Case Report - Otolaryngology Online Journal (2016) Volume 6, Issue 3
Metastasis of Renal Cell Carcinoma to the Head and Neck Region
- *Corresponding Author:
- Guler Berkiten
Department of Otorhinolaryngology-Head and Neck Surgery, Okmeydani Training and Reseach Hospital, Istanbul, Turkey
Tel: 905057278724
E-mail: gulerberkiten@gmail.com
Received date: May 07, 2016; Accepted date: July 13, 2016; Published date: July 18, 2016
Abstract
Renal cell carcinoma is the most common malignant tumor of the kidney. Thirty percent of the patients have distant organ metastasis at diagnosis. The lungs, bones, liver, lymph nodes and mediastinal metastasis are the most common regions. Metastasis is very rare in the head and neck region. In our study, the diagnosis and the treatment of two patients after nephrectomy due to renal cell carcinoma and other two patients with distant organ metastases at diagnosis, totally 4 patients were discussed with literature data.
Keywords
Renal cell carcinoma, Neoplasm, Metastasis
Introduct?on
Renal cell carcinoma (RCC) is the most common malignant tumor of the kidney and comprises 90-95% of renal tumors in adults. RCC metastasis hematogenously and lymphatically and 30 to 40% of patients are diagnosed with distant metastases. The lungs, bones, liver and brain are the most common regions of metastasis [1]. Metastasis to the head and neck region is very rare (less than 1%). 8-15% of all cases of metastasis in head and neck region are associated with RCC [2]. In our study, four patients were presented with metastasis of head and neck region and were discussed with literature data.
Case 1
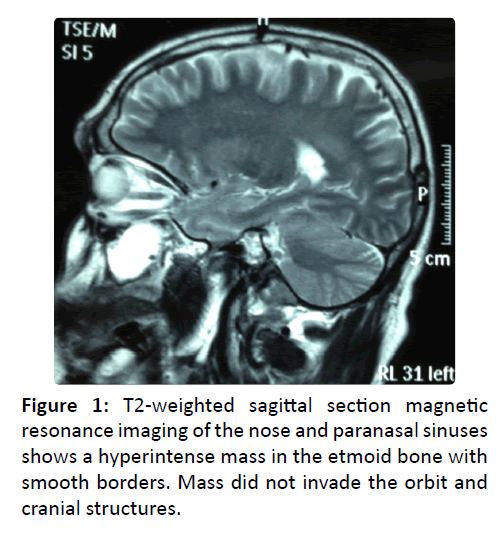
61-year-old male patient was admitted to our hospital because RCC and Positron Emission Tomography/ computed tomography (PET-CT) scan for metastasis showed increased fluorodeoxyglucose (FDG) uptake in the ethmoid sinuses. There was a non-polypoid, smooth, isolated mass in the left middle meatus and polypoid mass in the right meatus with rigid nasal endoscopy of the patient. There was not any pathology of nasal septum. Computed tomography of the paranasal sinuses (PNS CT) and magnetic resonance imaging (MRI) (Figure 1). had a soft tissue mass arising from the ethmoid cells. Biopsies of the masses were reported as the metastatic clear cell carcinoma in the left meatus and as the inflammatory polyp in the right meatus. The patient underwent left nephrectomy prior to endoscopic sinus surgery with general anesthesia. The patient's left ethmoid sinus histopathology was compatible with metastatic RCC. After palliative radiotherapy, there was not any pathology in 1-year follow-up.
Case 2
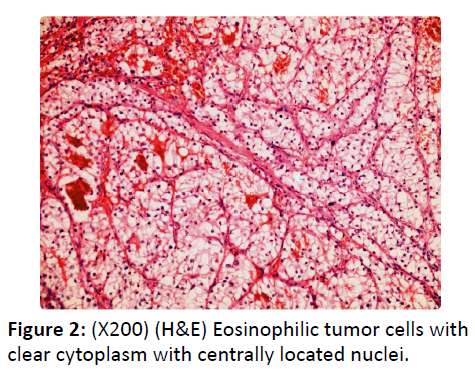
65-year-old female patient was admitted to our hospital because of an intranasal mass. The patient had left nasal obstruction, recurrent epistaxis and complaint of loss of smell for 3 months. In physical examination, there was 3 × 2.5 × 1.5 cm hemorrhagic and ulcerated bleeding polypoid mass filling the left nasal cavity from nasal vestibule. The patient had a history of colon carcinoma 15 years ago and left nephrectomy due to RCC 11 years ago. The patient had regular follow-up without any complaint. There was no invasion to the sinuses in the CT scan of PNS. Anterior nasal packing was needed due to bleeding during the biopsy. Histopathologic diagnosis was reported as RCC metastasis due to the earlier history of RCC. There was no other metastatic lesion in other systems and the primary region was free of the disease. The mass in the lateral nasal wall was excised in en bloc with tumor-free surgical margins endoscopically under general anesthesia and histopathological assessment after the surgery was reported to be compatible with preoperative pathology as RCC (Figure 2). After the interferon therapy, there was no recurrence in the 3-year follow-up of the patient.
