Research Article - Current Pediatric Research (2021) Volume 25, Issue 9
Observational study for allergic rhinitis symptoms causes and treatment at the asthma and allergy center in Karbala.
Mohammed I Rasool1*, Ahmed H Ismael2
1Department of Pharmacology, College of Pharmacy, University of Karbala, Karbala, Iraq
2Department of Clinical Pharmacy, College of Pharmacy, University of Karbala, Karbala, Iraq
- Corresponding Author:
- Mohammed I Rasool
Department of Pharmacology
College of Pharmacy
University of Karbala
Karbala
Iraq
E-mail: abujamaljameel@gmail.com
Accepted date: 29th September, 2021
Abstract
Background: Allergic Rhinitis (AR) is an inflammatory upper respiratory disorder with an increasing global health concern that impacts life quality, school, work attendance, and performance. The management of AR represents collaboration between pharmacists, physicians, other health care professionals, and patients. This study evaluates the awareness of patients to the AR management, if they follow the appropriate steps in treatment, and help them to improve the quality of life and work that are influenced by this disease. Methods: A questionnaire form was designed in order to address the most common symptoms, triggers, drugs used for AR. Additionally, Immunoglobulin E (IgE) test samples were collected and analyzed. Results: A total number of 140 patients of both sexes with AR have participated in this study (80 female and 60 male). The results obtained showed variation in patient’s symptoms, drugs, and dosage forms. At least 67% have the symptom sneezing, 63% was allergic to dust, 51% used loratadine (a second-generation antihistamine) as a treatment, and 41% of the observed patients preferred tablet dosage forms. Conclusion: Based on the results obtained in this study which was carried out in Imam Al-Hussein Medical City (IAHMC) in Karbala, it has been concluded that a high percentage of the population has allergic symptoms, and this is because of our climate as well as family history. Most patients participated in knowing what they should avoid and follow the right steps in pharmacological treatment. Early recognition and management of allergic rhinitis, which includes allergen avoidance, immunotherapy, and pharmacological treatment, can prevent serious complications, and significantly improve the patient's quality of life.
Keywords
Allergic rhinitis, Antihistamine, Immunoglobulin E, Allergy, Karbala.
Introduction
Allergic Rhinitis (AR) is a symptomatic disorder of the nose induced after allergen exposure by an immunoglobulin E-mediated inflammation of the nasal mucosa [1]. AR commonly known as hay fever is a group of symptoms affecting the upper airways [2]. AR represents a global health problem; the prevalence of self-reported AR has been estimated to be approximately 2% to 25% in children and 1% to greater than 40% in adults [3]. AR is not a severe disease, but it alters a patient’s social life, affecting school performance and work productivity. The prevalence in the industrialized world is in increasing, particularly in urban areas. Environmental factors such as air pollution and viral/bacterial infection are frequently considered as triggers for allergic sensitization and possible causes of the increased prevalence [4]. Additionally, a variety of putative factors have been suggested to cause AR and asthma such factors may include changes in lifestyle; increase in exposure to various compounds like allergens, pollution, irritants (smoke, drinks, gas, etc); changes in diet; infections; and stress [1,4].
AR has a complex pathophysiology which includes early- and late-phase allergic responses [5-7]. The process of allergen sensitization is triggered by exposure to allergens such as pollen and/or mites that are recognized by high-affinity antigen-specific Immunoglobulin E (IgE) receptors presented on the surface of all mast cells and basophils in genetically predisposed individuals. The early-phase reaction is associated with an immediate onset, within seconds to minutes, of acute nasal symptoms (such as sneezing and rhinorrhoea) as well as the emergence of ocular symptoms like redness, itching, and watering. These type I hypersensitivity reversible symptoms are caused by histamine release, especially from mast cells in the nasal mucosa [7].
Additional chemical mediators of the rapid hypersensitivity reaction include potent pro-inflammatory cytokines (like the leukotrienes) and eicosanoids (such as prostaglandins and kinins) [5-8]. These mediators, together with the early-phase histamine release, cause vasodilation, production of nasal secretions, and increased vascular permeability which leads to oedema formation [7]. The other is the late-phase allergic reaction which is caused by chemical mediators produced in the early reaction. Within this reaction, in contrast to the early reaction, the main mechanism is eosinophil chemotaxis. The late-phase reaction take place over a period of approximately six hours after exposure to allergens and becomes indolent gradually. The late stages of the allergic response is characterized by inflammatory reaction and immune cell infiltrate, including monocytes, T-lymphocytes, basophils, neutrophils, and eosinophils as well as the release of multiple mediators such as leukotrienes, cytokines, and prostaglandins. These processes eventually result in nasal obstruction which is considered to be the main symptom of AR patients and one of the most troublesome symptoms [8].
