Research Article - Biomedical Research (2017) Volume 28, Issue 7
Meibomian gland Dropout in Chinese cataract patients
Jinling Ge1,2#, Lian Duan3#, Chaoqing Wang2, Xiuhua Zheng2 and Lihua Wang1*
1Department of Ophthalmology, Provincial Hospital, Shandong University, Jinan, Shandong, PR China
2Department of Ophthalmology, Jinan Mingshui Eye Hospital, Zhangqiu, Shandong, PR China
3Department of Ophthalmology, Qianfoshan Hospital, Shandong University, Jinan Shandong, PR China
#These authors contributed equally
- *Corresponding Author:
- Lihua Wang
Department of Opthalmology
provincial Hospital
Shandong University, PR China
Accepted on December 06, 2016
Abstract
To examine the morphological changes in the meibomian gland (MG) of eyes of Chinese cataract patients using a keratography 5M and to assess their relations with meibomian dropout, signs, and tearfilm function. A cross-sectional observation study of subjects (N=99) unmatched for sex and without a significant difference in age was performed. Testing included administration of Ocular Surface Disease Index (OSDI) questionnaire, followed by Keratograph 5M measurements of the noninvasive tear breakup time (NIBUT), tear meniscus height (TMH), and the morphology of the MG (meibography). Partial or complete loss of the MG was scored for each eyelid from grade 0 (no loss of MG) through grade 3 (loss of >2/3 of the whole gland area). The average OSDI score was 27.80 ± 10.22, the average NIBUT-first was 6.34 ± 4.93 s, NIBUT-average was 8.42 ± 5.51 s, and the average TMH was 0.20 ± 0.11 mm (normal: >0.20 m). In addition, the mean MG photographic score (meiboscore) was 3.07 ± 1.39. The meiboscore demonstrated identical statistically significant Kendall’s correlations with OSDI scores (r=0.431, P=0.000) and no statistically significant correlations with NTBUT-first, NTBUT-average and TMH. The results suggest a large proportion of meibomian dropout cases in Chinese cataract patients. The meiboscore tested by Keratograph 5M and OSDI score demonstrated a statistically significant correlation. Meibography and OSDI questionnaire might be recommended as a routine test before cataract surgery.
Keywords
Chinese cataract patients, Meibography, Keratograpy 5M, OSDI, Correlation, Dry eye.
Introduction
Cataract surgery is one of the most successful surgical interventions performed today. In spite of excellent postoperative distance visual acuity obtained for most patients, some patients are distracted and dissatisfied because of dry-eye syndrome. However, for the patients with extensive meibomian gland dysfunction (MGD), only a lubricant supplement is inappropriate during the anti-dry eye treatment [1-3]. Thus, more attention should be paid to those cataract patients with MG problems instead of concern only about tear-film function.
The meibomian glands, which synthesize and secrete lipids for the superficial tear film layer, play an important role in maintaining a healthy ocular surface through reducing tear evaporation. MG dysfunction (MGD) was defined as the presence of an obstruction of the meibomian orifices or the absence of a gland structure, or both of these fingdings [4,5]. MG “dropout” or atrophy refers to the complete loss of acinar tissue when detected by meibography [6-8]. Previous studies have indicated that MG dropout increases with age in a normal population, not necessarily in response to the presence of obstructive MGD [6,9]. However, it has also been demonstrated that extensive dropout is associated with increasing evaporation of water from the eye [10]. Thus, it is necessary to study the correlation between MG dropout and dry eye disease in a large population to better understand their association. It is also very important to determine the condition of the MG in patients with cataract, particularly in those without dry eye or with mild symptoms before cataract surgery.
The Keratograph 5M is a noncontact, Placido ring-based corneal topographer that equipped with an infrared light (IR) illumination system (880 nm) for pupillometry measurements and with an onboard camera for shooting both video and still images. It is easy to operate and accurately shows the number and morphology of MG. This system allows for a shorter examination time without much discomfort and is a good inspection method for assessing MG function [11]. The application of MG photography to assessing changes in the structure of the MG will benefit ophthalmologists by providing a better understanding of MG disease.
In this study, we used the Keratograph 5M to investigated the morphological changes of the MG in cataract patients who without obvious lid margin changes which was quantified using the score proposed by Arita et al. [9]. We aimed to verify the incidence of MG dropout and to explore the relation between MG dropout and subjective symptoms or tear-film function, which will help ophthalmologists better understand the underlying cause of dry eye disease and provide assistance regarding the management of the MG condition during followup to prevent or reduce damage to the ocular surface.
Materials and Methods
Subjects and examination
Ninety-nine consecutive patients (mean age 62.82 ± 9.32 years, range 42-87; 47 female) who consulted for cataract surgery were recruited form the department of cataract of Jinan Mingshui Eye Hospital (Zhangqiu, China) between May and August 2015. Written informed consent was obtained from all subjects or authorized client before the examination. This study was approved by the Ethics Committee of Jinan Mingshui Eye Hospital (Zhangqiu, China) and adhered to the tenets of the Declaration of Helsinki.
Exclusion criteria were as follows: (1) acute eye inflammatory response or infection; (2) allergy; (3) abnormal limbal stem cells or other causes of ocular surface diseases, such as chemical or thermal burns; (4) ocular surgery or trauma; (5) contact lens wearing and lubricant using in history; and (6) MGD diagnosed by a slit-lamp microscope which indicating significant changes in the eyelid or orifice.
Assessments included gender, age, slit-lamp examination, noninvasive tear breakup time (NIBUT)-first (time at which the first breakup of tears occurs), NIBUT-average (average time of all breakup incidents), tear meniscus height (TMH) and meibography. Subjects were classified by severity based on subjective symptoms, as reported on the Ocular Surface Disease Index (OSDI) (Table 1) [12,13]. All data were obtained by the same ophthalmologist and the same technician.
| Parameter | Descriptive statistic |
|---|---|
| Age (mean ± SD), years | 62.82 ± 9.32 (range 42-87) |
| Gander | |
| Males, n (%) | 52 (52.52%) |
| Females, n (%) | 47 (47.47%) |
| NIBUT-first (mean ± SD), second | 6.34 ± 4.93 (range 1.34-23.90) |
| NIBUT-average (mean ± SD), second | 8.42 ± 5.51 (range 1.78-23.90) |
| TMH (mean ± SD), mm | 0.20 ± 0.11 (range 0.05-0.65) |
| OSDI (mean ± SD) | 28.08 ± 9.82 (range 0-60.7) |
| Grade 1, n (%) | 4 (4.04%) |
| Grade 2, n (%) | 64 (64.64%) |
| Grade 3, n (%) | 24 (24.24%) |
| Grade 4, n (%) | 7 (7.07%) |
| Meiboscores (mean ± SD) | |
| Upper eyelid | 1.43 ± 0.84 (range 0-3) |
| Lower eyelid | 1.64 ± 0.79 (range 0-3) |
| Upper and lower eyelids | 3.07±1.39 (range 0-6) |
DSDI: Ocular Surface Disease Index; NIBUT: Noninvasive Tear Breakup Time.
Table 1. Descriptive statistics of the subjects.
Examinations
Slit-lamp observation showed no blepharitis, corneal fluorescein staining and MG orifices clogging. Cataract diagnostic criteria were as follows: the lens became opaque (degeneration and clouding) and affected vision, but corrected visual acuity of 20/40 or less.
Subjective questionnaire
The OSDI questionnaire, developed by the Outcomes Research Group at Allergan Inc (Irvine, Calif), is a 12-item questionnaire designed to provide a rapid assessment of dry eye [12]. In this study, all patients completed the OSDI questionnaire, which was scored according to previous describes [12,14]. The 12 items of the OSDI questionnaire were graded on a scale 0 to 4, where 0 indicated none of the time; 1, some of the time; 2, half of the time; 3, most of the time; and 4, all of the time. The total OSDI score was then calculated on the basis of the following formula: OSDI=[(sum of scores for all questions answered) × 100]/[(total number of questions answered) × 4]. Thus, the OSDI scoring is based on a 0 to 100 scale and higher scores indicate more severe symptoms or discomfort.