Case 3
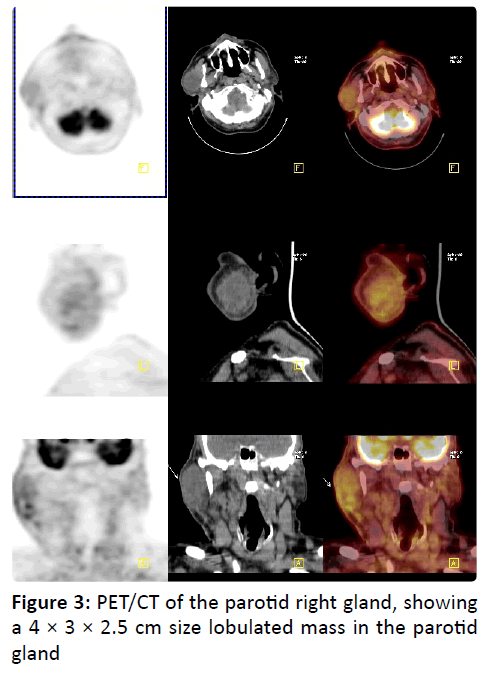
70 years old male patient was first admitted to our hospital because of growing lesion in the right parotid region. Any facial paresthesia and weakness, accompanied by dysphagia, snoring, otalgia, dysphagia, dyspnea, or unexplained weight loss was not available. The medical history of the patient had hypertension and right nephrectomy due to RCC 11 years ago. Physical examination revealed painless, soft, smooth 3 × 4 cm mass in the right parotid gland. In the contrast-enhanced neck CT, PET/CT (Figure 3) and MRI, 4 × 3 × 2.5 cm size lobulated mass in the right parotid gland was reported. As the result of fine needle aspiration biopsy (FNAB) of the lesion consistent with carcinoma infiltration, surgical excision was planned. Operation was terminated after biopsy was taken due to excessive bleeding. Immunohistochemical examination of neoplastic cells were positively stained with vimentin, CD10, EMA, LMWCK, S-100, Pan-CK, and were negatively stained with CK7, p63, HMWCK, CEA. Histopathology, RCC metastasis have been reported according to these findings. After receiving immunotherapy, lung and sacrum metastases developed in follow-up of the patients.
Case 4
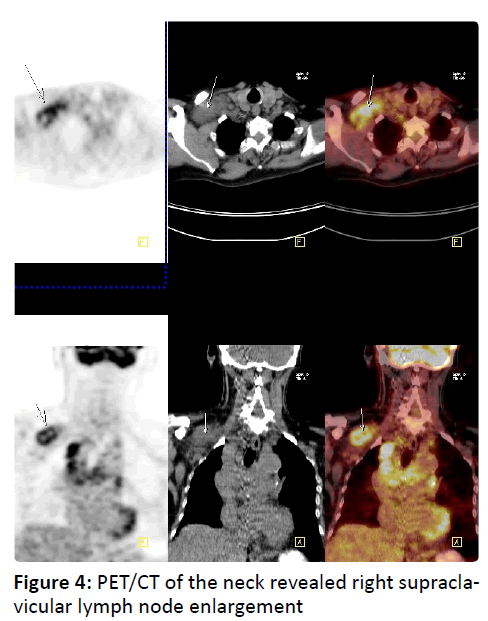
61-year-old male patient was admitted to our clinic because of growing mass in the right supraclavicular region of the neck. In the physical examination, there was 4 × 3 cm in size, smooth surface, painless fixed lesion in the right supraclavicular region. PET/CT of the neck revealed right supraclavicular lymph node enlargement (Figure 4). As the incisional biopsy was compatible with metastatic RCC, the patient was hospitalized planning operation.
