Research Article - Current Pediatric Research (2021) Volume 25, Issue 9
Post-operative changes following endoscopic third ventriculostomy by MR imaging.
Dalia Mohamed El-Mossly1*, Assem Mounir Abdel Latif2, Hanaa Abdelkader Ahmed1, Samar Ramzy Hanna1, Shaimaa Abdelsattar Mohammad1
1 Department of Diagnostic and Interventional Radiology and Molecular Imaging, Ain Shams University, Cairo, Egypt
2 Department of Neurosurgery, Ain Shams University, Cairo, Egypt
- Corresponding Author:
- Dalia Mohamed El-Mossly
Department of Diagnostic and Interventional Radiology and
Molecular Imaging
Ain Shams University
Cairo
Egypt
E-mail: abujamaljameel@gmail.com
Accepted date: 20th September, 2021
Abstract
Background: Endoscopic Third Ventriculostomy (ETV) has increased in popularity in recent years as an acceptable and effective treatment for many children with hydrocephalus. Purpose: To describe the post-operative findings after ETV with clinical correlation and to see if changes in ventricular size existed after ETV are correlated to clinical result. Methods and Materials: A total of 15 pediatric patients underwent ETV at our institution for hydrocephalus during the period of 2019 and 2020. MRI was routinely performed within the first week after surgery and its 3-month follow up. Post-operative clinical assessment was conducted by the neurosurgery team in the early post-operative period and at three and six months if the patient remained well. Results: The overall success rate and failure rate to restore CSF circulation was 73.3% and 26.7%, respectively. It demonstrated the strong association between clinical success and radiographic findings of ventriculostomy success by the presence of signal void within the expected site of third ventriculostoma on T2 weighted sequence (P=0.0088). Also, There was a statistically significant association between late clinical outcome and CSF collection with a signal void seen within it on T2 WI (P<0.001). Prepontine adhesions were seen in all the four failed ETVs. No apparent correlation between the magnitude of the change in ventricular size by Evans’ index even shortly after surgery or after three months and the clinical outcome Conclusion: The MRI study especially T2 weighted images can demonstrate successful ETV procedure by the presence of signal void at the ventriculostomy site, prepontine adhesions and a subcutaneous CSF collection with a signal void seen within it.
Keywords
Endoscopic third ventriculostomy, Neurosurgery, Hydrocephalus.
Introduction
The best treatment for child hydrocephalus has yet to be established [1,2]. Endoscopy and shunt hardware have made significant technological breakthroughs recently; yet, treating hydrocephalus remains one of the most difficult problems experienced by neurosurgeons when deciding on the optimal technique of hydrocephalus therapy [3]. In both obstructive and non-obstructive hydrocephalus, shunts have long been performed to divert Cerebrospinal Fluid (CSF). Currently, Endoscopic Third Ventriculostomy (ETV) has increased in popularity in recent years as an acceptable and effective treatment for many children with hydrocephalus [4,5]
According to prior studies, the patient's age, aetiology, and experience of the surgeon all play a role in determining ETV Success Rates (SRs) [6]. Young children under the age of two, particularly newborns and neonates, appear to have a worse fate. SRs of ETVs done in this age group are shown to range from 0% to 64% in several studies [1,2,6,7]. Other studies found that patients older than 6 months have better outcomes. However, there is still debate about whether ETV is better than shunt insertion in children under the age of six months [8].
The clinical condition following surgery remains the most important factor in determining its effectiveness, and the use of radiological alterations in the ventricular system as a predictor of success in this technique is debatable [9]. As a result, the most comprehensive method to assess the outcome of ETV treatment is to regard shunt independence as similar to success, and additional hydrocephalus treatment owing to either no improvement or relapse as failure [10-12].
A successful ETV is frequently followed by a decrease in ventricular size, although not to normal size [9,11]. The persistent ventriculomegaly's clinical significance is unknown. There are currently no strong arguments to pursue the restoration of the parenchymal mantle as a therapy goal for hydrocephalic patients [13]. There are some authors who believe that the importance of radiological alterations following a successful ETV is secondary to the clinical situation, to the point that postoperative check scans are rarely conducted [9]. For others, however, the presence of larger-than-normal ventricular size following a successful surgery indicates compensated communicating hydrocephalus [14].
