Research Article - Journal of Public Health Policy and Planning (2021) Volume 5, Issue 6
Preterm birth and associated factors among mother who gave birth in public health hospitals in harar town eastern Ethiopia.
Gosaye Tekelehaymanot*
Department ofMidwifery, Harar Health Science College, Harar, Ethiopia
- Corresponding Author:
- Dr. Gosaye Tekelehaymanot
Department of Midwifery
Harar Health Science College Harar
Ethiopia
E-mail: gosayeteklehaymanot33@gmail.com
Accepted date: 16 May, 2021
Citation: Tekelehaymanot G. Preterm birth and associated factors among mother who gave birth in public health hospitals in harar towneasternEthiopia. J Public Health Policy Plann. 2021;5(6):1-6.
Abstract
Background: Preterm birth is defined as a delivery which occurs at less than 37 weeks completed of gestation. The majority of preterm birth remains vulnerable to long term complications that may persist all over their lives. Globally, about 12.9 million births (9.6%) of all births worldwide were preterm and of these more than 60% of preterm births occur in Africa and South Asia while about 0.5 million were in each of Europe and North America. There is limited evidence on magnitude of preterm birth and associated factors, among women attending delivery service at public hospitals of low income countries like Ethiopia including the study setting, Harar town.
Keywords
Laboring mother, Pretermbirth, Public hospital, Harar town.
Introduction
Preterm birth is defined by WHO as all viable births before 37 completed weeks of gestation or fewer than 259 days since the first day of woman’s last menstrual period. It is classified as extremely preterm <28 weeks, very preterm 28 to <32 weeks, and moderate preterm 32 to <37 weeks can also be spontaneous or provider initiated (induced).
Globally, about 12.9 million births (9.6%) of all births worldwide were preterm and of these more than 60% of preterm births occur in Africa and South Asia while about 0.5 million were in each of Europe and North America and 0.9 million in Latin America and the Caribbean.
The rate of preterm birth is escalating globally and ranges from 5 to 7% in developed countries and significantly higher in least developed countries. Prematurity is one of the leading causes of neonatal deaths in Africa (11.9%) and is a major public health problem and it is responsible for 27% of all early neonatal admission [1]. According to the report from “white paper on preterm birth” in 2011, of all 4 million annual early neonatal deaths 28% are due to preterm birth. Preterm birth has many long and short term consequences like cerebral palsy, mental retardation, visual and hearing impairments, behavior and social-emotional concerns, learning difficulties, and poor health and growth, neurosensory deficits (blindness, deafness), intra ventricular hemorrhage, necrotizing enter colitis, and delay in physical and mental development. The major risk factor of preterm delivery was absence or inadequate prenatal care, low monthly income, no contraceptive use, cesarean delivery, and clinical complications during pregnancy. There is limited information on magnitude of preterm birth and associated factor among women attending delivery service at public hospitals of Harar Town therefore this study aimed to contribute in identifying magnitude and factors associated with preterm birth.
Significance of the study
The result of this study provides valuable information on magnitude of preterm birth and associated factors. Determining factors has a great role in guiding health professionals and health policy makers to design the intervention strategy and applying necessary preventive and appropriate measures to decrease preterm birth and new born mortality and morbidity. In addition, it will help to fill the research gaps in the study area and serve as base line information for other researcher [2].
Methods and Materials
Study area and period
Institutional based cross sectional study was conducted among mother who gave birth in Harar Town public health institution. Harar is located in the eastern part of Ethiopia 525 Km away from Addis Ababa, the capital city of Ethiopia. In the region, 27 health posts, 8 health centers and 2 Public, 2 Private, 1 Federal Police, 1 Fistula Hospitals, 18 Private for profit clinics, 25 pharmaceutical retails out let, 3 pharmaceutical whole sellers and 2 modern laboratories are available. The study was conducted in 2 public hospital specialized university hospital [3].
Study design
Quantitative Institutional based cross sectional study was utilized.
Source and study population
The source of population was mothers who gave birth in Harar town public hospitals and the study population were randomly selected mother who gave birth during the study period.
Inclusion and exclusion criteria
Women who gave births during the study period with known LNMP or had ultrasound check up result during pregnancy were include on this study while. A woman who doesn’t have consent, Women who are unable to communicate was excluded [4].
Sample size determination
Sample size was determined by using single population proportion formula (Proportion of preterm birth from study conducted were 25.9% Calculated sample size=295 by adding 10% non-response rate the final Sample was =325 and double population proportion formula (P1=23.46% and P2=9.64%, 95%, margin of error of 5% and power of 80%, and using Open Epi Info) Calculated sample size =254 by adding 10% non-response rate the final Sample was =279 then comparing the first and second objective, the final sample size was 325.
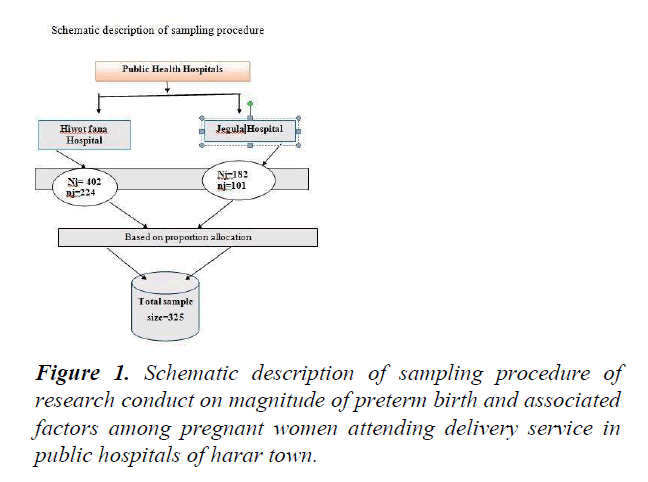
Sampling procedure
Two governmental public hospital were include sample was proportionally allocated based on their patient flow. Average monthly patient flows in two hospitals were 402 and 180 at HFSUH and Jegula Hospital [5]. Sampling frame was developed from delivery registration book and subjects were selected by using systematic random sampling method. Finally a total of 325 participants were selected based on their allocation until desired sample size was meet.
Variables of the Study
Data collection tools and procedure
The interviewer administered questionnaire was adopted after reviewing relevant scientific literatures. The tool were translated into local language Afan Oromo and translated back to English language to check its consistency, questionnaire contains socio demographic, obstetrics, health care service utilization and medical related factors. Data were collected by three diplomas and one BSc Midwives.
Data quality control
To assure the quality of the data, properly design data collection instrument was developed and pretest was conducted. Training was given for data collectors and supervisors for three days on the instruments, method of data collection, ethical issues and purpose of the study. Completeness and correctness of data was checked on daily based [6].
Data processing and analysis
Data entry was done by using Epi-info 3.1 and transferred to SPSS version 21 for analysis. The univariate analysis such as proportions, percentages frequency distributions and appropriate graphic presentations as well as measures of central tendency and measures of dispersion were made. Inferential statistics were used to establish associations between prematurity and the various risk factors using a chi- square analysis [7]. Multivariate logistic regression was used to determine the factors independently associated with preterm birth. In binary logistic regression analysis with p ≤ 0.25 were transferred to multivariate logistic regression analysis. In multivariable logistic regression analysis, the variables with P- value ≤ 0.05 were considered as significantly associated variable with preterm birth.
Ethical clearance
Ethical clearance letter was obtained from Harar health Science College Ethical Review Committee. Permission was obtained from study institution. All the participants were informed the purpose, advantages and disadvantages, there have the right to be involved or not. Consent was obtained from each respondent prior to data collection; Confidentiality was maintained by avoiding names and other personal identification [8].
Results
Socio-demographic characteristics
A total of 325 mothers were included on the study which makes the response rate 100%. The mean age of the study participants was 27.02 with ± 5.73 SD. Majority, 200(61.5%) of the study participants were between 20 and 30 years old. Regarding ethnicity majority 161(49.5%) of the respondent are Oromo 158(48.6%) and Muslim religion flowers (Table 1).
Table 1. Socio-demographic characteristics of women who give birth in public hospitals in harar town, eastern Ethiopia.