Immunohistochemical examination of neoplastic cells were positively stained with pancytokeratin, AMACR, CK7, focally positive with CD10, negatively stained with thyroglobulin, TTF-1 and CK 20 and was reported to be compatible with metastatic RCC. The patient died within 2 months during radiotherapy and chemotherapy after the diagnosis of incidentally RCC metastases to the supraclavicular, vertebral metastasis, paraaortic and retroperitoneal.
Discussion
RCC are usually encountered in the sixth and seventh decades of life and are three times more common in men than women. Cigarette smoking, hypertension, and obesity are risk factors [3]. Clear cell is the most common type of tumor cells. Metastasis occurs approximately in 10% of RCC although primary tumor is not yet clinically evident. Approximately 20- 25% of patients have distant metastasis at the time of the diagnosis. During follow-up after treatment of the primary tumor, local recurrence or metastasis develops in 50% o f the patients [4,5]. RCC grows slowly and usually produce no symptoms until large sizes. Therefore, small and asymptomatic RCC are usually diagnosed incidentally when investigating other diseases with imaging techniques. Two of our patients were also diagnosed with distant metastases.
Metastases in the nose and paranasal sinuses are rare and maxillary sinus is the most commonly affected area. Kidneys, bronchi, gastrointestinal tract, and breast are the most common organs that metastasize to paranasal sinuses and almost 50% of these cases are RCC [6].
Epistaxis is the main complaint of 70% of the patients for RCC to the sinonasal region. Nasal congestion, loss of smell, pain, orbital signs, symptoms such as swelling and headache can also be seen [7,8]. It is difficult to differentiate primary sinonasal tract from metastatic lesions clinically or radiologically. Sinonasal metastases of RCC are characterized by severe bleeding. Biopsy of the lesion may not be diagnostic in all the time due to diffuse necrosis [9]. Bleeding complicated the biopsy in our patients.
Nasal cavity metastasis is rare in the literature [10]. reported nasal cavity metastasis in 76-year-old patient and palliative chemoradiation was planned.
Parotid gland metastasis is also rare in RCC. Patients are usually presented asymptomatic with unilateral parotid mass. Although accompanied by pain, pulsation, tinnitus, numbness are reported in the literature, they are very rare. FNAB is not diagnostic and has false positive feature. FNAB can be diagnostic in clear cell tumors but immunohistochemical staining is needed to make the differential diagnosis of the other clear cell tumors of the parotid gland (clear cell myoepithelial carcinoma, epithelialmyoepithelial clear cell carcinoma, clear cell acinic cell carcinoma, clear cell adenocarcinoma of salivary glands and hyalinizing clear cell carcinoma) [11]. RCC is stained positive with CD10 and vimentin [12]. Appropriate treatment of patients with metastatic carcinoma of parotid gland is a multidisciplinary approach. In parotid gland metastases, the choise of treatment is the excision of the tumor while preserving the facial nerve if possible.
Despite the fact that RCC often can metastases, cervical or supraclavicular lymph node metastasis is rare. Only 1% of patients with metastatic head and neck region are presented with a solitary mass in the cervical metastatic [13]. In this case, the patient admitted to our clinic with a complaint of supraclavicular mass without having a diagnosis of RCC.
The prognosis is extremely poor in the metastatic RCC and the a verage survival is 7-11 months [14]. However, RCC biological behavior is variable and prognosis depends on the clinical, radiological, serological and histological factors of RCC. Tumor stage and grade, presence of vascular invasion and capsular infiltration, microvessel density and tumor necrosis are important prognostic factors [15]. Among the factors affecting the prognosis, the presence of occult metastases at diagnosis, especially positive lymph nodes or invasion of the renal veins, plays a particular major role [16]. 5-year survival of the RCC is 60-75% after nephrectomy. The survival rate decreases to 35% in the patients with single metastasis although metastases are treated radically. As the number of metastases increase, this rate varies between 0-7%. The regional metastases developed after the treatment of the primary tumor have a better prognosis than the metastasis at the time of the diagnosis. 5- year survival is 50% in these patients [17].
