Case Report - Journal of Oral Medicine and Surgery (2022) Volume 5, Issue 5
Odontogenic keratocyst in maxillar sinus A case report
Kalaiselvi Vasudevan1*, Ramnath Elangovan2, Sasirekha Balasubramanian3, Sathic Manzoor41Department of Oral Medicine and Radiology, Karpaga Vinayaga Institute of Dental Sciences, Padalam, Tamil Nadu
2Department of Periodontics, Adhiparaskthi Dental College, Melmaruvathur, Tamil Nadu
3Department of Oral Medicine and Radiology, JKKN Dental College, Komarapalayam, Tamil Nadu
4Faculty of Dentistry – Dental Radiology, Selangor, Malaysia
- *Corresponding Author:
- Kalaiselvi Vasudevan
Department of Oral Medicine and Radiology
Karpaga Vinayaga Institute of Dental Sciences
Padalam, Tamil Nadu
E-mail: dr.sks13@gmail.com
Received: 01-Sep-2022, Manuscript No. AAOMT-22-125; Editor assigned: 03- Sep-2022, PreQC No.AAOMT-22-125(PQ); Reviewed: 19-Sep-2022, QC No.AAOMT-22-125; Revised: 22-Sep-2022, Manuscript No.AAOMT-22-125(R); Published: 29-Sep-2022, DOI: 10.35841/aaomt-5.5.125
Citation: Vasudevan K. Odontogenic keratocyst in maxillar sinus- a case report. J Oral Med Surg. 2022;5(5):125
Abstract
Odontogenic Keratocyst (OKC) is a clinicopathologically distinct form of developmental odontogenic cyst. It is known for its aggressiveness biological behavior and high recurrence rate. OKC has a distinct feature to occurin body of the mandible and ramus. This report describes a rare Caseofodontogenic keratocystin maxillary sinusof a35 year old female patient
Keywords
Odontogenic Keratocyst, Keratocystic Odontogenic Tumour, Odontogenic Tumour, Gorlin Syndrome.
Introduction
Keratocysts of the jaw are benign cystic lesions which have a potential for keratinization. Philipsen (1956) and Pindborg, Hansen in (1963) described the clinical and histologic features of this non - inflammatory cyst that uniformly formed keratin. In 1971, the WHO simplified the classification of jaw cysts and made the terms primordial cyst and keratocyst synonymous. This classification emphasized the predominant histological features of the cyst rather than its presumed origin from the primitive enamel organ [1]. In 2003 odontogenic keratocyst (OKC) was designated by the World Health Organization (WHO) recommends the term keratocystic odontogenic tumour (KCOT)as it better reflects its neoplastic nature. WHO has reclassified the lesion as a tumour based on several factors, which include.
Behavior: Locally destructive and highly recurrent.
Histopathology: The basal layer of the KCOT budding into connective tissue and mitotic figures are frequently found in the suprabasal layers.
Genetics: SHH binding to PTCH inhibits growth – signal transduction thereby functioning of PTCH is lost, the proliferation-stimulating effects of SMO become predominate [2].
Case Report
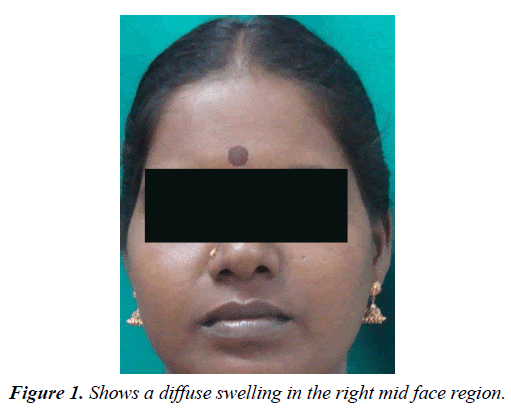
A 35 year old female reported to the Department of Oral Medicine and Radiology, Rajah Muthiah Dental College and Hospital with a complaint of pus discharge from the upper right back region of mouth since 3 months. History revealed that the discharge persisted even after the extraction of periodontally compromised 16.It was not associated with pain or any other discomfort (Figure 1).
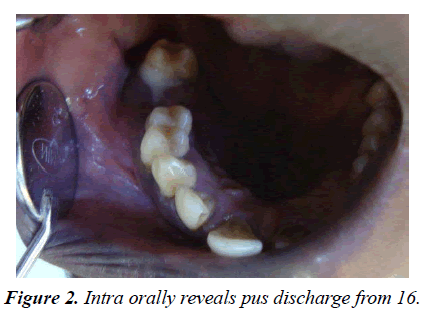
On extra-orally examination, single, diffuse, smooth surfaced swelling, measuring approximately 2×3cm in size seen on the right mid face region. It extended medially upto nose& laterally till malar prominence. Superiorly it extend to involve infra orbital margin& inferiorly upto ala tragal line. Skin over the swelling appeared normal with no secondary changes. On palpation, swelling was warm, soft and non-tender on palpation. There was no evident regional lymphadenopathy. Intra oral examination of hard tissue show congenital missing 18, with pus discharge from the socket of 16 (Figure 2).