Complications that are commonly associated with AR include bacterial sinusitis and nasal polyps as well as comorbid conditions like asthma, atopic dermatitis, and allergic conjunctivitis. Untreated chronic disease can result in mucosal remodeling, atrophic skin changes, and overall higher chance of morbidity [9].
The diagnosis of AR is based on a typical medical history includes a careful description of symptoms, environmental factors, and exposures, family history, results of previous therapy and diagnostic tests, use of medications, former nasal injury or surgery [10]. When at least two symptoms out of watery rhinorrhea, sneezing, nasal obstruction and nasal pruritus persist for at least one hour on most of the symptomatic days, AR is highly suspected. In this condition, disease severity should be classified according to the Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines which is based on duration and severity of symptoms. A confirmative diagnosis should be set up by the skin prick test or the serum-specific IgE level [11].
Previous studies carried out in Western countries commonly focused on the effects of drugs, pollens, pets, and family history on the presentation of AR [12-14]. Conversely, Asian countries concentrated more on the education attainment, family history, pet adoption, as well as smoking and drinking habits, as risk factors of AR [15-20]. Therefore, the interaction between environmental factors and individual susceptibility is important [21]. The current study evaluates the awareness of patients to the AR management and investigates the degree of symptom control and medication used in patients after starting medical treatment for AR. Collectively, this communication provides useful information relevant to symptoms and drugs used to improve the quality of life and work that are influenced by this disease.
Materials and Methods
This study was carried out on patients in Imam Al-Hussein Medical City (IAHMC) in Karbala province/Iraq. The patients were asked about their symptoms of allergic rhinitis, the triggers of the allergic reaction, the drugs they used, and in which dosage form. A screening questionnaire form was designed for this purpose depending on the previous studies and the most common questions in society. The patients who participated in this study were selected randomly from the patients in the otorhinolaryngology department in the hospital (IAHMC) by using direct interviews. A total number of 140 patients were included in this investigation. The subjects were screened in the same season to avoid potential seasonal differences.
