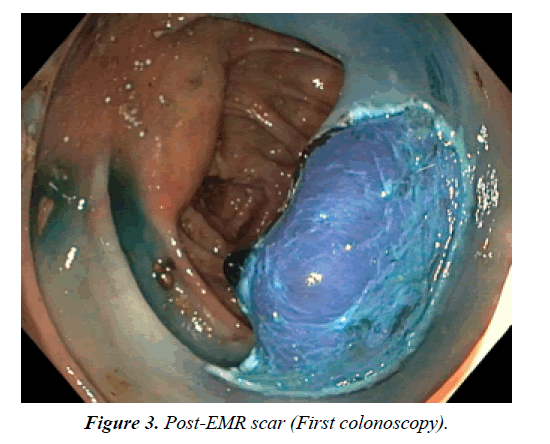
A 65-year-old male patient was referred to our institution for resection of a polyp in the ascending colon detected at a screening colonoscopy. The lesion was located in the proximal ascending colon, immediately above the ileocecal valve, in the contralateral fold. It was a flat lesion 0-IIa (Paris classification), laterally spreading tumor granular (LST-G) homogeneous type, with about 40 mm of biggest diameter, occupying more than one third of the luminal circumference (Figure 1). After submucosal injection with saline, adrenaline and methylene blue, piecemeal Endoscopic Mucosal Resection (EMR) was performed (Figures 2 and 3). The procedure was performed with the Olympus® 190-series colonoscope. No complications occurred. The histological analysis revealed a tubulo-villous adenoma with foci of high-grade dysplasia.
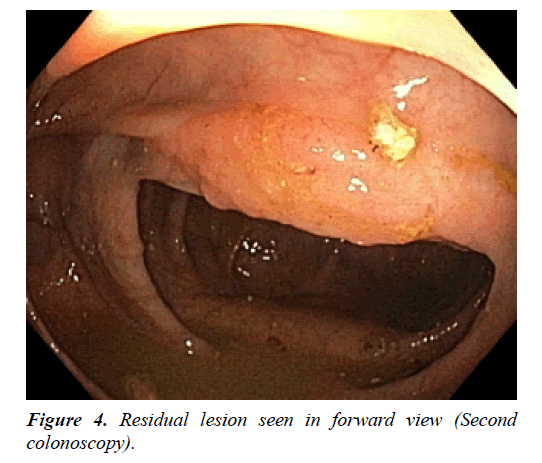
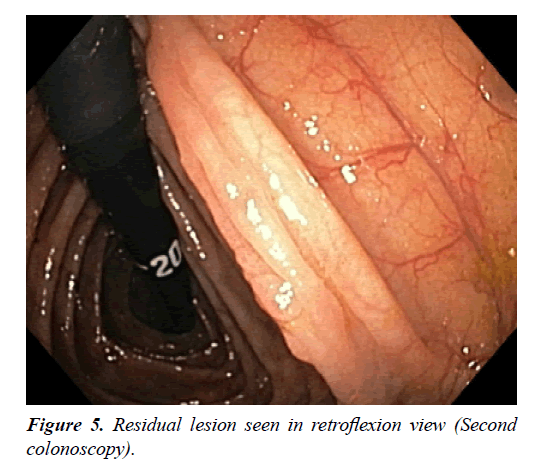
Three months later, the follow-up colonoscopy showed residual lesion (Figure 4). Since the lesion appeared to involve the proximal aspect of the fold that was not visible in direct vision, we decided to perform retroflexion, in order to better characterize the lesion (Figure 5). This time, submucosal injection was performed in retroflexed view so that the lesion could be approached in forward view for resection. There was no significant fibrosis and it was possible to manage the residual lesion endoscopically, with en bloc EMR. There were no complications and three months later there was no residual tissue.
Discussion and Conclusion
Retroflexion in the proximal colon is a useful technique for the detection, evaluation and resection of non-pedunculated polyps. Regarding the resection demonstrated in this case, it can be very important to first lift the proximal edge of the polyp while in retroflexed position. This allows for the entire polyp to become more visible in a forward view and facilitate the snaring and resection. Retroflexion can be used only to perform submucosal injection at the distal end of the lesion, like in our case, but in certain circumstances resection may be facilitated if performed in inversion. Moreover, it seems a safe technique, with only one adverse event described in the literature [3]. In conclusion, retroflexion in the proximal colon is simple to perform, safe and can be very useful in the evaluation and resection of lesions with difficult approach in direct vision.
References
- Pishvaian AC, Al-Kawas FH. Retroflexion in the colon: A useful and safe technique in the evaluation and resection of sessile polyps during colonoscopy. Am J Gastroenterol. 2006;101:1479–83
- Hewett DG, Rex DK. Miss rate of right-sided colon examination during colonoscopy defined by retroflexion: an observational study. Gastrointest Endosc. 2011;74(2):246-52.
- Geng Z, Agrawal D, Singal AG, et al. Contained colonic perforation due to cecal retroflexion. World J Gastroenterol. 2016;21; 22(11): 3285-88.