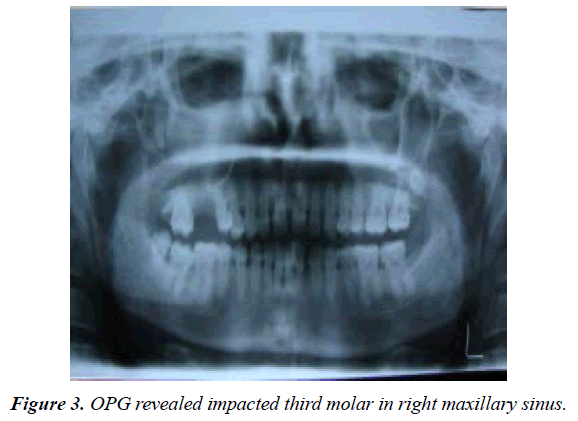
Diagnostic work up included plain film radiographic view (OPG and waters view) and advanced imaging modality. (CT scan with axial and coronal section) (Figure 3) (Figure 4).
A well-defined expansile radilucentlesion s was appreciable in panoramic, waters view and computer tomographic images. On CT axial view a radiopaque mass measuring approximately 3×2 cms in diameter with 1712 HU resembling tooth like structure is seen in right maxillary antrum. Evidance of buccal cortical expansion with radiolucent mass enchroching into the right sinus was better appreciated in the axial view. Breech along the posterolateral wall of the maxillary sinus with deviation of nasal septum and effusion of nasal conchae was appreciated CT.
Surgical enucleation of the lesion along with impacted tooth was done under general anesthesia and tissue was submitted for histopathological examination. Histopathologial diagnosis of KCOT was made.
Discussion
KCOT represents 10% to 12% of odontogenic developmental cysts[3,4].WHO defined KCOT as a benign uni- or multicystic, intraosseous tumour of odontogenic origin, with a characteristic lining of parakeratinized stratified squamous epithelium and it has high potential for infiltration and recurrence.
Peak frequency occur in 2 and 3rd decade. In our case patient was in her third decade of life. They occur most commonly in the mandible, especially in the posterior body and ramus region. In the present case, we report maxillary sinus involvement as a rare site of occurrence. The literature suggests that less than 1% of all case of KCOT occur in maxilla and exhibit sinus involvement. KCOT generally present with localized aggressive, asymptomatic swelling with spontaneous discharge into the oral cavity and mobility of the tooth are common symptoms. In the present case patients present with asymptomatic swelling and discharge. Nasal obstruction, parasthesia are rare symptoms [5].
Multiple KCOT are reported to be associated with nevoid basal cell carcinoma syndrome (NBCCS) or Gorlin-Goltz syndrome. Distinctive clinical feature of NBCCS are nevoid basal cell carcinomas, bifid ribs, calcification of the falx cerebri, frontal bossing, multiple epidermoid cysts and medulloblastoma [6].
Histopathological examination will show cystic lining which will be composed of uniform layer of stratified Squamous epithelium. The luminal surface shows flattened parakeratotic epithelial cells exhibiting wavy appearance. The basal epithelial layer is composed of palisadad layer of coloumnar cells. Similar finding was seen in the present case [7].
Incomplete removal of the cyst lining, growth of a new KCOT from satellite cysts or odontogenic rests left behind after surgery and development of a new KCOT in an adjacent area are few of the proposed mechanism of recurrence reported in literature [2].
Most recurrences take place within 5–7 years after treatment. Literature review suggests that recurrence rate is relatively low with aggressive treatment, whereas more conservative methods tend to result in more recurrent cases [7].
To minimize invasiveness and recurrence, the most effective treatment option appears to be enucleation of the KCOT and subsequent application of Carnoy’s solution. Alternatively, marsupialization followed by cystectomy is likewise effective, as this treatment does not result in a significantly higher rate of recurrence than enucleation plus Carnoy’s solution [8]. In the present case, surgical enucleation with Carnoys solution of the cyst was done under general anesthesia. Impacted tooth was removed along with the lesion.
Conclusion
KCOT occurring in maxillary sinus is a uncommon clinical presentation. Inherent limitation of OPG in interpretating maxillary lesion warrant CT evaluation. The aggressive nature of KCOT needs an aggressive treatment strategy. The odontogenic keratocyst have high rate of recurrence up to 62.5%.
References
- White SC, Pharoah MJ. Oral radiography principles and interpretation. St Louis Mosby. 2004:21-3.
- Langlais RP, Langland OE, Nortjé CJ. Diagnostic imaging of the jaws. Lea Febiger.1995.331-32
- Hodgkinson DJ, Woods JE, Dahlin DC, et al. Keratocysts of the jaw. Clinicopathologic study of 79 patients. Cancer. 1978;41(3):803-13.
- Madras J, Lapointe H. Keratocystic odontogenic tumour: reclassification of the odontogenic keratocyst from cyst to tumour. J Can Dent Assoc. 2008;74(2).
- Gorlin RJ. Nevoid basal cell carcinoma syndrome. Neuro Dis. 1987:67-79.
- Vencio EF, Mota A, Pinho CD, et al. Odontogenic keratocyst in maxillary sinus with invasive behaviour. J Oral Pathol Med. 2006;35(4):249-51.
- Morgan TA, Burton CC, Qian F. A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg. 2005;63(5):635-9.
- Çakur B, Miloglu O, Yolcu U, et al. Keratocystic odontogenic tumor invading the right maxillary sinus: a case report. J Oral Sci. 2008;50(3):345-9.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref