Case Report - Ophthalmology Case Reports (2023) Volume 7, Issue 4
Presumed adenoviral dacryoadenitis with extraocular movement restriction: a case report
Muhannad A. Alnahdi1, Ahmed A. Aldubaikhi1, Abdulrahman Alsaedy1,2,3, Sameera M Aljohani3,4, Mohammed Alrajeh3,5*, Lujain Albadr3,51College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
2Division of Infectious Diseases, Department of Medicine, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia.
3King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
4Microbiology Division, Pathology and Laboratory Medicine, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia.
5Ophthalmology surgery division, King Abdulaziz Medical City, Ministry of the National Guard - Health Affairs, Riyadh, Saudi Arabia.
- *Corresponding Author:
- Mohammed Alrajeh
Ophthalmology surgery division
King Abdulaziz Medical City
Ministry of the National Guard - Health Affairs
Riyadh, Saudi Arabia
E-mail: mohd.rajeh@gmail.com
Received: 19-Jun-2023, Manuscript No. OER-23-103149; Editor assigned: 21-Jun-2023, Pre QC No. OER-23-103149(PQ); Reviewed: 05-Jul-2023, QC No. OER-23-103149; Revised: 25-Jul-2023, Manuscript No. OER-23-103149(R); Published: 01-Aug-2023, DOI: 10.35841/2591-7846-7.4.161
Citation: Alnahdi MA, Aldubaikhi AA, Alsaedy A, et al. Presumed adenoviral dacryoadenitis with extraocular movement restriction: A case report. Am J Ophthalmol 2023;7(4):161.
Abstract
Acute dacryoadenitis usually presents with erythema, tenderness, discharge and enlargement of the lacrimal gland. Viral dacryoadenitis usually exhibits chronicity rather than acute presentation. However, we describe a unique case of acute dacryoadenitis in a 25-year-old immune competent male that presented with history of viral prodrome, painless upper lid swelling and extra-ocular movement restriction. His illness failed to improve with antimicrobials, but completely resolved after corticosteroids. Acute viral dacryoadenitis might be initially misdiagnosed as preorbital cellulitis as seen in this case; thus, this unique entity should be kept in mind to avoid treatment delay and prevent worsening.
Keywords
Dacryoadenitis, Ocular, Acute dacryoadenitis, Patient, Inflammatory.
Introduction
Dacryoadenitis is a rare ophthalmic inflammatory disease of the lacrimal gland that can be caused by infectious causes like bacteria and viruses, and other inflammatory conditions like sarcoidosis [1]. Bacterial organisms are thought to be the most common cause of acute dacryoadenitis while chronic dacryoadenitis is usually viral in origin [2]. The most frequent involved microorganisms are staphylococcus and Epstein bar virus [3]. Adenovirus is known to have ocular manifestations like conjunctivitis, keratoconjunctivitis, and recently reported to cause acute dacryoadenitis [3]. In this article, we describe a case of presumed adenoviral dacryoadenitis that presented with a history of mildly erythematous painless upper lid swelling associated with ocular movement restriction.
Case presentation
A 25-year-old male presented with a four-day history of right upper lid swelling with no visual involvement. The patient had a preceding history of painful periauricular lymph nodes which resolved a day before his presentation. No history of preceding trauma or insect bite, and his past medical, surgical, social, family history were unremarkable.
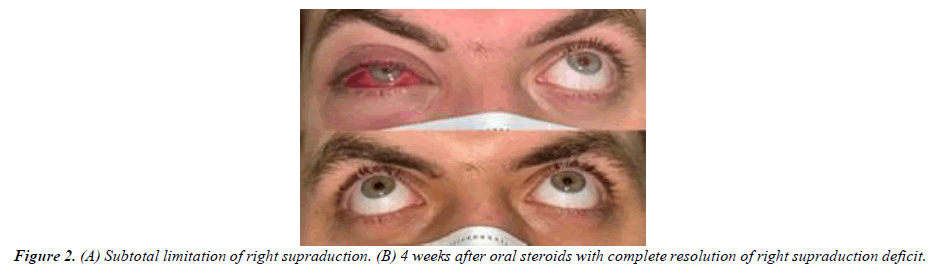
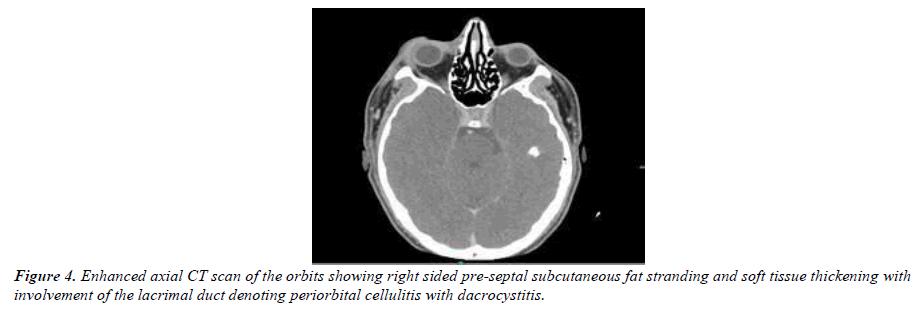
Ocular examination revealed visual acuity of 20/28 in the right eye and 20/25 in the left eye. Mild erythema with painless swelling of the right upper lid was evident with lateral chemosis (Figure 1). The palpebral lobe of the lacrimal gland had no obvious pointing or palpable abscess. Extraocular movements were normal apart from painless (-2) supraduction limitation (Figure 2). Right eye slit-lamp exam showed clear cornea, deep and quiet anterior chamber, clear lens. Left eye examination was unremarkable. Magnetic resonance imaging findings were suggestive of right periorbital cellulitis with mild thickening of the right lacrimal gland. The initial diagnosis was right periorbital cellulitis; thus, the patient was started on vancomycin, ceftazidime, metronidazole as twice daily as an outpatient.