Although surgical resection of metastases in head and neck region is very important in order to survive, the surgical treatment of metastases is generally palliative. RCC are known as radioresistant tumor, but radiotherapy plays an important role in the control of symptoms associated with pain and local compression [18]. In addition, high-dose radiation therapy can be used to facilitate
the surgical excision to reduce the blood supply to the primary tumor [17]. The other alternative for the treatment are hormonal therapy, immunotherapy and chemotherapy. However, the results obtained from the studies with immunotherapy are more promising. Interferon-α (IFN-α) and interleukin-2 (IL- 2) are used in the recent years [19]. As renal cell tumors are highly vascular, drugs that inhibit angiogenesis and tumor vascularization are promising for better treatment results [20].
Renal cell carcinoma cases may refer to the physician with many different clinical presentations and different prognosis. The diagnosis of patients with uncommon symptoms and the clinical course of the RCC will be effective in reducing mortality and morbidity.
References
- Ritchie AW, Chisholm GD (1983) The natural history of renal carcinoma. Semin Oncol 10:390-400.
- Pritchyk KM, Schiff BA, Newkirk KA (2002) Metastatic renal cell carcinoma to the head and neck. Laryngoscope 112: 1598-601.
- Boggess MA, Hester TO, Archer SM (1996) Renal clear cell carcinoma appearing as a left neck mass. Ear Nose Throat J 75:620-622.
- Golimbu M, Joshi P, Sperber A, Tessler A, Al-Askari S, et al. (1986) Renal cell carcinoma: survival and prognostic factors. Urology 27:291-301.
- Motzer RJ, Bander NH, Nanus DM (1996) Renal-cell carcinoma. N Engl J Med 335:865-875.
- Tariq M, Gluckman P, Thebe P (1998) Metastatic testicular teratoma of the nasal cavity: a rare cause of severe intractable epistaxis. J Laryngol Otol 112:1078-1081.
- Maheshwari GK, Baboo HA, Patel MH, Usha G (2003) Metastatic renal cell carcinoma involving ethmoid sinus at presentation. J Postgrad Med49:96-97.
- Atar Y, Topaloglu I, Ozcan D (2013) Metastatic renal cell carcinoma in the nasopharynx. Indian J Pathol Microbiol 56:40-42.
- Torres MB, Solano R, Baro RJG, Bonilla PR (2006) Maxillary sinus metastasis of renal cell carcinoma. Actas Urol Esp 30: 954-957.
- Terada T (2012) Renal cell carcinoma metastatic to the nasal cavity. Int J Clin Exp Pathol 5:588-591.
- Seijas BP, Franco FL, Sastre RM, Garcia AA, Lopez-Cedrun CJL (2005) Metastatic renal cell carcinoma presenting as a parotid tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99:554-557.
- Andreadis D, Nomikos A, Barbatis C (2007) Metastatic renal clear cell carcinoma in the parotid gland: a study of immunohistochemical profile and cell adhesion molecules (CAMs) expression in two cases. Pathol Oncol Res13:161-165.
- Pompeo AC, Kanashiro H, Silva MN (2005) Renal cell carcinoma presenting as a cervical mass. Int Braz J Urol 31:151-152.
- Shariat SF, Karam JA, Karakiewicz PI (2009) Words of wisdom. Re: Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. Eur Urol55:250-252.
- Rabinovitch RA, Zelefsky MJ, Gaynor JJ, Fuks Z (1994) Patterns of failure following surgical resection of renal cell carcinoma: implications for adjuvant local and systemic therapy. J Clin Oncol 12: 206-212.
- Negrier S, Escudier B, Lasset C (1998) Recombinant human interleukin2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma. Groupe Francais d\'Immunotherapie. N Engl J Med338:127-128.
- Nason R, Carrau RL (2004) Metastatic renal cell carcinoma to the nasal cavity. Am J Otolaryngol 25:54–57.
- Ather MH, Masood N, Siddiqui T (2010) Current management of advanced and metastatic renal cell carcinoma. Urol J 7: 1-9.
- Jacobsen J, Grankvist K, Rasmuson T, Ljungberg B (2006) Different isoform patterns for vascular endothelial growth factor between clear cell and papillary renal cell carcinoma. BJU Int 97:1102-1108.
- Choi YR, Han HS, Lee OJ (2012) Metastatic renal cell carcinoma in a supraclavicular lymph node with no known primary: a case report. Cancer Res Treat 44:215-218.