The IgE test using the Polycheck® screening assay kit (a brand of biocheck, Münster, Germany) which are test kits for human serum diagnostics to test for allergies as well as autoimmune disorders. Samples of this test were collected for the studied subjects in order to find the most common allergic triggers that the patient can be exposed to during their daily life. Statistical analysis: descriptive statics was performed using SPSS and Microsoft Excel programs for Microsoft Windows (release 10.0), and results were represented in tables and diagrams.
Results
Demographic data
A total number of 140 patients with AR were participated in this study, with an age range (18-55 years) of both sexes. The demographic data of the studied participants are summarized in Table 1.
| Total no. | Females | Males | Age |
|---|---|---|---|
| 140 | 80 | 60 | 18-55 adults |
Table 1. Details of participated patient.
Symptoms of allergic rhinitis
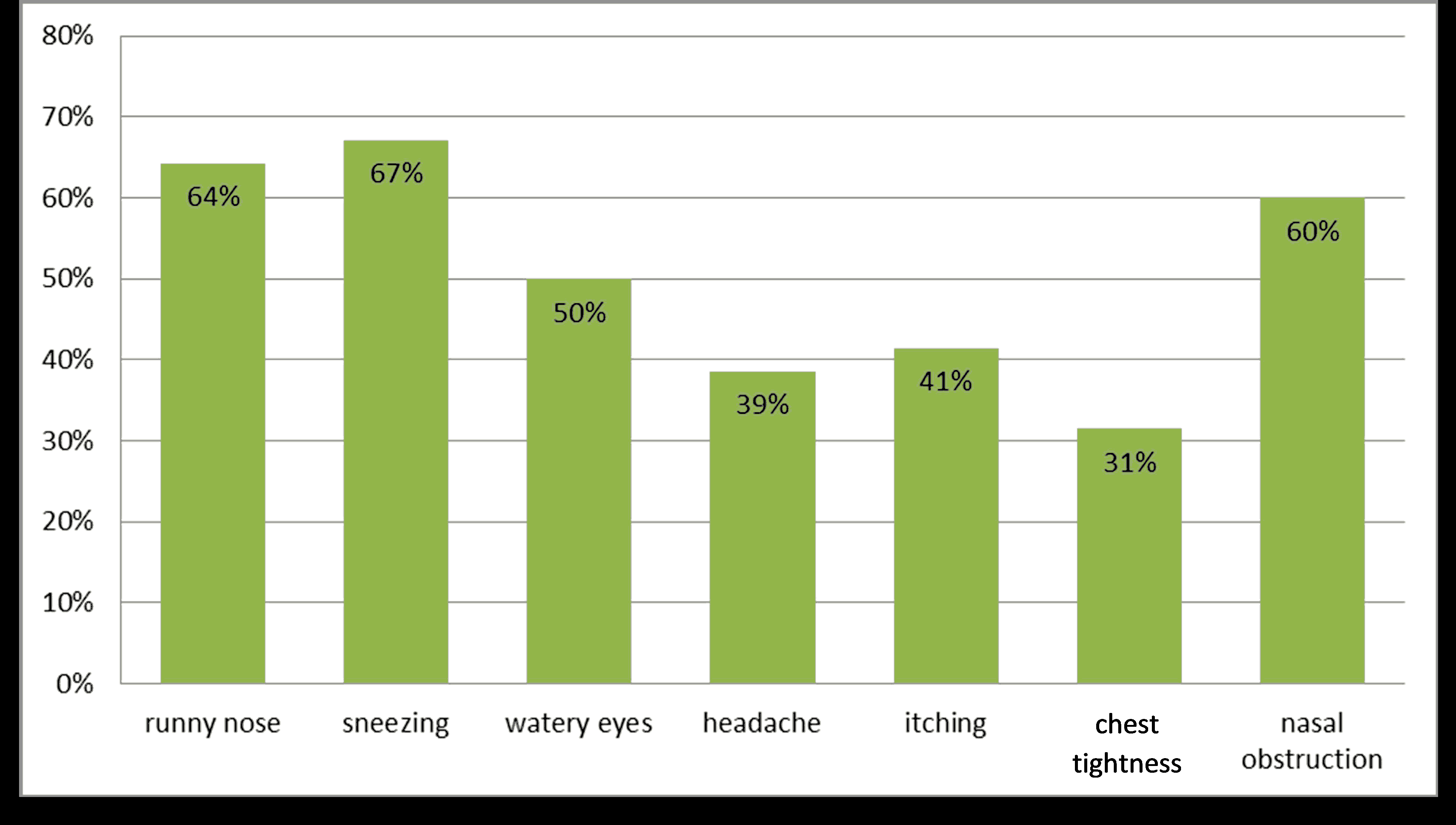
This part of the study covered the most common symptoms that the patients with AR suffered from as shown in Table 2. The prevalence of AR symptoms in patients are depicted in Figure 1.
| Symptoms | No. of patients | Percentage % |
|---|---|---|
| Runny nose | 90 | 64% |
| Sneezing | 94 | 67% |
| Lacrimation | 70 | 50% |
| Headache | 54 | 39% |
| Itching | 58 | 41% |
| Chest tightness | 44 | 31% |
| Nasal obstruction | 84 | 60% |
Table 2. Symptoms of allergic rhinitis patients.
As shown in Figure 1 the most common symptoms that the AR patients suffered from were respectively (sneezing, runny nose, nasal obstruction, and watery eyes), and in less frequent (itching, headache, and breath difficulty or chest tightness).
Causes of allergic rhinitis
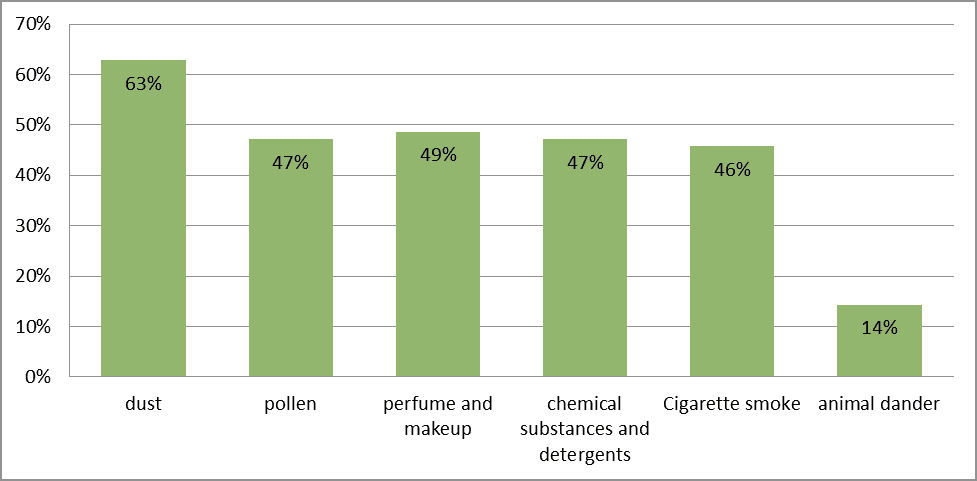
This part of the study covered the environmental triggers of allergic reaction in the studied subjects, Table 3.
| Triggers | No. of patients | Percentage % |
|---|---|---|
| Dust | 88 | 63% |
| Pollen | 66 | 47% |
| Perfume and makeup | 68 | 49% |
| Chemical substances and detergents | 66 | 47% |
| Cigarette smoking | 64 | 46% |
| Animals dander | 20 | 14% |
The highest proportion of at least 63% of patients, in this study, developed the allergic symptoms after the exposure to dust and, in less extent, to other triggers as shown in Figure 2.
