Research Article - Current Pediatric Research (2017) Volume 21, Issue 3
Neonatal hyperbilirubinemia as a risk factor for hearing loss.
Juan C Falcón González*, Cándido Corujo-Santana, Silvia A Borkoski-Barreiro, Ángel Ramos-MacíasOtorhinolaryngology, Head and Neck Surgery Department, Complejo Hospitalario Universitario Insular Materno Infantil, Las Palmas University, Las Palmas of Gran Canaria, Spain.
- Corresponding Author:
- Juan C Falcón González
Complejo Hospitalario Universitario Insular-Materno Infantil
Av. Marítima del Sur s/n-Las Palmas de Gran Canaria, 35016, Spain
Tel: +34-928441801
Fax: +34-928444068
E-mail: jfalgond@gobiernodecanarias.org
Accepted date: June 22, 2017
Abstract
Objective: The Objective is to analyse newborn hyperbilirubinemia as risk factor for hearing loss in children born in the Hospital of Insular Maternal and Child University Hospital Complex, between 2007 and 2013. Materials and methods: Retrospective study of 796 new-borns with hyperbilirubinemia at birth, by transient-evoked otoacoustic emissions and brainstem auditory evoked potentials. Results: 185 new-borns (23.24%) were referred for brainstem auditory evoked potentials. 35 new-borns (4.39%) were diagnosed with hearing loss: 18 (51.43%) with conductive hearing loss and 17 (48.57%) with sensorineural hearing loss, 3 of which were diagnosed bilateral profound hearing loss. Half of the children had other risk factors associated, the most frequent being exposure to ototoxics. Conclusion: The percentage of children diagnosed with sensorineural hearing loss who suffered hyperbilirubinemia at birth is higher than for the general population. Of those diagnosed none had levels of indirect bilirubin ≥ 20 mg/dl, only 47% had hyperbilirubinemia at birth as a risk factor and 53% had another auditory risk factor associated.
Keywords
Neonatal hyperbilirubinemia, Hearing loss, Neonatal screening.
Introduction
Permanent hearing loss in childhood is an important public health problem. Its prevalence, when considering only bilateral profund congenital sensorineural hearing loss (SNHL), is 1 in 1000 living newborns and 5 in 1000 when all degrees of hearing loss are considered [1]. Hearing loss produces not only permanent effects on oral language development but may also have implications in emotional and social development [2].
The criteria or risk factors associated with hearing loss were established in 1994 and were revised in 2000. Between 10 and 30% of new-borns meet one of these risk factors, hyperbilirubinemia at birth being one of them. Severe jaundice that requires blood transfusion has become a relatively rare situation today. About 60% of babies born on time and 80% of premature newborns will develop hyperbilirubinemia within the first week of life.
New-borns with hyperbilirubinemia represent 2.30% of the total newborn population. Hyperbilirubinemia at birth is a risk factor associated with hearing loss. It is usually associated with other factors, which might have synergistic effects on hearing, so the risk of hearing loss is substantially higher than in children not affected by it.
Early detection and treatment of these problems will largely determine the quality of life of these children in the future, so regular monitoring of certain aspects is necessary, including an assessment of hearing abilities [3].
Therefore, the aim of this paper is to quantify the incidence of hyperbilirubinemia at birth as a risk factor for SNHL in children born in the of Insular Maternal and Child University Hospital Complex, in the period 2007-2013, included in the Program for Early Detection of Infant Hearing Loss.
Materials and Methods
This is a retrospective study of 796 newborns that were diagnosed perinatal hyperbilirubinemia as a risk factor and were included in the Program of Early Detection of Hearing Loss in Children.
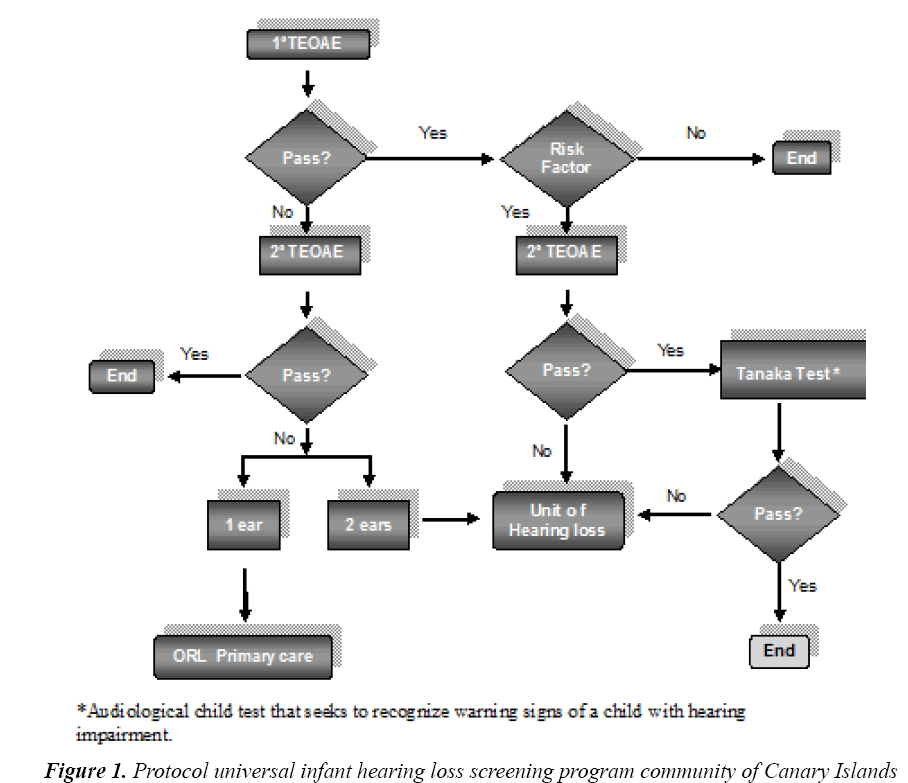
In the Canary Islands this program is based on a universal population screening and is divided in two phases (Figure 1) [4].
The first checkup is performed during the first 48 h of life, making the most of the hospitalization period of the mother. The chosen technique is the detection of otoacoustic emissions using portable and automatic devices (ScreenTA Echo-Plus). All infants were referred to the second phase. In this phase, the technique used is the detection of otoacoustic emissions using Intelligent Hearing and Interacoustic systems.
If Transient-Evoked Otoacoustic Emissions (TEOAE) were absent in both ears, they were referred to the Hearing Loss Unit of the ENT department for diagnosis and followup using Brainstem Auditory Evoked Potentials (ABR).
For statistical data processing SPSS 21.0 was used in its Windows version. To study possible associations between categorical variables, the Fisher's exact test (p<0.05) or p-value obtained by the Pearson chi-square test (p<0.001) were used.
The Ethics Committee on Clinical Trials of the Insular Maternal and Child University Hospital Complex approved the execution of this study.
Results
A total of 796 infants were studied during the period starting in January 1, 2007 until December 31, 2013. All had hyperbilirubinemia as main risk factor. Of these, 475 (59.67%) were boys and 321 were (40.33%) girls.
Table 1 shows the descriptive statistics of the distribution of risk factors by sex.
| Boy | Girl | Total | ||||
|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | |
| Only Hb | 255 | 32.04 | 188 | 23.61 | 443 | 55.65 |
| Only Ototoxic | 113 | 14.20 | 65 | 8.16 | 178 | 22.36 |
| Only very low weight (VLW) | 10 | 1.26 | 8 | 1.01 | 18 | 2.27 |
| Only others | 18 | 2.26 | 11 | 1.37 | 29 | 3.63 |
| Hyperbilirubinemia+ototoxics+very low weight+others | 79 | 9.93 | 49 | 6.16 | 128 | 16.09 |
| Total | 475 | 59.69 | 321 | 40.31 | 796 | 100.00 |
Table 1: Distribution of risk factors by gender
In the first phase of the Early Detection of Children's Hearing loss, OEAPT were negative in 16.54% of newborns, while in the second phase, OEAPT were absent in 49.05%. 185 newborns were referred for ABR, 116 boys (14.57%) and 69 girls (8.67%). A total of 93 children attended the ABR evaluation, 54 (29.19%) boys and 39 (21.08%) girls.
In relation to the distribution of risk factors for hearing loss indicated by ABR results, of the 92 newborns who attended this test, those who showed only hyperbilirubinemia at birth as a risk factor are divided into two groups: 14 with hearing loss and 31 with normal hearing (Table 2).
| Hearing Loss | Total | ||
|---|---|---|---|
| No | Yes | ||
| Only Hyperbilirubinemia | 31 | 14 | 45 |
| Only Ototoxic | 6 | 8 | 14 |
| Only very low weight | 0 | 2 | 2 |
| Only others | 1 | 1 | 2 |
| Hyperbilirubinemia+ototoxics+very low weight+others | 19 | 10 | 29 |
| Total | 57 | 35 | 92 |
Table 2: Distribution of risk factor by hearing loss as indicated by ABR
The distribution of the type of hearing loss for right/left ear determined by ABRs is seen in Table 3. Of the 92 children, 4 had left ear unilateral CHL; 13 had bilateral CHL, left ear CHL and right ear SNHL and 1 had right ear unilateral CHL. 10 children also had bilateral SNHL, 1 had right ear unilateral SNHL, 1 had left ear SNHL and 3 had right ear CHL and left ear SNHL.
| PEATC Right Ear |
Total | |||||
|---|---|---|---|---|---|---|
| Normal | CHL | SNHL | Absent | |||
| ABR Left Ear |
Normal | 57 | 1 | 1 | 0 | 59 |
| CHL | 4 | 13 | 2 | 0 | 19 | |
| SNHL | 1 | 3 | 10 | 0 | 14 | |
| Absent | 0 | 0 | 0 | 93 | 93 | |
| Total | 62 | 17 | 13 | 93 | 185 | |
Table 3: Distribution of hearing loss by right/left ear as indicated by ABR
Table 4 shows the distribution of the values of total bilirubin in the blood as a function of weeks of gestation and sex, while the study of the association between transfusion and sex is shown in Table 5.
| SNHL Mild | SNHL Moderate | SNHL Severe | SNHL Profund | |||||
|---|---|---|---|---|---|---|---|---|
| Unilat | Bilat | Unilat | Bilat | Unilat | Bilat | Unilat | Bilat | |
| Only Hyperbilirubinemia | 2 | 1 | - | 2 | 1 | - | 5 | 3 |
| Hyperbilirubinemia+others | 9 | 2 | 2 | 6 | 2 | - | - | - |
| Total | 14 | 10 | 3 | 8 | ||||
Table 4: Distribution of SNHL
| Preterm (<37 weeks) |
Term (>37 weeks) |
||||||
|---|---|---|---|---|---|---|---|
| Gender | Values of BT (mg/dl) | Count | % | Count | % | Total | Total % |
| Boy | 5 to 13.99 mg/dl | 124 | 15.58 | 42 | 5.27 | 166 | 20.85 |
| 14 á 19.99 | 115 | 14.45 | 130 | 16.33 | 245 | 30.78 | |
| ≥ 20 | 19 | 2.39 | 45 | 5.65 | 64 | 8.04 | |
| Girl | 5 to 13.99 mg/dl | 83 | 10.43 | 32 | 4.02 | 115 | 14.45 |
| 14 to 19.99 | 73 | 9.17 | 80 | 10.05 | 153 | 19.22 | |
| ≥ 20 | 13 | 1.63 | 40 | 5.03 | 53 | 6.66 | |
| Total | 427 | 53.65 | 369 | 46.35 | 796 | 100.00 | |
Table 5: Total bilirubinemia blood values relation with week of gestation and gender
The study of the association between presence of marked hearing loss using ABR, the values of total bilirubin in blood and the weeks of gestation showed that 11 (45.83%) patients had levels of total bilirubin in blood between 14 and 19.99 mg/dl, less than 37 weeks of gestation and 5 (45.45%) patients had the same values of bilirubin but more than 37 weeks of gestation. All had hearing loss. A total of 4 (36.36%) children with values of total bilirubin greater than 20 mg/dl and more than 37 weeks gestation were also diagnosed with hearing loss (p<0.001) Table 6.
| Exchange transfusion | |||||
|---|---|---|---|---|---|
| Gender | Yes | % | No | % | p-value* |
| Boy | 11 | 61.11 | 464 | 59.64 | 0.552 |
| Girl | 7 | 38.89 | 314 | 40.36 | |
| Total | 18 | 2.27 | 778 | 97.73 | 100 % |
| *p-value obtained by Fisher test | |||||
Table 6: Relation between exchange transfusion and gender
The percentage of children studied, diagnosed with profound SNHL, among 796 infants with hyperbilirubinemia is 2.135%. This value is above the expected percentage of hearing loss for the general population (p<0.001), with data being statistically significant (Table 7).
| Bilirubin mg/dl | |||||||
|---|---|---|---|---|---|---|---|
| ≥ 5<13.99 | ≥ 14 ≤ 19.99 | ≥ 20 | |||||
| Hearing Loss | Week of gestation | Count | % | Count | % | Count | % |
| Yes | Preterm (<37 weeks) |
13 | 54,17 | 11 | 45,83 | 0 | ,00 |
| Term (>37 weeks) |
2 | 18,18 | 5 | 45,45 | 4 | 36,36 | |
| No | Preterm (<37 weeks) |
23 | 60,53 | 13 | 34,21 | 2 | 5,26 |
| Term (>37 weeks) |
2 | 10,53 | 10 | 52,63 | 7 | 36,84 | |
| Total | 40 | 43.47 | 39 | 42.40 | 13 | 14.13 | |
| *p-value obtained by Pearson Chi-square Test | |||||||
Table 7: Asociation between total bilirubin in blood, week of gestation and presence of hearing loss indicated by ABR (p<0.001*)
Discussion
It has been shown that the only effective strategy for early intervention and treatment of hearing loss in children is early detection, and that this strategy must be universal [5-8].
Severe hyperbilirubinemia that required transfusion has become a relatively rare situation today; however, moderate hyperbilirubinemia is seen in approximately 60% of babies born on time and 80% of premature infants. It is accepted that levels above 20 mg/dl of bilirubin increase the risk of neurological damage in babies born on time, but also that premature ones can suffer consequences with much smaller numbers. There is scientific evidence that demonstrates that sensorineural impairment appears as a result of increased indirect bilirubin in blood, but it has not been demonstrated why there is not a proportional relationship between these values. This effect is attributed to the interaction with other risk factors present in the neonate that may potentiate the effect of hyperbilirubinemia (prematurity, low birth weight, hypoxia, metabolic acidosis or perinatal infections) [9-15].
Clinically bilirubin toxicity may be reversible and not give clinical symptoms or they may be very subtle and appear late. In a study by Suresh et al., no cases of hearing loss were found despite prolonged exposure to high levels of bilirubin >20 mg/dL in the majority of patients evaluated, which led them to indicate that bilirubin is not as toxic to the auditory system as was assumed [16]. Our results match with those of their sample. Of the 17 children diagnosed with SNHL, none had values ≥ 20 mg/dl of bilirubin.
Very low birth weight and prematurity are often concomitant, being difficult to completely separate the factors as being linked to one or the other. These children are a high-risk population for SNHL. In these patients bilirubin levels above 14 mg/dL mean a 30% risk of having hearing loss [17,18].
In our sample, we studied the association between gestational week and the presence of hearing loss. Of the 35 (38.04%) children diagnosed with hearing loss, 24 (68.57%) were premature newborns (<37 weeks) and 11 (31.43%) were on born on time (>37 weeks).
The Joint Committee on Infant Hearing (JCIH) and the Commission for the Early Detection of Infant Hearing Loss (CODEPEH) define Hyperbilirubinemia as a risk factor for SNHL as: “hyperbilirubinemia that requires blood transfusion”. This definition has a specificity that is clinically unclear, because it is very ambiguous in that it fails to define the value of bilirubin required for such transfusions [19-21].
In our sample, there were 18 blood transfusions with blood bilirubin levels >14 mg/dL. Of these, none suffered severe SNHL. This is in agreement with a study from Wong et al. [22] where from a sample of 99 infants with hyperbilirubinemia, they described three cases of blood transfusion with unaltered ABR results.
Ohl et al. [23] found that the association of two or more risk factors significantly increases bilateral hearing loss. In our sample of 35 new-borns diagnosed with SNHL, 8 had the sole risk factor of hyperbilirubinemia, of which 3 (8.57%) had a diagnosis of bilateral SNHL and 5 (14.28%) had unilateral SNHL. 27 newborns presented an association between two to four risk factors, the most common association being ototoxic medication and very low weight at birth.
The rate of sensorineural hearing loss among children with associated risk factors in our sample is 2.13%. This data matches with that from the study by Ptok [24], Erenberg et al. [25] where the rate of SNHL among children who have some associated risk factor is said to be 1-2%.
In our sample of 3 newborns diagnosed with profound SNHL, only 1 had the sole risk factor for hyperbilirubinemia, the other two also presented the association of exposure to ototoxic medication and very low weight at birth.
Conclusion
47% of children with HNS had only Hyperbilirubinemia at birth as risk factor for hearing loss, while the remaining 53% had another risk factor associated. Of those children diagnosed with profound SNHL, only one had neonatal hyperbilirubinemia as the sole risk factor.
None of the children diagnosed with HNS required blood transfusion as treatment to their hyperbilirubinemia.
References
- Manrique M, Morera C, Moro M. Early detection of childhood hearing loss in high-risk new-borns An Esp Pediatr 1994; 40: 11-45.
- Marco J, Almenar A, Alzina V, et al. Quality control of an early detection, diagnosis and early intervention program for deafness in newborn. Official document of the Early Detection Comission of Deafness in Newborn (CODEPEH).Acta Otorrinolaringol Esp 2004; 55: 103-106.
- American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007; 120: 898-921.
- Borkoski Barreiro SA, Falcón González JC, Bueno Yanes J, et al. Results of an early hearing detection program. Acta Otorrinolaringol Esp 2013; 64: 92-96.
- Yoshinaga Itano A, Sedey AL, et al. Language of early and later identified children with hearing loss. Pediatrics 1998; 102: 1161-1171.
- Cabra J, Moñux A, Grijalva M, et al. Implantation of a program for the early detection of neonatal hearing loss. Acta Otorrinolaringol Esp 2001; 52: 668-673.
- Bailey H, Bower C, Krishnawamy J, Coates H. New-born hearing screening in Western Australia. Med J Aust 2002; 177: 180-185.
- Levitt H, Mc Garr NS, Geffner D. Development of language and communication skills in hearing impaired children. ASHA Monographs 1987; 26: 1-168.
- Borkoski Barreiro SA, Falcón González JC, Limiñana Cañal JM, et al. Evaluation of very low birth weight (≤ 1,500 g) as a risk indicator for sensorineural hearing loss. Acta Otorrinolaringol Esp 2013; 64: 403-408.
- Pruszewicz A, Pospiech I. Low birth weight as a risk factor of hearing loss. Scand Audiol Suppl 2001; 52: 194-196.
- Shapiro SM. Definition of the clinical spectrum of kernicterus and bilirubin-induced neurologic dysfunction (BIND). J Perinatol 2005; 25: 54-59.
- Yoshikawa S, Ikeda K, Kudo T, et al. The effects of hypoxia, premature birth, infection, ototoxic drugs, circulatory system and congenital disease on neonatal hearing loss. Auris Nasus Larynx 2004; 31: 361-368.
- Wennberg R, Gospe SM Jr, Rhine WD, et al. Brainstem bilirubin toxicity may primate be promoted and reversed by modulating PCO2. Pediatr Res 1993; 34: 6-9.
- Campistol J, Galvez H, Cazorla AG, et al. Neurological dysfunction induced by bilirubin. Neurologia 2012; 27: 202-11.
- Shapiro SM. Bilirubin toxicity in the developing nervous system. Pediatr Neurol 2003; 29: 410-421.
- Suresh G, Lucey JF. Lack of deafness in Crigler-Najjar syndrome type 1: A patient survey. Pediatrics 1997; 100: E9.
- Martines F, Salvago P, Bentivegna D, et al. Audiologic profile of infants at risk: Experience of a Western Siicily tertiary care centre. Int J Pediatr Otorhinolaryngol 2012; 76: 1285-1291.
- De Vries L, Lary S, Dubowitz L. Relationship of serum bilirubin levels to ototoxicity and deafness in high-risk low-birth-weight infants. Pediatrics 1985; 76: 351-354.
- Martínez JC. The real problem of newborn jaundice: New guidelines from the American Academy of Pediatrics. Archivos Argentinos de Pediatría 2005; 103: 524-532.
- Trinidad Ramos G, de Aguilar VA, Jaúdenes Casaubón C, et al. Early hearing detection and intervention: 2010 CODEPEH recommendation. Acta Otorrinolaringol Esp 2010; 61: 69-77.
- Nuñez Batalla F, Carro Fernández P, Antuña León ME, González Tulls T. Incidence of hypoacusia secondary to hyperbilirubinaemia in a universal neonatal auditory screening programme based on otoacoustic emissions and evoked auditory potentials. Acta Otorrinolaringol Esp 2008; 59: 108-113.
- Wong V, Chen WX, Wong KY. Short-and long-term outcome of severe neonatal non hemolytic hyperbilirubinemia. J Child Neurol 2006; 21: 309-315.
- Ohl C, Dornier L, Czajka C, et al. New-born hearing screening on infants at risk. Int J Pediatr Otorhinolaryngol 2009; 73: 1691-1695.
- Ptok M. Early detection of hearing impairment in new-borns and infants. Dtsch Arztebl Int 2011; 108: 426-431.
- Erenberg A, Lemons J, Sia C, et al. Newborn and infant hearing loss: detection and intervention. American Academy of Pediatrics. Task Force on Newborn and Infant Hearing, 1998-1999. Pediatrics 1999; 103: 527-530.