The aim of our study was to describe the post-operative findings after ETV with clinical correlation and to see if changes in ventricular size existed after ETV are correlated to clinical result.
Patients and Methods
A total of 15 pediatric patients underwent ETV at our institution for hydrocephalus during the period of 2019 and 2020. The decision to perform this procedure was made by the neurosurgeons. The study was approved by our institutional ethical committee, and an informed consent was given to the patient guardians.Clinical history and examination, including neurological examination focusing on effects of hydrocephalus were done to all patients. Special note taken of manifestations as delayed development, macrocephaly, and symptoms of increased intracranial tension.
MRI was routinely performed within the first week after surgery and its three months follow up. Post-operative clinical assessment was conducted by the neurosurgery team in the early post-operative period and at three and six months if the patient remained well.All patients usually scanned under sedation or general anaesthesia according to our radiology and anaesthesia departments’ guidelines.
Inclusion criteria included
All incoming patients with hydrocephalus who underwent recent third ventriculostomy (within one week of the operation).
Exclusion criteria included
•Patients <6 months due to their high failure rate.
•Patients with known contraindications for MRI examinations, e.g. pacemakers, and aneurysm clips.
•Patients whom operative findings precluded the completion of an adequate third ventriculostomy.
Our MRI protocol
It performed by using a 1.5 T machine (Achieva and Ingenia, Philips medical system, Eindhoven, Netherlands) using an eight-channel SENSE head coil (SENSE acceleration factor of 8) in Ain Shams university hospital.All patients underwent routine MR brain imaging including axial/sagittal T2 WI (TR/TE: 3000-4200 ms); axial FLAIR (TR/TE/TI: 1100/130/2400 ms), axial T1 WI (TR/TE: 450-15 ms) and axial T2* (TR/TE: 756-24 ms).
Image analysis
The obtained images were analyzed to identify hydrocephalus and determine its underlying cause. Sagittal and axial planes in T2 WI were analyzed for the presence or absence of signal void at the level of the ventriculostomy site to determine its patency, and the presence of prepontine adhesions. Moreover, the tract of the surgical procedure from the right parietal burr hole till the floor of 3rd ventricle was examined as well as the subcutaneous region overlying the skull burr hole for the presence of a CSF collection with or without signal void seen on T2 images. Axial T2* images identified the presence of intraventricular air foci.
The ventricular size was measured pre-operatively, early post-operatively (within one week of surgery) and after three months of surgery on axial T2 weighted MR slices with Evans’ index obtained by measuring the maximal bifrontal distance and maximum inner diameter of the skull.
Outcome evaluation
The clinical outcome was assessed using pragmatic criteria that are used in most studies where ETV outcomes had recently been analyzed [10-12,14,15]. ETV clinical success criteria: (a) The patients improved clinically up to their last follow-up visit and required no further intervention to treat hydrocephalus. (b) In patients with chronic hydrocephalus, residual symptoms such as a disturbed gait or memory deficit may to a certain degree persist; however, these symptoms had to improve without further surgery to be considered a satisfactory clinical outcome, (c) The absence of signs or symptoms of raised intracranial pressure, and (d) Shunt independence. ETV clinical failures were categorized as patients who had clinical symptoms of hydrocephalus that never disappeared or resolved and necessitating further hydrocephalus surgery.
The results were documented, calculated, and analyzed using IBM SPSS Statistics 20.0.0 software. The characteristics of the study sample were summarized by descriptive statistics, with dichotomous or ordinal data presented as percentages and continuous data as means with standard deviations. Mann-Whitney test and fisher’s exact test were used. Statistical associations were considered significant if the p value was <0.01.
Results
Among the fifteen patients included in our study, male: female ratio are equals to 1.1:1. The mean age: 3.76 years and median age: 2.5 years; with age range (7 months-15 years). Four ETV procedures were performed in infants aged <1 year old (26.7%), 6 procedures in toddlers 1 year-4yearold (40%), 2 ETVs were performed in preschool age category (4 years-5 years) (13.3%) and another 2 ETVs in childhood period from 5 to 12 years (13.3%). There was one ETV performed in an adolescent from 12 to 18 years (6.7%).
There were 11 cases of aqueductal stenosis (73.3%) in which: 7 cases were congenital due to aqueductal web/membrane, 4 cases were secondary either due to tumours (2 cases) (as tectalglioma) or a posterior fossa arachnoid cyst (1 case) or an arterio-venous malformation (1 case). Chiari II malformation, craniosynostosis, isolated posterior fossa arachnoid cyst and communicating hydrocephalus were seen in other 4 patients.
Regarding the outcome evaluation following ETV: 11 patients showed improvement, among these; 2 patients presented with partial improvement and 9 had complete resolution of the symptoms. Additionally, 3 patients presented initial improvement, but progressive worsening of the symptoms ended up with shunting, and one patient did not improve at all.
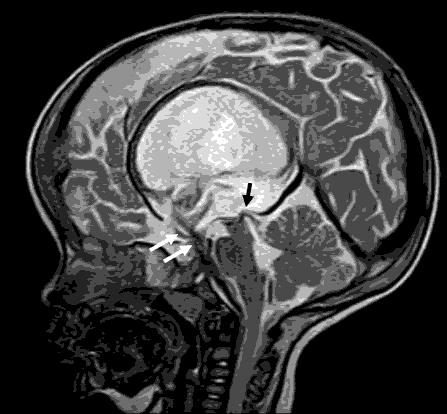
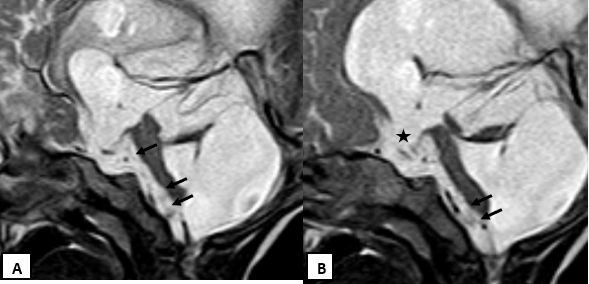
By analyzing axial and sagittal planes T2 WI, a signal void was seen in 11 patients in which 10 ETVs were successful and only one showed failure in late follow-up. However, all patients with no evidence of signal void were failed (3 patients). The difference is statistically significant, p=0.0088 (fisher’s exact test) (Figure 1). Prepontine adhesions were seen in all the four failed ETVs (Figure 2).
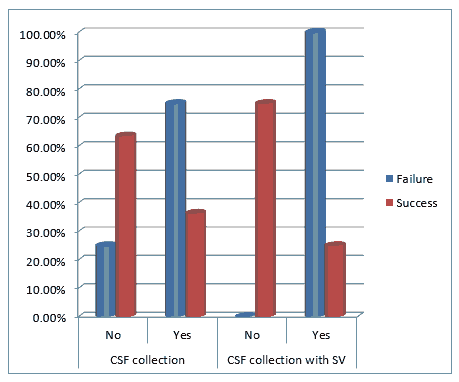
A CSF collection is seen in the subcutaneous area overlying the skull burr hole in the operative site showing signal void on T2 Wis in four patients in which three of them showed failure in late clinical follow up. There was a statistically significant association between late clinical outcome and CSF collection with a signal void within with p-value <0.001 (fisher’s exact test) (Figure 3).
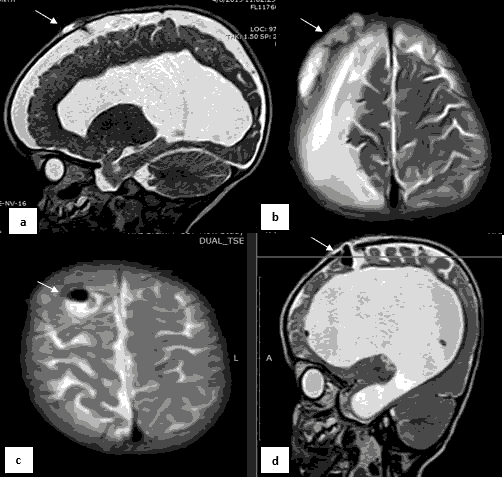
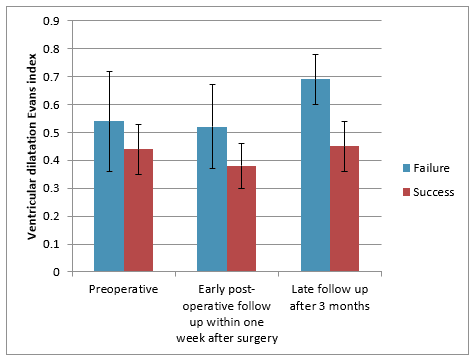
Regarding the ventricular dilatation size measured by Evans’ index done preoperatively, early post-operatively and after 3 months of surgery, there was no statistically significant association between them and late clinical outcome, using: Mann-Whitney test; p-value >0.05 (Figure 4). By reviewing T2* sequence in early post-operative assessment, air foci were detected in most of the cases to be an acceptable post-operative finding Figure 5.
Discussion
The success of ETV is highly varied, and the precise clinical prognosis is unpredictable even in the best-case scenario. CSF leak and hydrocephalus are the most terrible postoperative consequences due to failure or malfunction [10,13]. A single CSF leak can cause meningitis and its associated morbidity [16].
Early clinical identification of ETV failures is challenging, particularly in children, when the only alteration may be an abnormally increasing trend in head circumference. Despite having a patent ETV stoma, patients may show evidence of failure. Hydrocephalus caused by a malfunction can be both causing short- and long-term morbidities [13]. Predicting failure, especially in the very young, might be delayed until critical stages [17]. As a result, anticipating failure, especially noninvasively, is a desirable goal. The value of MRI is a non-invasive method for evaluating the successfulness of the ETV procedure [18].
In our study, we present a one-center experience in 15 hydrocephalic children performed ETV by one neurosurgeon. The overall success rate and failure rate to restore CSF circulation was 73.3% and 26.7%, respectively. The results of this study demonstrate the strong association between clinical success and radiographic findings of ventriculostomy success by the presence of signal void within the expected site of third ventriculo-stoma on T2 weighted sequence.
To the extent of our knowledge, there is lack of information as regards the presence of CSF collection with signal void at the subcutaneous region overlying the surgical pathway. In our study we found a statistically significant association between late clinical outcome and CSF collection with a signal void within with a p-value <0.001. Although it is a small sample because our work is interrupted due to COVID-19 circumstances. This makes recommendations for a larger research study to examine the subcutaneous operative site and the procedural tract for any CSF collections.
When the ventricular size is reduced, the cortical mantle re-expands in most but not all patients. The ventricular system is frequently enlarged even in patients who have a good clinical prognosis and a normal performance status after treatment [12]. The clinical importance of residual ventriculomegaly is still up for discussion. When the ventricles remain enlarged, some authors believe that a functioning third ventriculostomy can convert non-communicating hydrocephalus into an arrested communicating form of hydrocephalus [14].
The results of our study are does not provide additional information to support the use of ventricular size assessment by Evans’ index in the post-operative evaluation of these patients [12]. Our findings corroborate that there is no apparent correlation between the magnitude of the change in ventricular size by Evans’ index observed even shortly after surgery or after three months and the clinical outcome. A moderate decrease in ventricular size does not exclude the possibility of a late clinical failure [19,20].
Conclusion
Apparently, the MRI study especially T2 weighted images indicate an association between the presence of signal void at the ventriculostomy site and the clinical outcome in a follow up period of 3 months. Presence of a subcutaneous CSF collection with a signal void seen within has been found to be correlated to clinical failure as well as the presence of prepontine adhesions. The reliability of Evans’ index ratio has been questioned after having detected a low correlation with late clinical outcome.
Small sample size and short follow up period due to COVID-19 pandemic era are the main obstacles of this study. However, this study is very promising and opens the door for larger samples and longer follows up.
References
- Baldauf J, Oertel J, Gaab MR, et al. Endoscopic third ventriculostomy in children younger than 2 years of age. Childs Nerv Syst 2007; 23(6): 623-6.
- Balthasar AJ, Kort H, Cornips EM, et al. Analysis of the success and failure of endoscopic third ventriculostomy in infants less than 1 year of age. Childs Nerv Syst 2007; 23(2): 151-5.
- Constantini S, Sgouros S, Kulkarni A (2013) Neuroendoscopy in the youngest age group. World Neurosurg 2013; 79(2 Suppl): S23.e1-11.
- Kulkarni AV, Drake JM, Kestle JR, et al. Predicting who will benefit from endoscopic third ventriculostomy compared with shunt insertion in childhood hydrocephalus using the ETV Success Score. J Neurosurg Pediatr 2010; 6(4): 310-5.
- Drake JM, Riva-Cambrin J, Jea A, et al. Prospective surveillance of complications in a pediatric neurosurgery unit. J Neurosurg Pediatr 2010; 5(6): 544-8.
- Duru S, Peiro JL, Oria M, et al. Successful endoscopic third ventriculostomy in children depends on age and etiology of hydrocephalus: outcome analysis in 51 pediatric patients. Childs Nerv Syst 2018; 34(8): 1521-8.
- Buxton N, Macarthur D, Mallucci C, et al.Neuroendoscopic third ventriculostomy in patients less than 1 year old. Pediatr Neurosurg 1998; 29(2): 73-6.
- Ogiwara H, Dipatri AJ Jr, Alden TD, et al. Endoscopic third ventriculostomy for obstructive hydrocephalus in children younger than 6 months of age. Childs Nerv Syst 2010; 26(3): 343-7.
- Buxton N, Turner B, Ramli N, et al. (2002) Changes in third ventricular size with neuroendoscopic third ventriculostomy: A blinded study. J Neurol Neurosurg Psychiatry 2002; 72(3): 385-7.
- Jemiluyi OO, Bank-Ola RF. (2021). The burden of infectious diseases: A Trend appraisal in sub-saharanafrica regional trade blocs. J Sci Res Med BiolSci2021; 2(3): 104-22.
- Kadrian D, Van Gelder J, Florida D, et al. Long-term reliability of endoscopic third ventriculostomy. Neurosurgery 2005; 56(6): 1271-8.
- Kulkarni AV, Drake JM, Armstrong DC, et al.Imaging correlates of successful endoscopic third ventriculostomy. J Neurosurg 2000; 92(6): 915-9.
- Santamarta D, Martin-Vallejo J, Díaz-Alvarez A, et al. Changes in ventricular size after endoscopic third ventriculostomy. Acta Neurochir (Wien) 2008;150(2):119-27.
- ShoukryLR, Mohamed AN, SharafAEA, et al. Diagnostic markers for early detection of neonatal sepsis. J Sci Res Med Biol Sci 2021; 2(3): 13-26.
- Deopujari CE, Karmarkar VS, Shaikh ST. Endoscopic third ventriculostomy: success and failure. J Korean Neurosurg Soc 2017; 60(3): 306-14.
- St George E, Natarajan K, Sgouros S (2004) Changes in ventricular volume in hydrocephalic children following successful endoscopic third ventriculostomy. Childs NervSyst 2004; 20(11-12): 834-8.
- Fukuhara T, Vorster SJ, Luciano MG. Risk factors for failure of endoscopic third ventriculostomy for obstructive hydrocephalus. Neurosurgery 2000; 46(5): 1100-11.
- Bouras T, Sgouros S. Complications of endoscopic third ventriculostomy: a systematic review. Acta Neurochir Suppl 2012; 113: 149-53.
- Fischbein NJ, Ciricillo SF, Barr RM, et al. Endoscopic third ventriculocisternostomy: MR assessment of patency with 2-D cine phase-contrast versus T2-weighted fast spin echo technique. Pediatr Neurosurg 1998; 28: 70-8.
- Udayakumaran S, Joseph T. Can we predict early endoscopic third ventriculostomy failure? The role of ultra-early postoperative magnetic resonance imaging in predicting early endoscopic third ventriculostomy failure. World Neurosurg X 2019; 2: 100013.