Drugs used to treat AR
This part of the investigation is essential to detect the most common drugs that have been used by the patients of AR, Table 4.
| Drugs | No. of patients | Percentage % |
|---|---|---|
| Desloratadine | 34 | 24% |
| Fexofenadine | 2 | 1% |
| Loratadine | 72 | 51% |
| Chlorpheniramine | 26 | 19% |
| Diphenhydramine | 38 | 27% |
| Cetirizine | 12 | 9% |
| Pseudoephedrine | 4 | 3% |
| Sodium cromoglycate | 4 | 3% |
| Xylometazoline (Otrivin)® | 26 | 19% |
| A combination of ascorbic acid/chlorpheniramine/dexamethasone (Hayanil)® | 30 | 21% |
| A combination of triprolidine and pseudoephedrine (Actifed)® | 14 | 10% |
| Azelastine (Rhinolast)® | 0 | 0% |
| Ipratropium bromide | 0 | 0% |
| Beclomethasone | 6 | 4% |
| Triamcinolone acetonide (Nasocort)® | 2 | 1% |
| Fluticasone propionate (Flonase)® | 6 | 4% |
| Mometasone furoate (Nasonex)® | 30 | 21% |
| Budesonide (Rhinocort)® | 14 | 10% |
| Xylometazoline (Xylo acino)® | 12 | 9% |
| Seawater (Nasal saline) | 20 | 14% |
| Montelukast | 24 | 17% |
Table 4. Drugs used by the allergic rhinitis patients.
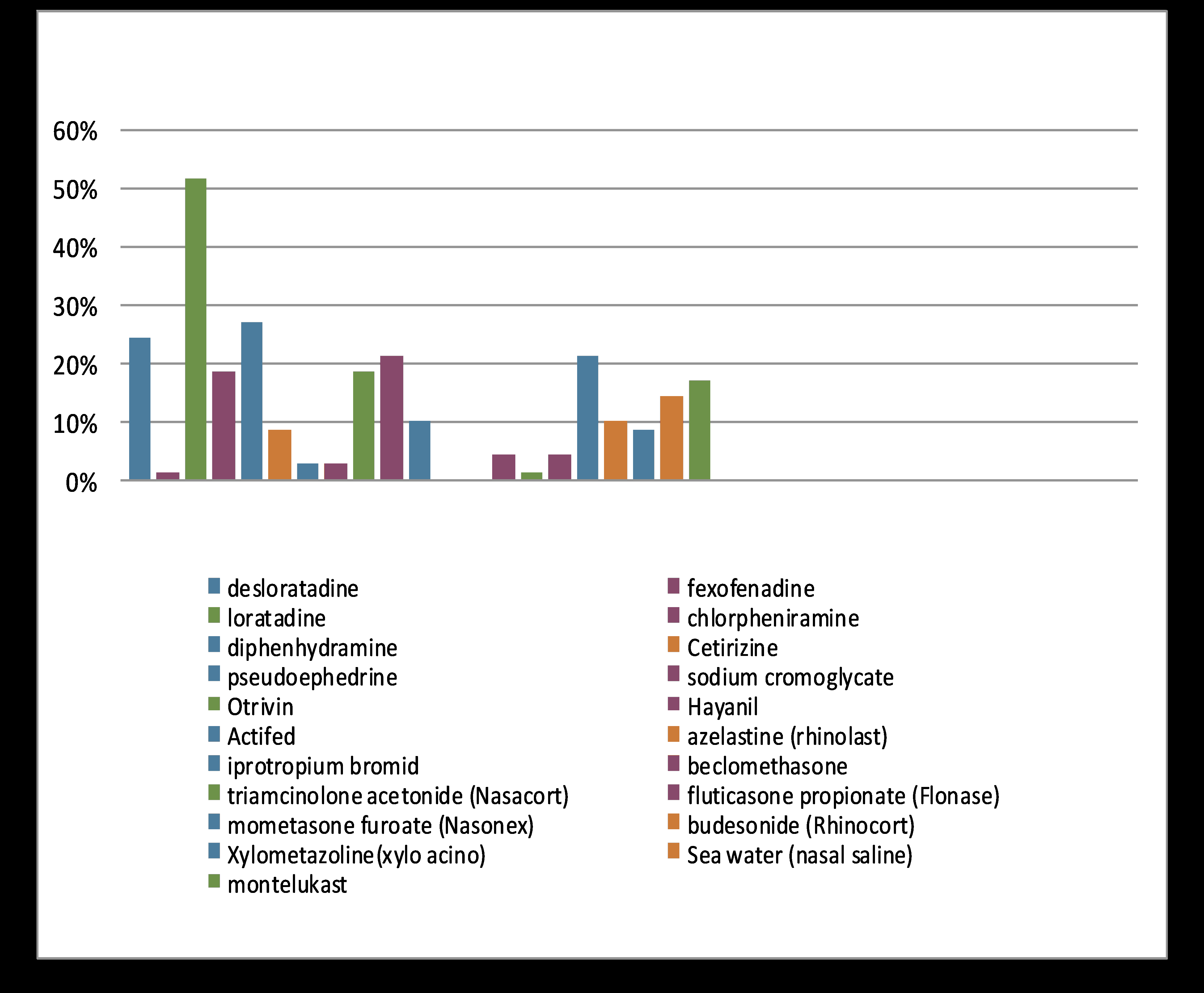
Antihistamine drugs e.g. (loratadine, desloratadine, chlorpheniramine, and diphenhydramine were the most common drugs consumed in the treatment of the AR patients. Hayanil® (a combination of the active ingredients ascorbic acid, chlorpheniramine, and dexamethasone) was also widely used to treat the AR symptoms as shown in Figure 3. The topical corticosteroids are not used as frequently as antihistamines.
The dosage form of drugs
This part of the study shows which dosage forms of the medications frequently used by the patients in Table 5.
| Dosage form | No. of patients | Percentage % |
|---|---|---|
| Sprays and drops (local) | 36 | 26% |
| Tablets (systemic) | 58 | 42% |
| Tablets, sprays, and drops (systemic and local) | 46 | 33% |
Table 5. Dosage forms of the used allergic rhinitis drugs.
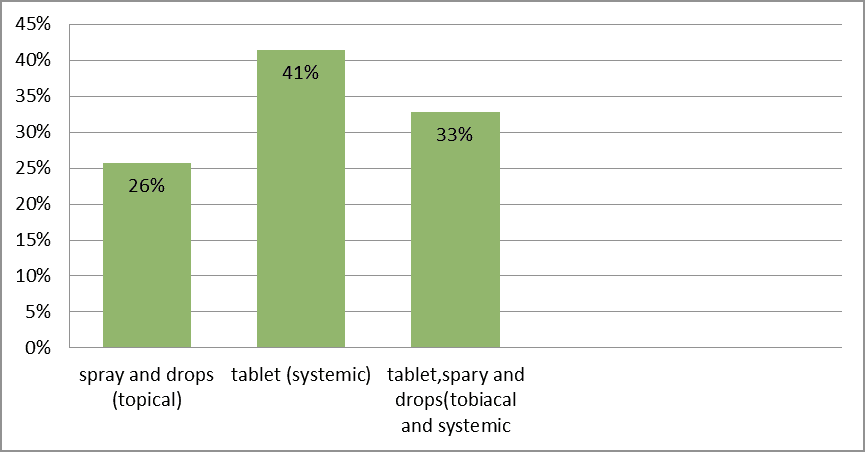
Tablets were the most dosage form used in at least 41% of the patients, followed by mixed treatments of both systemic and local drugs presented with 33% of patients. The sprays and drops alone accounted 26% of patients were the less frequent to be utilized, as shown in Figure 4.
IgE test samples
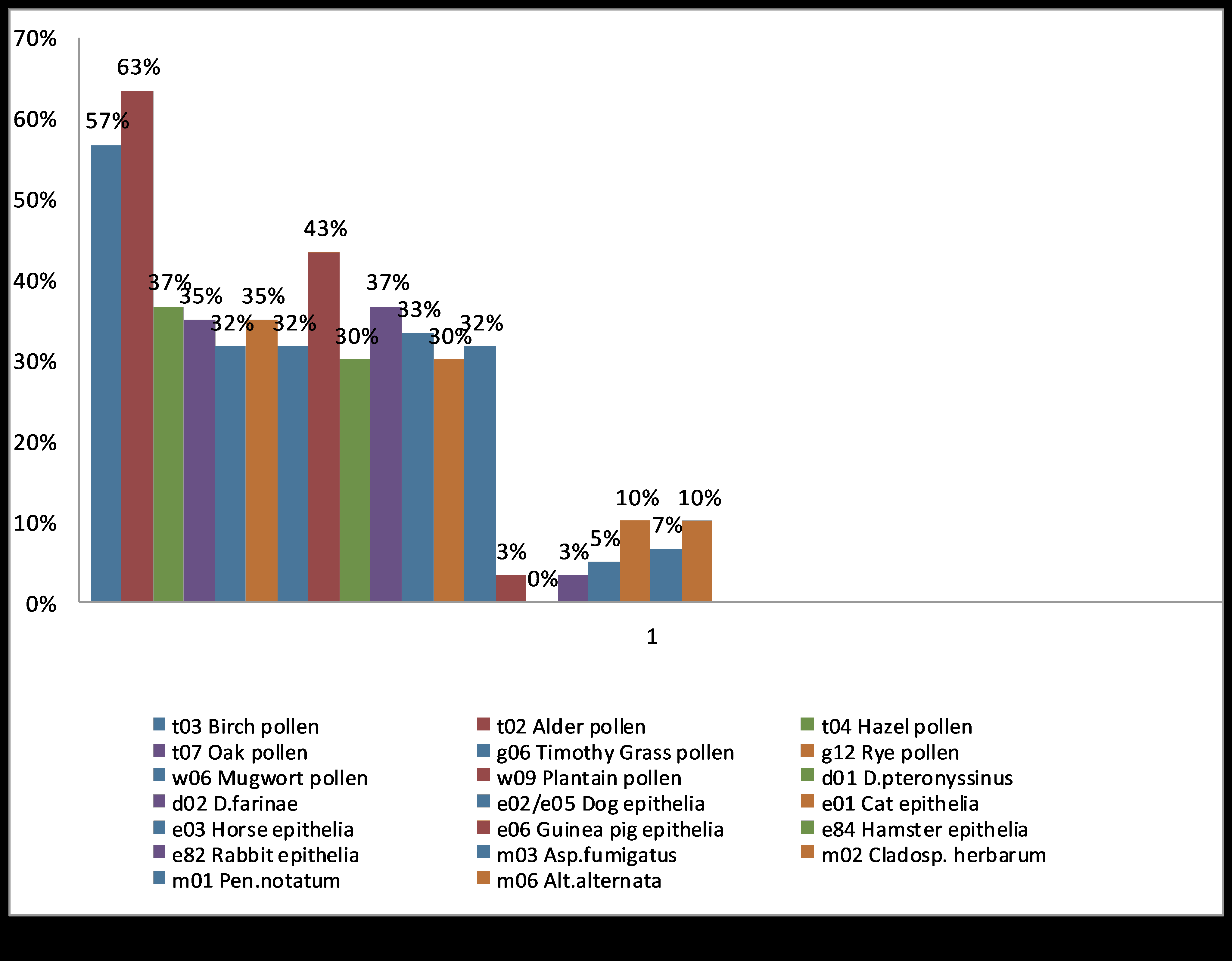
The samples for the allergen specific IgE screening assay were collected to indicate the allergens that the investigated AR patients may show sensitivity towards them in Table 6.
| Allergens | No. of patients | Percentage (%) |
|---|---|---|
| Birch pollen | 80 | 57% |
| Alder pollen | 88 | 63% |
| Hazel pollen | 52 | 37% |
| Oak pollen | 49 | 35% |
| Timothy Grass pollen | 45 | 32% |
| Rye pollen | 49 | 35% |
| Mugwort pollen | 45 | 32% |
| Plantain pollen | 60 | 43% |
| D. pteronyssinus | 42 | 30% |
| D. farinae | 52 | 37% |
| Dog epithelia | 46 | 33% |
| Cat epithelia | 42 | 30% |
| Horse epithelia | 45 | 32% |
| Guinea pig epithelia | 4 | 3% |
| Hamster epithelia | 0 | 0 |
| Rabbit epithelia | 4 | 3% |
| Asp. fumigatus | 7 | 5% |
| Clasp. herbarium | 14 | 10% |
| Pen. notatum | 10 | 7% |
| Alt. alternata | 14 | 10% |
Table 6. Results of allergen specific IgE screening assay.
The highest proportion of 63% of patients developed allergic symptoms when they were exposed to the alder pollen while 57% of patients have an allergy to birch pollen. The other materials are shown in Figure 5.
Discussion
Both Allergic Rhinitis (AR) and sensitization are considered chronic conditions with increasing prevalence worldwide [22]. AR patients can go through a variety of troublesome clinical symptoms which are mostly insufficiently acknowledged and underreported resulting in a delay in medical management and ultimately a decrease in the patient health related life quality [23]. Medical attention of AR should be individualized and based on the spectrum, duration, and severity of symptoms, physical examination findings, comorbidities, the age of the patients, and patient preferences. It is beneficial to understand the medical measures for AR patients as well as pointing out the environmental factors that trigger allergy [24,25].
In this investigation, some considerations may help in the treatment and improvement of the life quality of AR patients. It was noted that the most common inconvenient symptoms in AR patients were at least 67% sneezing, 64% runny nose, 60% nasal obstruction, 50% watery eyes, 41% itching, and 39% headache. A previous study, undertaken in the Middle East region which included five countries (Egypt, Iran, Lebanon, Saudi Arabia, and the United Arab Emirates) reported that these bothersome signs were one of the most common symptoms of AR [26]. The reported symptoms are a response of the allergic reaction which results from the release of histamine, leukotriene, prostaglandin, and other mediators [27-30]. The identification of the most common symptoms, the impact of AR on the population, and highlighting the treatment gaps will provide better understanding and treatment of AR, leading to improvements in the overall patient’s management and life quality [31].
Furthermore, the data shows that at least 63% of patients developed allergic reactions after exposure to dust; this was expected due to the climate changes of Iraq which is known for its increasing incidence of sandstorms which is shown in Table 3 [32]. Dust was a trigger factor for AR in other countries that have a comparable climate like, Saudi Arabia and UAE which presented with at least 74% and 59% respectively, of patients allergic to dust [33].
An earlier study reported that desert regions are found in south and north of Iraq, with a fertile lower Mesopotamian plain supported by both the Tigris and Euphrates rivers. Yearly, dust and sandstorms occur and reaches their peak from May to October [34]. Moreover, the allergen specific IgE tests showed that at least 32%-63% of the studied patients exert sensitivity to several types of pollens (Table 6 and Figure 5). A former study involved pollen and mold survey in the Iraqi capital Baghdad reported periodic peaks of penicillium, alternaria, aspergillus, and hormodendrum. Several individuals had positive skin tests with grass, weed, and tree pollens after being tested with several seasonal aeroallergens [35].
About 49% of the tested individuals were allergic to makeup and perfumes this was because the highest proportion of patients that took part in the current study were women that usually use such products. Furthermore, at least 46% of the patients were allergic to cigarette smoke and about 14% of patients were allergic to animal dander (Table 3). Such decrease might be related to Karbala urban society and religion that show limitations to handle or raise pets. This relatively low percentage of allergic patients to animals was also reported in other countries like Iran and UAE which showed 18% and 4%, respectively [31].
Additionally, the current study showed that more than half of the patients used the drug loratadine for relieve of AR symptoms. Loratadine a second-generation, non-sedating antihistamine that is one of the first line pharmacological treatments recommended for all patients with AR [32]. The second-generation oral antihistamines have been found to efficiently relieve rhinorrhea, itching, and sneezing when taken prophylactically or regularly at the time of maxima symptoms from the exposure to an allergen [30]. The first-generation sedating antihistamines, diphenhydramine and chlorpheniramine, were used in a lesser percentage, 27% and 19%, respectively by the studied patients than the second-generation oral antihistamines. Although the older first-generation antihistamines are also effective in reducing the symptoms of AR, they have been shown to exert a negative effect on the functioning and cognition of the patients due to their somnolence effect. Therefore, they are not routinely recommended for AR treatment. In addition to the second-generation antihistamines, intranasal steroids are also considered as first-line therapy for patients with more severe AR symptoms [25-32].
About 41% of patients prefer tablets, 33% prefer both tablets and spray, and 26% prefer spray only dosage forms (Figure 4 and Table 5). The oral tablet dosage form is easy to be self-administered, maintains the accuracy of dose, and cheaper from other available dosage forms [33]. To conclude, the results that were obtained from the current study which was done in Imam Al-Hussein Medical City (IAHMC) in Karbala displayed a high percentage of the population suffered from disturbing allergic symptoms and this was because of our climate and family history. Early recognition and management of AR, which includes allergen avoidance, immunotherapy, and pharmacological treatment, can prevent serious complications and significantly improve the patient's quality of life. Consequently, the identification of the unwanted symptoms was found to be essential in the management of AR and pointing out the most frequent symptoms will definitely aid in the selection of the proper medications to be used. Pending additional studies, such information may aid in the formulation of personalized regimens for individuals with AR [35].
Abbreviations
IgE: Immunoglobulin E; AR: Allergic Rhinitis; IAHMC: Imam Al-Hussein Medical City; PAR: Perennial Allergic Rhinitis; SAR: Seasonal Allergic Rhinitis.
Conflict of Interest
None declared.
References
- Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA (2) LEN and AllerGen). Allergy 2008; 63(86): 8-160.
- Cvetkovski B, Kritikos V, Yan K, et al. Tell me about your hay fever: A qualitative investigation of allergic rhinitis management from the perspective of the patient. NPJ Prim Care Respir Med 2018; 28(1): 3.
- Brożek JL, Bousquet J, Agache I, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol 2017; 140(4): 950-958.
- Wang DY. Risk factors of allergic rhinitis: Genetic or environmental?. Ther Clin Risk Manag 2005; 1(2): 115-123.
- Min YG. The pathophysiology, diagnosis and treatment of allergic rhinitis. Allergy Asthma Immunol Res 2010; 2(2): 65-76.
- Sin B, Togias A. Pathophysiology of allergic and non-allergic rhinitis. Proc Am Thorac Soc 2011; 8(1): 106-114.
- Bjermer L, Westman M, Holmström M, et al. The complex pathophysiology of allergic rhinitis: Scientific rationale for the development of an alternative treatment option. Allergy Asthma Clin Immunol 2019; 15: 24.
- Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol 2006; 117(2): S450-S456.
- Stull DE, Roberts L, Frank L, et al. Relationship of nasal congestion with sleep, mood, and productivity. Curr Med Res Opin 2007; 23(4): 811-819.