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Age | < 20years | 19 | 5.8 |
| 21-30 years | 200 | 61.5 | |
| 31- 40 years | 106 | 32.7 | |
| Residency | Urban | 146 | 44.9 |
| Rural | 179 | 55.1 | |
| Religion | Muslim | 158 | 48.6 |
| Orthodox | 107 | 32.6 | |
| Protestant | 60 | 18.5 | |
| Ethnicity | Oromo | 161 | 49.5 |
| Amhara | 106 | 32.6 | |
| Harari | 35 | 10.8 | |
| Tigray | 15 | 4.6 | |
| Somali | 8 | 2.5 | |
| Education of mother | Can’t read and write | 101 | 31.7 |
| Can read and write | 110 | 33.8 | |
| Primary level | 90 | 27.7 | |
| Secondary and above | 25 | 0.8 | |
| Occupation of mother | Government | 128 | 39.4 |
| Private | 115 | 35.4 | |
| Merchant | 82 | 25.2 |
Obstetric related characteristics
Majority of the respondent 227(69.8%) were multigravida women. Regarding birth interval 164(72.2%) women had less than two years birth interval. Spontaneous vaginal delivery accounts the highest 240(73.8%) mode of delivery. Nearly one third 99(30.5%) of women had history of abortion. while more than half 180(55.4%) of the pregnancy were planned. Majority women 282(86.8%) labour had start spontaneously and they had no 250(76.9%) history of Liquid drainage before labor.
Table 2. Obstetrics related characteristics of women who give birth in public hospitals in harar town, eastern Ethiopia.
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Ever give birth | Yes | 227 | 69.8 |
| No | 98 | 30.2 | |
| Inter birth interval | ≤ 2 years | 164 | 72.2 |
| 3-5 years | 56 | 24.7 | |
| > 5 years | 7 | 3.1 | |
| Current mode of delivery | SVD | 240 | 73.8 |
| C/S | 70 | 21.5 | |
| Instrumental | 15 | 4.7 | |
| Pregnancy outcome | Single tone | 243 | 74.8 |
| Multiple | 82 | 25.2 | |
| History of preterm | Yes | 85 | 26.8 |
| No | 240 | 73.8 | |
| History of abortion | Yes | 99 | 30.5 |
| No | 226 | 69.5 | |
| Pregnancy type | Planned | 180 | 55.4 |
| Unplanned | 145 | 44.6 | |
| Labor onset | Spontaneous | 282 | 86.8 |
| Induced | 43 | 13.2 | |
| Liquid drainage before labor | Yes | 75 | 23.1 |
| No | 250 | 76.9 | |
| History of PIH | Yes | 75 | 23.1 |
| No | 250 | 76.9 | |
| History of APH | Yes | 84 | 25.4 |
| No | 241 | 74.2 | |
| Any injury during current pregnancy | Yes | 50 | 15.4 |
| No | 275 | 84.6 |
Health care service related characteristics
Out of 325 mothers, 240(73.8%) had ANC follow up for their recent pregnancy whereas about 85(26.2%) of them had no ANC follow up. Among those mothers who had ANC follow 22(6.8%) of them had at least one visit while 180(55.4%) had 2 times visited and 38(11.7%) of women had having ANC Visit 3 and above.
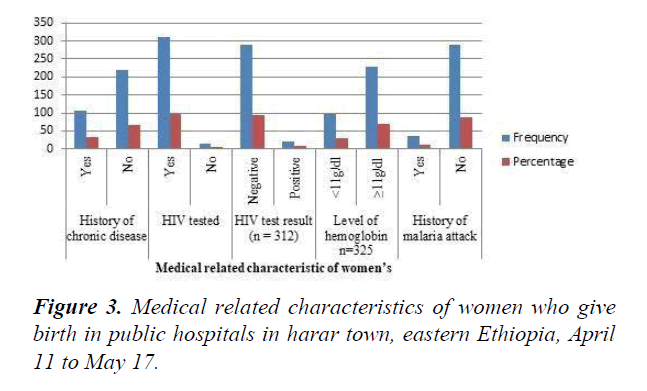
Medical related characteristic of women’s
Among 325 women tested for Anemia one third 98(30.2%) was anemic whose Hgb concentration was below 11 g/dl. Majority 312(96.4%) of the participant had tested for HIV among those tested 22(7%) had Positive result while the rest 290(93%) had Negative.
Factors associated with preterm birth
In multivariable logistic regression analysis: women who do not attending ANC follow up, maternal, hemoglobin level, history of chronic disease and History of APH were statistically significant Women who didn’t attend ANC were
1.5 times (AOR=1.5, 95% CI: 0.7, 2.3), those who had history of ante partum hemorrhage were 1.3 times (AOR=1.3, 95% CI: 0.2, 2.7) and women whose hemoglobin were less than eleven were 1.4 times (AOR=1.4, 95% CI: 0.2, 2.2) more likely to give preterm birth than counters (Table 3).
Table 3. Factors associated with preterm births among mothers who gave birth in harar town public hospitals, Eastern Ethiopia, April 11 to May 17.
| Variable | Preterm birth | COR (95% CI) | AOR (95% CI) | |
| Yes | No | |||
| Residence | ||||
| Urban | 34(23.3%) | 112(76.7%) | 1 | 1 |
| Rural | 47(26.3%) | 132(73.7%) | 1.17(0.7,1.94 )* |
1.2(0.3,1.6) |
| History of preterm | ||||
| Yes | 36(42.4%) | 49(57.6%) | 3.1(1.8,5.3)* | 2.6(1.3,5.2) |
| No | 45(18.8%) | 195(81.2%) | 1 | 1 |
| Pregnancy type | ||||
| Planned | 42(23.3%) | 138(76.7%) | 1 | 1 |
| Unplanned | 39(16.9%) | 106(73.1%) | 1.2(0.7,2.0)* | 1.6(0.4,2.5) |
| Do you attend ANC | ||||
| Yes | 60(25%) | 180(75%) | 1 | 1 |
| No | 21(24.7%) | 64(75.3%) | 1.3(0.5,1.8)* | 1.5(0.7,2.3)* |
| Inter birth interval | ||||
| <24 Months | 55(24.3%) | 171(75.7%) | 1.2(0.6,1.90)* | 1.3(0.4,2.0)* |
| ≥ 24 Months | 26(26.3%) | 121(73.7%) | 1 | 1 |
| History of Abortion | ||||
| Yes | 29(29.3%) | 70(70.7%) | 0.72(0.42,1.2 2)* |
0.5(0.2,1.2) |
| No | 52(23%) | 174(77%) | 1 | 1 |
| History of APH | ||||
| Yes | 56(66.7%) | 28(33.3%) | 1.5(0.8,2.3)* | 1.3(0.4,2.7)* |
| No | 25(10.4%) | 216(89.6%) | 1 | 1 |
| History of PIH | ||||
| Yes | 20(26.7%) | 55(73.3%) | 0.8(0.5,1.6)* | 0.7(0.3,1.2) |
| No | 61(24.4%) | 189(75.6%) | 1 | 1 |
| Onset of labor | ||||
| Spontaneous | 69(24.5%) | 213(75.5%) | 1 | 1 |
| Induced | 12(27.9%) | 31(72.1%) | 1.2(0.5,2.45)* | 1.3(0.3,2.8) |
| Hemoglobin level | ||||
| <11g/dl | 26(26.5%) | 72(73.5%) | 1.1(0.6,1.94)* | 1.4(0.3,2.2)** |
| ≥11 g/dl | 55(24.2%) | 172(75.8%) | 1 | 1 |
| Hx of chronic disease | ||||
| Yes | 27(25.7%) | 78(74.3%) | 1.9(0.6,2.4)* | 1.3(0.4,2.3)** |
| No | 54(24.5%) | 166(75.5%) | 1 | 1 |
| Hx of malaria attack | ||||
| Yes | 9(25%) | 27(27%) | 0.9(0.4,2.2)* | 1.2(0.7,2.2) |
| No | 72(24.9%) | 217(75.1%) | 1 | 1 |
Discussion
The prevalence of preterm births in this study was found to be 24.9%(95% CI 21.0, 29.8).These finding is consistent with study conducted in Brazil 21.7%, Nigeria 24%, 25.9%. The finding on this study was higher than the cross sectional study conducted in India 15%. Kenya 18.6%. Gondar town 4.4%,
Debremarkos 11.6%, 11.7% and 13.3%. This discrepancy might be due to difference in, sample size, study area, sample size, study population and intervention done toward pregnant mother as well as socio demographic characteristics [9].
Mothers who had history of Ante partum during current pregnancy were 1.3 times more likely to have preterm birth compared to counterpart. These are consistent with study conducted. These might be due consequence of anemia following bleeding predispose to hypoxia and preterm to the new womb [10].
In these study mothers who had no ANC follow up were 1.5 times more likely to deliver preterm birth than counterpart. These in lined with study conducted. The association might be due to Antenatal visits of the pregnant mothers are very important as they provide chances for monitoring the fetal wellbeing and allow timely intervention for feto-maternal protection. This may be described to the routine provisions of nutritional and medical advice or care and supplementations offered during ANC visits.
Mothers who had inter birth interval at less than 24 months were 1.3 times more likely to have preterm births compared to mothers who had inter pregnancy interval greater than or equals to 24 months. These is similar with study done [11]. These might be due to existence of unidentified risk factors which precipitating preterm births in mothers with short inter pregnancy interval as well as it may be maternal related problems such as in ability to take care for close birth interval which might be due to socio economic status.
Women who had history of chronic disease were 1.3 times more likely to deliver preterm birth than counterparts. These in lined with study conducted. These might be due to maternal chronic illnesses may alter or limit the placental delivery of oxygen and nutrients to the developing fetus, possibly resulting in fetal growth restriction. In addition, they can increase the risk of preeclampsia and, thus increases the risk preterm birth. Therefore, acute maternal medical conditions might lead to preterm birth [12].
Finally women whose hemoglobin level is less than 11 g/dl were 1.4 times more likely to deliver preterm birth than counter parts. These in lined with study conducted. These might be due to fact effect of anemia on the oxygen bearing capacity and its transportation tendency to the placental site for the fetus.
Conclusion
The prevalence of preterm birth in Harar town public health hospitals is slightly higher than studies done in different parts of Ethiopia and still a major public health problem in the area. Not attending ANC, short inter pregnancy interval (<24 months), previous history of APH, Presence of chronic medical illness and low hemoglobin level (<11 g/dl) were found to be statistically significant with the occurrence of preterm birth in current pregnancy.
Recommendation
• Timely recognition of factor predisposes to ante partum hemorrhage and managing it promptly.
• Encourage mother to have Antenatal follow up and strengthening Antenatal care service.
• Encourage contraceptive usage and birth intervals.
• Health promotion and diseases prevention strategy should be strengthened.
• Iron provision for pregnant women should be strengthened.
• Identification and timely referral for specialized obstetrical evaluation and management of these who have high risk of preterm birth mothers in early pregnancy.
References
- Lumley J. Defining the problem: the epidemiology of preterm birth. BJOG Int J Obstet Gynaecol. 2003;110:3–7.
- Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31-8.
- Seyom E, Abera M, Tesfaye M, et al. Maternal and fetal outcome of pregnancy related hypertension in Mettu Karl referral hospital. Journal of Ovarian Research. 2015;4:10.
- Blencowe H, CousensS, Oestergaard M, et al. The global epidemiology of 15 million preterm births. Reprod Health. 2013;10:1–14.
- Guerra MC, de Moraes Barros AL, Goulart LV, et al. “Premature infants with birth weights of g exhibit considerable delays in several developmental areas,” Acta Pediatrics. 2014;103:1-6.
- Blencowe H, Cousens S, Oestergaard, et al. ” National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2013;379:2162–72.
- Passini RJR, Cecatti JG, Lajos GJ, et al. Brazilian Multicenter Study on Preterm Birth: Prevalence and Factors Associated with Spontaneous Preterm Birth. PLoS ONE. 2014;9:1-12.
- Chiabi N, Mboudou E, Tchokoteu P, et al. Risk Factors for Premature Births: A Cross-Sectional Analysis of Hospital Records in a Cameroonian Health Facility. African J Reprod Heal. 2016;17:77-83.
- Halimi ASLA, Safari S, Hamrah M, et al. Epidemiology and Related Risk Factors of Preterm Labor as an Obstetrics Emergency. Emerg. 2015;3:10-17.
- Gebreslasie K. Preterm Birth and Associated Factors among Mothers Who Gave Birth in Gondar Town Health Institutions. Adv Nurs. 2016;2-4.
- Steinbock B. Liberty, responsibility, and the common good. Hastings Center Rep.1996;26:45–7.
- Schwartzbaum JA, Wheat JR, Norton RW. Physician breach of patient confidentiality among individuals with human immunodeficiency virus (HIV) infection: patterns of decision. Am J Public Health.1990;80:829–34.