Case Report - Ophthalmology Case Reports (2021) Volume 5, Issue 6
Orbital Langerhans cell histiocytosis with multiple fluid fluid levels :a case report
Jafari Reza*
Department of Ophthalmology, Bu Ali Sina Hospital, Mazandaran University of Medical Sciences, Sari, Iran
- Corresponding Author:
- Jafari Reza
Department of Ophthalmology
Bu Ali Sina Hospital
Mazandaran University of Medical Sciences Sari, Iran
Tel: 00989113534558
Email: REZAJ76@YAHOO.COM
Accepted date: August 13 2021
Citation: Reza J. Orbital langerhans cell histiocytosis with multiple fluid-fluid levels: a case report. Ophthalmol Case Rep. 2021;5(6):1-4.
Abstract
Purpose: Langerhans cell histiocytosis (LCH) is a rare disorder that affects the pediatric population. However, LCH presentation as a bony lytic and cystic lesion with fluid-fluid levels (FFLs) is unusual. Observation: We describe imaging and pathologic section features of A 13-year-old boy who presented with several weeks history of a right eyebrow mass with persistent lid swelling and blepharoptosis caused by orbital LCH of the frontal bone with bony lytic lesion and multiple fluidfluid levels. Conclusion and importance: despite some cases of calvarial or orbital LCH previously reported and even a few cases of LCH had fluid-fluid levels, however, our case is first reported orbital LCH with multiple fluid-fluid levels. Keywords: Orbital, Langerhans Cell Histiocytosis (LCH), Fluid-fluid levels.
Keywords
Orbital, Langerhans Cell Histiocytosis (LCH), Fluid-fluid levels.
Introduction
Langerhans cell histiocytosis is an uncommon disorder with unknown etiology that affects pediatrics [1]. Langerhans cell histiocytosis (LCH) is the most common histiocytic disease that develops from the calvarial bone in pediatrics. The characteristic pattern of LCH is a homogeneous enhancement on Magnetic Resonance Imaging (MRI) [2]. However, LCH presentation as a bone lytic and cystic lesion with fluid-fluid levels (FFLs) is unusual. This specific image pattern has been reported rarely [3]. LCH usually presents in younger pediatrics with the age of 1-4 years. In pediatrics older than 10 years, the incidence of LCH is lower. LCH incidence in boys is more than in girls. Orbital involvement is usually uncommon [4]. Therefore, we decide to report a case of orbital LCH in the frontal bone of the orbital roof with multiple fluid-fluid levels.
Case Report
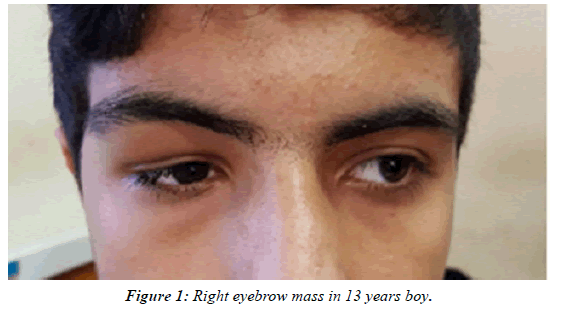
A 13-year-old boy presented with a several weeks history of right eyebrow mass with persistent lid swelling and blepharoptosis without a history of trauma (Figure 1). His levator function was good and blepharoptosis was mechanical. He had mild limitation in elevation and hypothalamus without proptosis. Visual acuity and slit-lamp examination were normal. Ophthalmoscopy was good and RAPD (Relative Afferent Pupillary Defect) was negative. The neurological exam was good, he had no tenderness or bruising over the mass. Hematologic and biochemical value was normal.
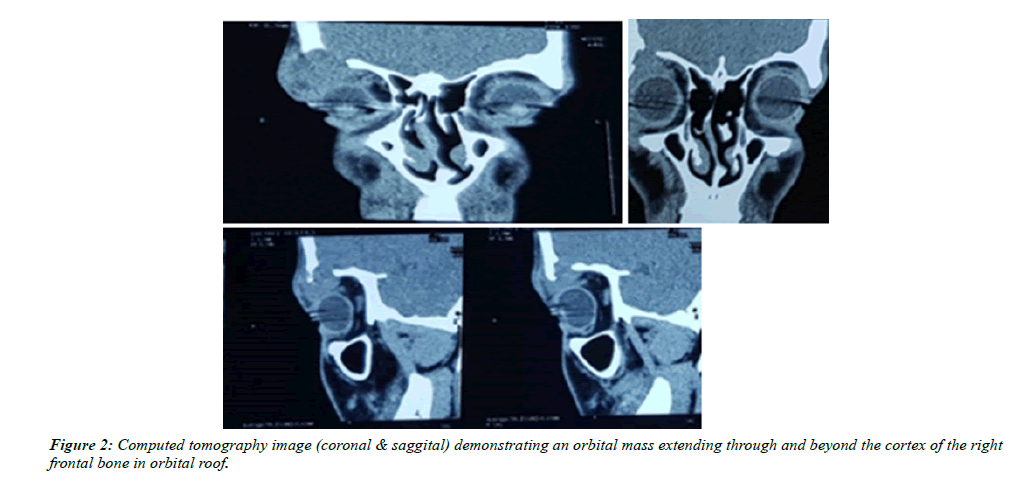
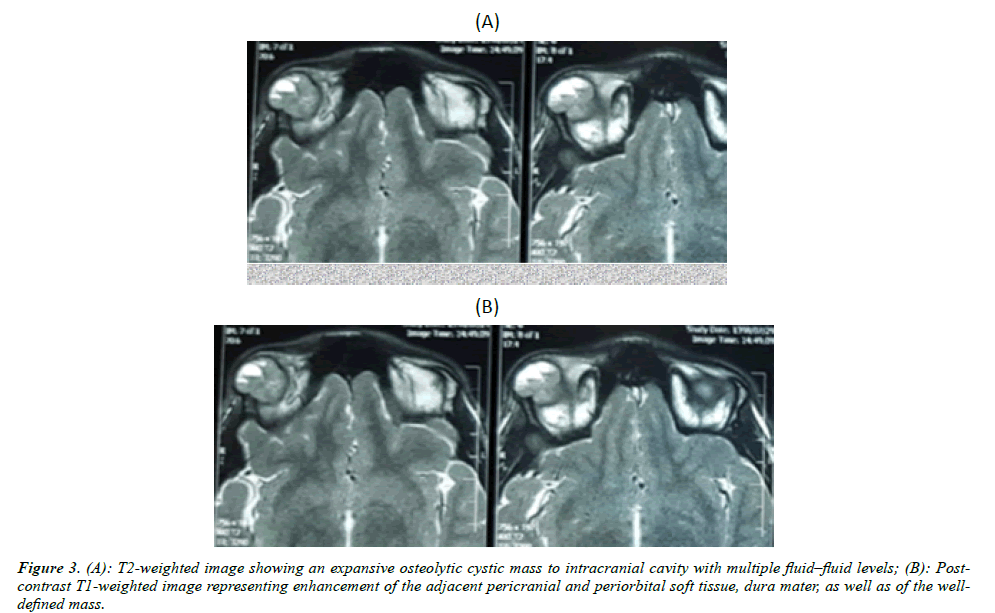
Orbital radiography demonstrated a single osteolytic lesion without sclerosis in the right orbital rim and roof. Computed tomography (CT scan) showed an orbital mass that extended beyond the cortex of the inner and outer tables to the intracranial cavity and shifted the globe inferiorly (Figure 2). T2-weighted images represented several fluid-fluid levels (Figure 3A), Postcontrast T1-weighted images showed enhancement of the lesion and adjacent pericranial and periorbital soft tissue, dura mater. (Figure 3B).
We have a team surgery with a neurosurgeon and orbital surgeon. our approach in surgery was transcranial right lateral coronal incision. after dissection, up to the orbital rim, an extradural multicystic mass containing chocolate color fluid was found that ruptured during surgery, and the hematoma was discharged. surprisingly periorbital and dura mater were intact but the bone border was corrugated.
In Pathological examination of hematoxylin-eosin staining sections showed proliferation of plasma cells, lymphocytes, infiltrated by abundant eosinophils and some multinucleated giant cells. (Figure 4A and 4B) In immunohistochemistry staining scattered multinucleated CD68 positive osteoclastic giant cells were seen. tumoral cells were positive for CD1a and S100 with negative reactivity for CD3, CD20, and CD68. Ki67 was estimated up to 10%. Therefore, the diagnosis of orbital Langerhans histiocytosis (LCH) was confirmed.
Discussion
Langerhans Cell Histiocytosis (LCH) is a rare immunologic disease characterized by histiocytic cell proliferation in several organs. Eosinophilic granuloma is a benign bony lesion that represents a focal or multifocal form of LCH [5]. because our case had focal bone involvement with abundant eosinophils and multinucleated giant cells eosinophilic granuloma type of LCH was suggested. sometimes, acute presentation of a solitary eosinophilic granuloma of the skull is epidural hematoma [5]. Fortunately, our case had no acute symptoms or hematoma in imaging.
The most important fact in imaging was fluid-fluid levels. While fluid-fluid levels have been infrequently encountered in skull lesions due to LCH, they have been reported in lesions of the appendicular skeleton [6]. Recently Dr. Matsushita reported a case of Langerhans Cell histiocytosis with multiple fluid-fluid levels in the parietal bone [7]. The radiographic appearance is well-defined lytic “punched-out” lesions of the skull due to asymmetric destruction of the inner and outer table of cortices and characteristic pattern of the beveled edge [8]. Well-known patterns of Langerhans cell histiocytosis almost is a homogeneous enhancement on MRI [1], whereas in our patient its manifestation was a mass with a lytic lesion of bone containing multiple cystic components with fluid-fluid levels. Nabavizadeh, et al. reported children with skull bone lytic masses containing fluid-fluid levels. The underlying pathology was LCH in four children, aneurysmal bone cysts (ABCs) in three cases, cephalohematoma in three, and metastatic neuroblastoma just in one of these cases [2]. Though FFLs are well-known characteristics of ABCs, the beveled edge appearance, in this case, cannot be seen in ABCs. These FFLs in LCH happened due to hemorrhage, which can be due to trauma or even spontaneously [2]. Therefore, the most probable differential diagnosis for cystic lesions with fluid-fluid levels in pediatric patients is inflammatory lesion specially LCH.
As we know abnormal cells in LCH are derived from myeloid dendritic cells that exhibit the same antigens (CD1a, S100, and CD207) and exhibit the same unique intracytoplasmic organelles, known as Birbeck granules, as in Langerhans cells [7]. Confirmation of Langerhans cells presence was by CD1a and S100 immunostaining [4]. We confirmed these antigens with immunohistochemistry staining.
In conclusion, despite some cases of calvarial or orbital LCH previously reported and even a few cases of LCH in other sites had fluid-fluid levels. however, our case is first reported orbital LCH with multiple fluid-fluid levels. We suggest considering any mass with fluid-fluid level and bony lytic involvement as a Langerhans histiocytosis.
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Conflicts of Interest
The authors declare that they have no financial disclosures
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Funding
No funding or grant support.
Acknowledgments
Thanks for the technical help of neurosurgeon Dr. Meysam Mohseni.
References
- Albadr FB, Elgamal EA, Alorainy IA, Hassan HH. Fluid-fluid level in Langerhans cell histiocytosis of the skull. Neurosciences (Riyadh). 2006;11:47-9.
- D’Ambrosio N, Soohoo S, Warshall C, et al. Craniofacial and intracranial manifestations of Langerhans cell histiocytosis: report of findings in 100 patients. AJR Am J Roentgenol. 2008;191:589-97
- Nabavizadeh SA, Bilaniuk LT, Feygin T, et al. CT and MRI of pediatric skull lesions with fluid-fluid levels. AJNR Am J Neuroradiol. 2014;35:604-608.
- Martina C, Herwig, Ted Wojno, Qing Zhang, et al. MBA Langerhans Cell Histiocytosis of the Orbit: Five Clinicopathologic Cases and Review of the Literatur.Surv Ophthalmol. 2013; 58(4): 330-40.
- Lee YS, Kwon JT, Park YS. Eosinophilic granuloma presenting as an epidural hematoma and cyst. J Korean Neurosurg Soc. 2008;43(6):304-6.
- Varanasi VRK, Leong MY, Tan AM, et al. Langerhans cell histiocytosis: another cause of a fluid-fluid level within an appendicular bony lesion. BJR Case Rep. 2016;2:2015:4-8.
- Matsushita K, et al. Langerhans Cell Histiocytosis with Multiple Fluid–fluid Levels in the Parietal Bone. Magn Reson Med Sci. 2020;19(1):5-6.
- Zaveri J, La Q, Yarmish G, Neuman J. More than just Langerhans cell histiocytosis: a radiologic review of histiocytic disorders. Radiographics. 2014;34(7):2008;24.