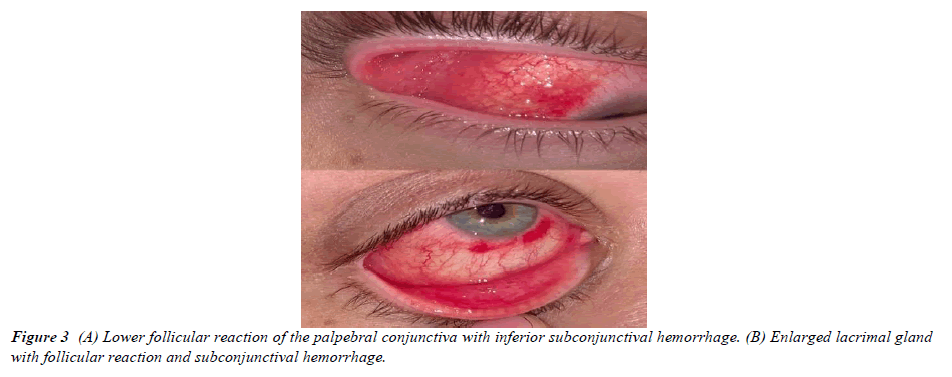
On the 3rd day of presentation, the patient’s clinical status showed no response to treatment, his visual acuity deteriorated to 20/50 in the right eye, and the palpebral lobe of the right lacrimal gland was noted to be enlarged (Figure 3). Notable follicular reaction was seen in the upper and lower palpebral conjunctiva with subconjunctival hemorrhage (Figure 4). No membranes or subepithelial infiltrates were seen, and the limitation of extraocular movement did not improve. The patient’s medications were escalated by the infectious disease team to meropenem and linezolid, and the primary team commenced 50mg oral prednisone for possible viral infection.
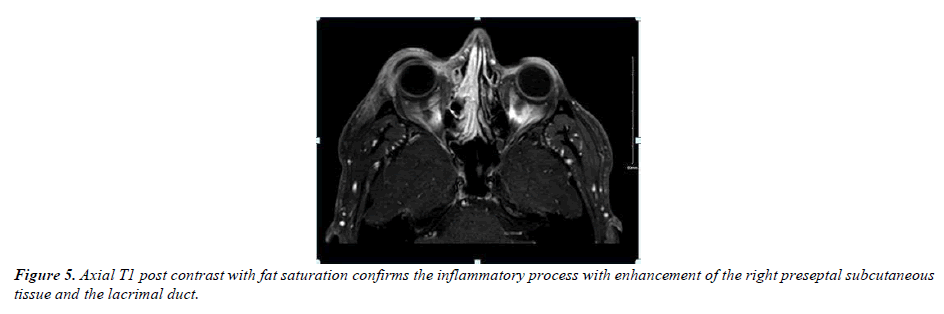
Multiple investigations like complete blood counts, inflammatory markers, and bacterial cultures were unremarkable. Viral conjunctival swaps were sent for a polymerase chain reaction and serum immunoglobulins IgG & IgM for mumps, cytomegalovirus, Epstein bar virus, enterovirus, adenovirus, COVID-19 virus, rhinovirus, and herpes simplex virus, and results were within normal limits (Figure 5).
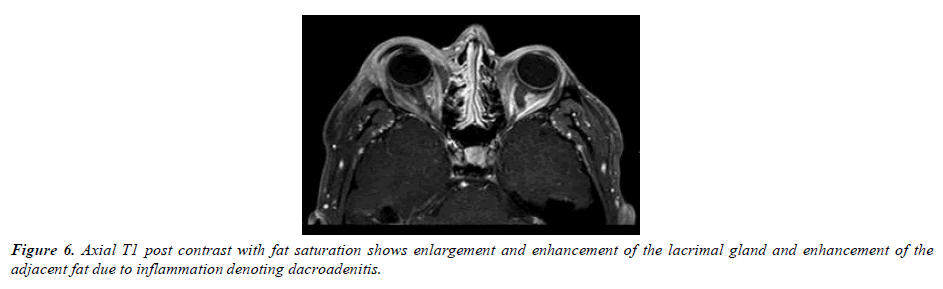
The patient had marked improvement after one day of corticosteroids. Visual acuity improved to 20/30 right eye and 20/20 left eye. Also, evident decrease in the right eye swelling, erythema, subconjunctival hemorrhage, and chemosis was resolved. Prior follicular reaction was noted to be decreased and limitation of supraduction was better (-1). At 1st week follow- up, the patient had near resolution of signs and symptoms with visual acuity of 20/20 in both eyes. Supraduction movement was regained with minimal limitation. Complete recovery was evident after 4 weeks of oral corticosteroids (Figure 6).
Discussion
Acute dacryoadenitis usually presents with erythema, tenderness, discharge, and enlargement of the lacrimal gland while chronic dacryoadenitis usually presents as painless enlargement of the gland [1]. Viruses like mumps, Epstein bar virus, herpes simplex virus, herpes zoster virus, and adenovirus were previously described to cause dacryoadenitis [3-8]. Two similar cases were previously described in patients with concurrent keratoconjunctivitis. Tirkey et al. reported painful dacryoadenitis in 16-year-old male that had adenoviral keratoconjunctivitis [3]. Amjadi et al. described a case of painful erythematous bilateral upper eyelid swelling in a 32- year-old lady that had keratoconjunctivitis [8].
The clinical impression upon the patient’s initial presentation was preorbital cellulitis due to both clinical and radiological suspicion that prompted the initiation of broad-spectrum antibiotics; which did not show any improvement even after treatment escalation. After commencement of steroids, his symptoms had marked improvement pointing towards viral dacryoadenitis. We assume our patient had adenoviral dacryoadenitis due to his clinical signs and symptoms and treatment response. The presence of self-resolved painful periauricular nodes, follicular reaction to the conjunctiva, lack of response to empiric antibiotics, and his marked improvement after steroid therapy supports our assumption of an underlying viral etiology. Notably, the patient presented with supraduction movement restriction and was found to be painless upper eyelid swelling, and, up to our knowledge, these two clinical features have not been reported in the literature.
The patient had marked improvement in supraduction after receiving systemic steroids, possibly owing to its anti- inflammatory and swelling reduction properties. The administration of steroids in dacryoadenitis was previously described in a patient diagnosed with severe dacryoadenitis- related infectious mononucleosis. Aburn et al. described a similar pattern of signs and symptoms resolution days after giving a course of steroids to their patient [9].
Conclusion
Acute dacryoadenitis may initially mimic preorbital cellulitis and could present with painless swelling and extraocular movement limitation as evident in our case. Such unique presentation should be kept in ophthalmologists’ differential diagnosis to avoid delays in patients’ treatment and prevent potential complications. Treatment is deemed to be supportive with administration of corticosteroid to alleviate the underlying inflammatorypathology.
Acknowledgement
A signed consent was taken from the patient.
References
- Aburn NS, Sullivan TJ. Infectious mononucleosis presenting with dacryoadenitis. Ophthalmology. 1996;103(5):776-8.
- Amjadi S, Rajak S, Solanki H, et al. Dacryoadenitis associated with adenoviral keratoconjunctivitis. Clin Experiment Ophthalmol. 2016;44(2):140-2.
- Boruchoff SA, Boruchoff SE. Infections of the lacrimal system. Infect Dis Clin North Am. 1992;6(4):925-32.
- Foster WJ, Kraus MD, Custer PL. Herpes simplex virus dacryoadenitis in an immunocompromised patient. Arch Ophthalmol. 2003;121(6):911-3.
- Galpine JF, Walkowski J.A case of mumps with involvement of the lacrimal glands. BRIT MED J. 1952;1(4767):1069.
- BR J. The clinical features and aetiology of dacryoadenitis. Trans Ophthalmol Soc U K. 1955;75:435-52.
- Obata H, Yamagami S, Saito S, et al. A case of acute dacryoadenitis associated with herpes zoster ophthalmicus. Jpn J Ophthalmol. 2003;47(1):107-9.
- Rhem MN, Wilhelmus KR, Jones DB. Epstein-Barr virus dacryoadenitis. Am J Ophthalmol. 2000;129(3):372-5.
- Tirkey E, Chandravanshi SL, Jain S, et al. Presumed Acute Adenoviral Dacryoadenitis Associated with Epidemic Keratoconjunctivitis: A Case Report. Niger J Ophthalmol. 2014;22(2):90-2.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref