Case Report - Journal of Oral Medicine and Surgery (2025) Volume 8, Issue 1
Mucous extravasation cysts (Ranulae).
Mahesha Imbulana*
Department of Dental Surgery, National Dental Hospital, Colombo, Sri Lanka
*Corresponding Author:
Mahesha Imbulana Department of Dental Surgery, National Dental Hospital, Colombo, Sri Lanka E-mail: E-mail: imbulanai@gmail.com
Received: 17-Jul-2023, Manuscript No. AAOMT-23-106598; Editor assigned: 19-Jul-2023, AAOMT-23-106598 (PQ); Reviewed: 02-Aug-2023, QC No. AAOMT-23-106598; Revised: 04-Jan-2025, Manuscript No. AAOMT-23-106598 (R); Published: 11-Jan-2025, DOI:10.35841/aaomt.8.1.171
Citation: Imbulana M. Mucous extravasation cysts (Ranulae). J Oral Med Surg. 2025;8(1):1-3.
Abstract
Mucous extravasation cysts, commonly referred to as ranulae, are benign lesions originating from the salivary glands. These cysts typically manifest as painless, fluctuant swellings in the floor of the mouth, often presenting as a result of trauma or obstruction of the salivary ducts. This review aims to provide a comprehensive overview of mucous extravasation cysts, including their etiology, clinical presentation, diagnostic approach, and management strategies. Various treatment modalities, ranging from conservative measures to surgical intervention, are discussed, with an emphasis on individualized patient care. Understanding the pathogenesis and appropriate management of ranulae is essential for clinicians to ensure optimal outcomes and patient satisfaction.
Keywords
Ranulae, Salivary glands, Etiology, Surgical intervention, Cysts
Introduction
The most common type of salivary and soft tissue cysts are the extravasation mucoceles of minor salivary glands. It is not a true cyst as it has no epithelial lining. Retention cysts are the less common mucoceles mainly affect the minor salivary glands particularly at the lip. However, 44% to 79% of mucoceles occur on the lower lip [1]. The accumulation of mucus into the surrounding connective tissue forms a pseudocyst that lacks of epithelial lining [2]. The analysis of the saliva reveals a high protein and amylase concentration consistent with secretions from the mucinous acini in the sublingual gland. The high protein content may produce a very intense inflammatory reaction and mediate pseudocyst formation [3].
The long term ranula derived from Latin word ‘Rana tigerina ‘i.e., frog belly. The term ranula is used for mucoceles which is asymptomatic extravasation cystic lesion arising from the floor of the mouth in association with ducts of submandibular or sublingual salivary glands. The ranula usually present as unilateral swelling of the floor of the mouth.
There are two types of ranula. They are classified as:
• Superficial ranula.
• Cervical/deep (plunging ranula).
Superficial ranulae are developed as a retention or extravasation phenomenon associated with trauma to one of or more of the numerous excretory ducts of the sublingual salivary gland and lies above mylohyoid muscle. Plunging or cervical ranulae occur deeply in to the neck.
Ranula can be recognized as a bluish, fluctuant swelling in the floor of the mouth and does not pose a diagnostic difficulty. If it is large, it tends to cause medial superior deviation of the tongue. On some occasions plunging ranula can occur as extra oral swelling without an associated intraoral swelling. Such lesions must be differentiated clinically from thyroglossal cyst, dermoid cyst, lymphangioma, lipoma, hemangioma, thyroid gland, abscess or tumour.
Many methods of treatments for ranulae have been described in literature, including excision of ranula only, excision of ranula and ipsilateral sublingual gland, marsupialization and cryosurgery. Besides surgical management, CO2 laser has been used to vaporize ranulae [4]. In rare cases radiation therapy is an alternative.
Case Presentation
39 years old otherwise healthy female patient was referred from outdoor patient department of national dental hospital, Colombo, Sri Lanka to the oral and maxillofacial surgery unit of national dental hospital, Colombo, Sri Lanka, due to the complaint of painless recurrent swelling on the left side of the floor of the mouth for more than one-year duration. Time to time it appeared and ruptured several times.
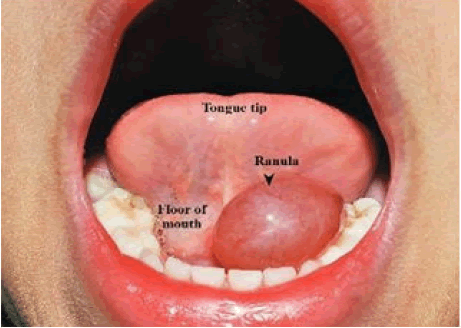
On general examination, she was fit and healthy-looking patient with no allergies for any foods and medicines (Figure 1).
On extra oral examination, no palpable lymph nodes detected in head and neck region. There was no obvious swelling on the face and no facial asymmetry detected. Intra oral examination revealed soft transparent swelling on left side of the floor of the mouth associated with raised floor. It was oval in shape with 3 cm × 1.5 cm in size and bluish in color. Transillumination was present. On palpation swelling was soft in consistency, nontender and fluctuant. There were no secondary changes like fistula, ulceration, infection or discharge. In special investigation, based on history and clinical presentation lower standard occlusal radiograph was taken. Radiograph revealed no evidence of obstruction or abnormality.
Tentative diagnosis of ranula was made based upon history and clinical examination.
Treatment plan
• Improvement of oral hygiene by doing full mouth scaling and polishing.
• Marsupialization of the ranula under local anesthesia.
Treatment
Oral care has been given to the patient. Surgical procedure under local anesthesia was explained to the patient. After taking the written consent from the patient local anesthesia was infiltrated around the lesion after identifying the margins of the lesion.
Marsupialization of the cystic cavity was done. Contents were evacuated and the cavity was made continuous with oral epithelium. After the surgery patient was given antibiotics and analgesics therapy for 5 days.
Results and Discussion
Ranulae occur from extravasation of mucus after trauma to the sublingual salivary gland or obstruction of the ducts [5]. Ranula can present in any age of someone’s life. It has been reported from 2 to 61 years of age with slight female preponderance. The etiology of ranula is unknown, but it hasbeen described in association with congenital anomalies, trauma and disease of sublingual salivary gland [6].
Ranula can be classified into two groups, simple (intraoral) and the plunging (cervical) types. Simple ranula is much more common than plunging type. A simple ranula represents a localized collection of mucus within the floor of the mouth. In plunging ranula, the mucus collection is in the submandibular and submental space of the neck with or without an associated intraoral collection [7].
The possibility of a plunging ranula should be considered in a patient with a painless cervical swelling that gradually increases in size, particularly if there is a history of oral trauma, including dental or other oral surgical procedures.
The pathophysiology involved in extravasation is hypertension in the duct due to obstruction leading to acinar rupture in the salivary gland.
Conclusion
In conclusion, mucous extravasation cysts, or ranulae, represent a common entity encountered in clinical practice, particularly by oral and maxillofacial surgeons and otolaryngologists. Although typically benign, these cysts can cause discomfort and functional impairment, necessitating appropriate management. The diagnosis of ranulae relies on a thorough clinical evaluation supplemented by imaging studies, such as ultrasound and magnetic resonance imaging. Treatment options include observation, needle aspiration, marsupialization, and excisional procedures, with the choice depending on the size, location, and symptoms associated with the lesion. The selection of the most suitable approach should be tailored to each patient, taking into account their preferences and the risk of recurrence. Further research is warranted to explore novel therapeutic strategies and improve the understanding of the underlying mechanisms of mucous extravasation cysts. By advancing our knowledge and refining treatment algorithms, clinicians can effectively manage ranulae and optimize patient outcomes.
References
- White DA, Leonard MC. Acute stroke with high-dose intravenous immune globulin. Am J Health Syst Pharm. 2007;64(15):1611-4.
[Crossref] [Google Scholar] [PubMed]
- Bronstein SL. Postsurgical TMJ arthrography. J Craniomandibular Pract. 1984;2(2):165-71.
[Crossref] [Google Scholar] [PubMed]
- Zhi K, Wen Y, Ren W, et al. Management of infant ranula. Int J Pediatr Otorhinolaryngol. 2008;72(6):823-6.
[Crossref] [Google Scholar] [PubMed]
- Mintz GS, Pichard AD, Kovach JA, et al. Impact of preintervention intravascular ultrasound imaging on transcatheter treatment strategies in coronary artery disease. Am J Cardiol. 1994;73(7):423-30.
[Crossref] [Google Scholar] [PubMed]
- Catone GA. Sublingual gland mucus-escape phenomenon treatment by excision of sublingual gland. J Oral Surg. 1969;27(10):774-86.
[Google Scholar] [PubMed]
- Davison MJ, Morton RP, McIvor NP. Plunging ranula: Clinical observations. Head Neck. 1998;20(1):63-8.
[Crossref] [Google Scholar] [PubMed]
- Zhao YF, Jia Y, Chen XM, et al. Clinical review of 580 ranulas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(3):281-7.
[Google Scholar] [PubMed]