- Tamay Z, Akcay A, Ones U, et al. Prevalence and risk factors for allergic rhinitis in primary school children. Int J Pediatr Otorhinolaryngol 2007; 71(3): 463-471.
- Sultész M, Katona G, Hirschberg A, et al. Prevalence and risk factors for allergic rhinitis in primary schoolchildren in Budapest. Int J Pediatr Otorhinolaryngol 2010; 74(5): 503-509.
- Kuyucu S, Saraçlar Y, Tuncer A, et al. Epidemiologic characteristics of rhinitis in Turkish children: The International Study of Asthma and Allergies in Childhood (ISAAC) phase 2. Pediatr Allergy Immunol 2006; 17(4): 269-277.
- Li CW, De Chen H, Zhong JT, et al. Epidemiological characterization and risk factors of allergic rhinitis in the general population in Guangzhou City in China. PLoS One 2014; 9: 1-16.
- Ziyab AH. Prevalence and risk factors of asthma, rhinitis, and eczema and their multimorbidity among young adults in Kuwait: A cross-sectional study. Biomed Res Int 2017; 2017: 2184193.
- Phathammavong O, Ali M, Phengsavanh A, et al. Prevalence and potential risk factors of rhinitis and atopic eczema among schoolchildren in Vientiane capital, Lao PDR: ISAAC questionnaire. Biosci Trends 2008; 2(5): 193-199.
- Hsu SP, Lin KN, Tan CT, et al. Prenatal risk factors and occurrence of allergic rhinitis among elementary school children in an urban city. Int J Pediatr Otorhinolaryngol 2009; 73(6): 807-810.
- Lim FL, Hashim Z, LTL T, et al. Asthma, airway symptoms and rhinitis in office workers in Malaysia: Associations with House Dust Mite (HDM) allergy, cat allergy and levels of house dust mite allergens in office dust. PLoS One 2015; 10: 1-21.
- Chong SN, Chew FT. Epidemiology of allergic rhinitis and associated risk factors in Asia. World Allergy Organ J 2018; 11(1): 17.
- Bousquet J, Van Cauwenberge P, Khaltaev N, et al. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 2001; 108(5): S147-S334.
- Thompson A, Sardana N, Craig TJ. Sleep impairment and daytime sleepiness in patients with allergic rhinitis: the role of congestion and inflammation. Ann Allergy Asthma Immunol 2013; 111(6): 446-451.
- Lakhani N, North M, Ellis AK. Clinical manifestations of allergic rhinitis. J Aller Ther 2012; S5: 007.
- Frati F, Dell'Albani I, Passalacqua G, et al. A survey of clinical features of allergic rhinitis in adults. Med Sci Monit 2014; 20: 2151-2156.
- Bodtger U, Linneberg A. Remission of allergic rhinitis: An 8-year observational study. J Allergy Clin Immunol 2004; 114(6): 1384-1388.
- Takano H, Inoue KI. Environmental pollution and allergies. J Toxicol Pathol 2017; 30(3): 193-199.
- Abdulrahman H, Hadi U, Tarraf H, et al. Nasal allergies in the Middle Eastern population: Results from the "Allergies in Middle East Survey". Am J Rhinol Allergy 2012; 26(1): S3-S23.
- Al-Ansari N, Sissakian VK, Knutsson S. Climate change: Consequences on Iraq’s Environment. J Earth Sci Geotech Eng 2018; 8(3): 43-58.
- Waibel KH. Allergic rhinitis in the Middle East. Mil Med 2005; 170(12): 1026-1028.
- Al-Tikriti SK, Al-Salihi M, Gaillard GE. Pollen and mold survey of Baghdad, Iraq. Ann Allergy 1980; 45(2): 97-99.
- Small P, Keith PK, Kim H. Allergic rhinitis. Allergy Asthma Clin Immunol 2018; 14(2): 51.
- Small P, Frenkiel S, Becker A, et al. The Canadian rhinitis working group. Rhinitis: A practical and comprehensive approach to assessment and therapy. J Otolaryngol 2007; 36(1): 5-27.
- Kim H, Kaplan A. Treatment and management of allergic rhinitis feature. Clin Focus 2008; pp: 1-4.
- Church MK, Church DS. Pharmacology of antihistamines. Indian J Dermatol 2013; 58(3): 219-224.
- Bozek A. Pharmacological Management of Allergic Rhinitis in the Elderly. Drugs Aging 2017; 34(1): 21-28.
- Rosenwasser LJ. Treatment of allergic rhinitis. Am J Med 2002; 113(9A): 17S-24S.
- Gaikwad SS, Kshirsagar SJ. Review on Tablet in Tablet techniques. Beni-Suef Univ J Basic. Appl Sci 2020; 9:1.