Case Report - Annals of Cardiovascular and Thoracic Surgery (2025) Volume 8, Issue 1
Reconstruction of the aortic root with preservation of the aortic valve (case from practice).
IH Bebezov1,2, MK Djundubaev1,2, AA Rakimbaev1, DB Toktosunova1,2, RS Kalieva1, AK Turgunov1,2*
1 Department of Cardiology, Scientific Research Institute of Heart Surgery and Organ Transplantation, Bishkek 720040, Kyrgyzstan
2 Department of Medicine, International Higher School of Medicine, Bishkek 720054, Kyrgyzstan
*Corresponding Author:
- AK Turgunov
Department of Cardiology, Scientific Research Institute of Heart Surgery and Organ Transplantation, Bishkek 720040, Kyrgyzstan
E-mail: azaturgunov@gmail.com
Received: 28-Aug-2023, Manuscript No. AAACTS-23-113374; Editor assigned: 30-Aug-2023, AAACTS-23-113374 (PQ); Reviewed: 13-Sept-2023, QC No. AAACTS-23-113374; Revised: 20-Jan-2025, Manuscript No. AAACTS-23-113374 (R); Published: 27-Jan-2025, DOI: 10.35841/aaacts.8.1.161
Citation: Bebezov IH, Djundubaev MK, Rakimbaev AA, et al. Reconstruction of the aortic root with preservation of the aortic valve (case from practice). Ann Cardiothorac Surg 2025;8(1):1-4.
Keywords
Ascending aortic aneurysm, Aortic root reconstruction, Echocardiography, MDCT.
Introduction
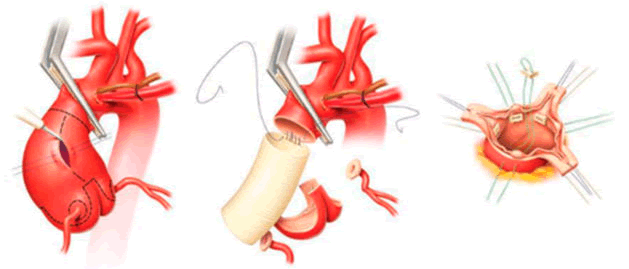
In 1992, T. David proposed to perform prosthetics of the ascending aorta, valsalva sinuses and implantation of the mouths of the coronary arteries into a vascular prosthesis in case of aneurysm of the aortic root and intact Aortic Valve flaps (AV), and isolates the aortic valve flaps together with the commissures and re-implant inside the vascular prosthesis [1]. Preservation of the native aortic valve makes it possible to save the patient from potential prosthesis-associated complications, such as Thrombosis, endocarditis, structural and non-structural dysfunction of the prosthesis, etc. (Figure 1) [2,3].
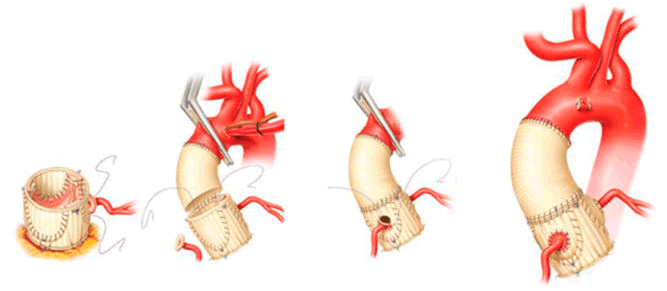
Valve preserving technologies in aortic root surgery are a worthy alternative to AV prosthetics in the treatment of aortic root pathology with or without aortic insufficiency. The development and improvement of methods of re-implantation and remodeling of the aortic root, as well as the absence of potential prosthesis-associated complications in the long-term postoperative period have ensured the continued popularity of valve-preserving methods in aortic root surgery (Figure 2) [4].
Case Presentation
The aim of the work is to present a clinical case of successfully performed surgical treatment of sinus Valsalva aneurysm and ascending aorta using the David technique.
Patient K.M., born in 1981, entered the research institute of heart surgery and organ transplantation with complaints of pressing pains behind the sternum at rest, increasing with little physical exertion. According to the patient, he noted an increase in blood pressure for 1 year, the maximum figures reached 150/100 mmHg, accompanied by chest pains. During the examination for ECHOCG, signs of expansion of the ascending aorta were revealed. Subsequently, Multi-Detector Computed Tomography (MDCT) of the mediastinal organs was performed to clarify the diagnosis, where the expansion of the Valsalva sinus to 50 mm, the ascending part of the aorta to 45 mm was revealed. Hospitalized for surgical treatment [5].
Examinations before surgery
Electrocardiogram: Sinus rhythm, heart rate 62 beats per minute. The horizontal position of the EOS. Violation of the processes of repolarization of the walls of the left ventricle.
Echocardiography
• Aorta: Compacted, the diameter of the ascending part is 33 mm, at the root of the aorta is 46 mm, at the sinus of the Valsalva is 48 mm, the descending aorta is not changed.
• Aortic valve: tricuspid, with marginal seal. The degree of regurgitation is minimal, AVmaxPG is 11 mmHg.st;
• Mitral valve: In the opposite phase, with an edge seal. The degree of regurgitation is 1(+), MVmaxPG is 5 mmHg.st;
• Tricuspid valve: In antiphase [6]. The degree of regurgitation is 1(+), TVmaxPG is 3 mmHg.st;
• Pulmonary artery: Not dilated,
• Pulmonary artery valve: Not changed, regurgitationminimal. The pressure gradient is 6 mmHg.
• Left atrium: 32 mm.
• The right atrium is not dilated.
• Left ventricle: Diastolic size-56 mm; Systolic size-37 mm; Ejection fraction-63%; (according to Teigolz); hypokinesis zones: Diffuse hypokinesis of LV walls. LV diastolic function: E/A-0.8 are impaired,
• Right ventricle: 24 mm, anterior wall of the right ventricle-4 mm. TARSE-mm.
• Pericardium: The systole is not changed. Pulmonary arterial pressure 35 mmHg.
• Atrial septum: Intact.
• Interventricular septum: Intact.
• Additional features: None.
Multi-detector computed tomography: In the arterial phase of the study, there is a uniform filling of the aorta and branches with a contrast agent. There were no signs of dissection in the entire area of the examined aorta. No pathological changes were detected in the projection of the coronary arteries. The walls of the aorta are not compacted. Without calcification. There is an aneurysmal expansion of the ascending aorta, starting from the sinuses of the Valsalva, for 55 mm (Figure 3). The transition of the aneurysm to the aortic arch and brachiocephalic vessels was not revealed. The heart is usually located. Dimensions of the heart chambers: Left atrium 3.6 cm × 5.7 cm. The transverse size of the left ventricle is 0.9 cm [7].
Chest X-ray: The pulmonary fields are transparent; the pulmonary pattern is reinforced, deformed in a cellular type due to the peribronchial component. The roots of the lungs are poorly structured. Pleural sinuses are free. A heart shadow with a smoothed waist. The aorta is dilated in the ascending part.
Coronary angiography: Coronary arteries without hemodynamically significant lesions.
Discussion
The patient underwent preoperative preparation, on 23.01.2020; an operation was performed as planned-operation David in conditions of moderate hypothermic artificial circulation (32C), blood cold cardioplegia.
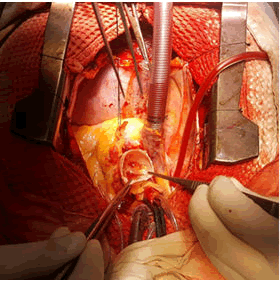
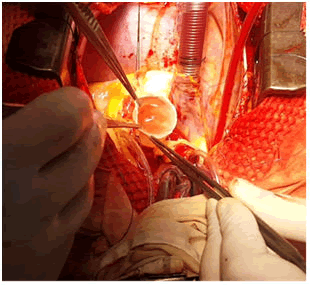
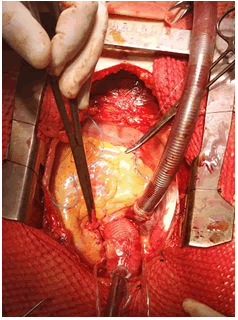
Intraoperatively: The ascending aorta, starting from the root, the sinus of the valsalva is expanded to 5.5-5.8 cm, tense, thinned, closer to the arc diameter of about 3.0 cm. The heart is enlarged in size due to the left ventricle. Pouch seams, heparin. The ascending aorta is isolated, taken on a ribbon. Cannulation of the vox. The aorta is closer to the arch and the RA is a twostage cannula, artificial blood circulation has been started. Smooth cooling of the patient. The aortic root was isolated; the upper right pulmonary vein was drained for LV decompression. The aorta was clamped, the aortic wall was opened longitudinally, blood cold cardioplegia at the mouth of the left and right coronary arteries, cardiac arrest. Revision of the aorta and AV: The aortic wall is thinned, atherosclerotically altered. The aortic valve is tricuspid, the fibrous ring is moderately expanded, the valve flaps are not changed, and there is no soldering. The mouths of the L?A and RCA at the sites are highlighted. Excised aneurysmal sac of the sinus of Valsalva. The ring freely passes the 25 calibrator. Implantation of a proximal anastomosis according to the David method. Hydraulic test- the coaptation of the AV is complete, there is no regurgitation, the valve opening is sufficient. Reimplantation of the mouths of the coronary arteries at the sites into a vascular prosthesis.
The distal anastomosis is applied end-to-end with a continuous suture. Smooth warming of the patient. Prevention of air embolism. The aorta was released, cardiac activity was restored through the AV block, the myocardial electrode was sewn to the pancreas, and the rhythm from the pacemaker was imposed. Stabilization of hemodynamics, smooth departure from IR.
Control hemostasis, its own rhythm, pacemaker is disabled. Decanulation of vessels, protamine sulfate. Protamine sulfate. Drains into the pericardial cavity and anterior mediastinum. Stitches on the pericardium. Polispastnye seams. Layered suturing of the wound. Postoperative data of ECHO?G at the time of discharge: Aorta-conduit-24 mm. Aortic valve-three flaps, minimal regurgitation, from the commissary-right coronary flap/not a coronary sash. The left atrium is 33 mm; the right ventricle is 23 mm. The left ventricle is 53 × 32 mm; the ejection fraction is 70%. Mitral valve and tricuspid valve: Regurgitation is minimal. Systolic PAP-30 mmHg. Pericardium, pleural cavities-not changed (Figures 4-6).
Conclusion
The generally accepted method of treating aneurysms of the ascending aorta is the operation of total replacement of the aortic root and the ascending department with a valvecontaining conduit (Bentall-deBono operation). However, such interventions are not without drawbacks associated with the use of an artificial heart valve: There is still a need for anticoagulant therapy; there is a risk of thromboembolic complications, infectious endocarditis.
Prosthetics of the ascending aorta with reimplantation of AV (David operation) is an effective and safe method of surgical treatment of an aneurysm of the ascending aorta, combined with an aortic insufficiency and unchanged AV valves. When using Valsalva aortic prostheses, there were no significant advantages compared to linear prostheses. Relapses of aortic insufficiency in the long-term period, requiring repeated intervention, are most often associated with technical errors during the initial operation.
References
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. JAMA. 2000;283(7):897-903.
[Crossref] [Google Scholar] [PubMed]
- Meszaros I, Morocz J, Szlavi J, et al. Epidemiology and clinicopathology of aortic dissection. Chest. 2000;117(5):1271-8.
[Crossref] [Google Scholar] [PubMed]
- Saczkowski R, Malas T, de Kerchove L, et al. Systematic review of aortic valve preservation and repair. Ann Cardiothorac Surg. 2013;2(1):3.
[Crossref] [Google Scholar] [PubMed]
- David TE, Feindel CM, Webb GD, et al. Aortic valve preservation in patients with aortic root aneurysm: Results of the reimplantation technique. Ann Thorac Surg. 2007;83(2):S732-5.
[Crossref] [Google Scholar] [PubMed]
- David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg. 1992;103(4):617-22.
[Google Scholar] [PubMed]
- Aicher D, Fries R, Rodionycheva S, et al. Aortic valve repair leads to a low incidence of valve-related complications. Eur J Cardiothorac Surg. 2010;37(1):127-32.
[Crossref] [Google Scholar] [PubMed]
- Hanna MF, Malguria N, Saboo SS, et al. Cross-sectional imaging of sinus of Valsalva aneurysms: Lessons learned. Diagn Interv Radiol. 2017;23(5):339.
[Crossref] [Google Scholar] [PubMed]