Measurements using a keratograph 5M device
All the subjects underwent imaging with a keratography 5M equipped with modified TF-scan software performed in dark room conditions by the same operator. After 3 to 4 blinks, the subjects were asked to keep his or her eyes open as long as possible. From this moment on, the reflected projection surface was observed closely. TBUT was measured twice for each eye using IR video derived from the NIBUT tool, followed by the standard fluorescein staining of the tear film. NIBUT-first (time at which the first breakup of tears occurs) and NIBUTaverage (average time of all breakup incidents) measurements were obtained [15]. After NIBUT measurements in each subject, 3-4 seconds rest with eyes closed, lower tear film meniscus images were captured.
The upper lid (UL) and lower lid (LL) was imaged with the meibography technique respectively by the Meibo-scan system. The MG dropout score of the UL and LL was scored using a 4-grade scoring system (0-3) as Arita described as. Briefly, MG loss was scored using the following rating for each eyelid: Grade 0, no loss of MG; Grade 1, loss of area was less than 1/3 of the total MG area; Grade 2, loss of area was between 1/3 and 2/3; Grade 3, loss of area was more than 2/3. Meiboscores for the upper and lower eyelids were summed to obtain the score for each eye (0-6). Due to the similar nature of the two eyes, data from only right eyes were analysed to avoid statistical bias [16].
Statistical analysis
Data were analyzed using SPSS 23.0 (SPSS Inc., Chicago, US). Correlations among meiboscores, OSDI scores and ocular surface examinations (TMH, NIBUT-first, NIBUT-average) were evaluated by Kendall’s correlation. The difference in meiboscores between the males and the females was determined using the Mann-Whitney U-test. P values <0.05 was considered significant.
Results
MG dropout grades
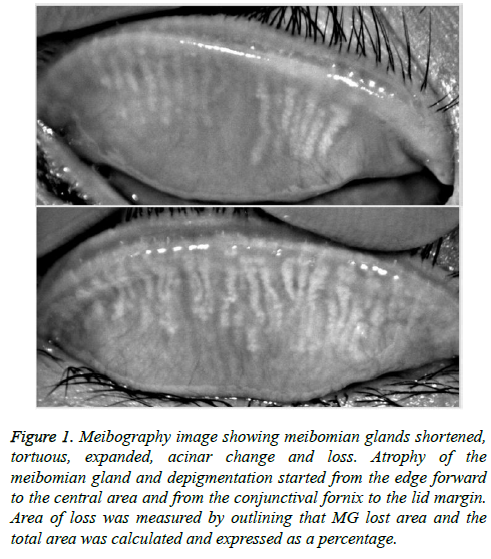
Meiboscore of the MG by Keratograph 5M: Clear images of the MG were obtained using the Meibo-Scan system in all subjects. The MG photographs displayed a variety of morphological changes, such as shortened, tortuous, expanded, and lost MG. Atrophy of the MG and depigmentation started from the edge forward to the central area and from the conjunctival fornix to the lid margin (Figure 1).
Figure 1: Meibography image showing meibomian glands shortened, tortuous, expanded, acinar change and loss. Atrophy of the meibomian gland and depigmentation started from the edge forward to the central area and from the conjunctival fornix to the lid margin. Area of loss was measured by outlining that MG lost area and the total area was calculated and expressed as a percentage.
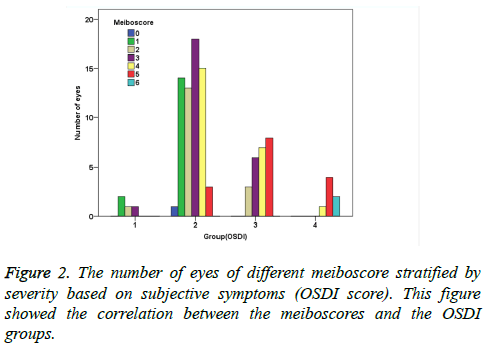
The average meiboscore was 3.07 ± 1.39. Among them, 1% scored 0 (1 eye), 16.2% scored 1 (16 eyes), 17.2% scored 2 (17 eyes), 25.3% scored 3 (25eyes), 23.2% scored 4 (23 eyes), 15.2% scored 5 (15 eyes) and 2% scored 6 (2 eyes). A total of 65.7% (66 eyes) scored ≥ 3 on the MG photographic analysis (Table 1 and Figure 2).
Correlation between meiboscore and gender/age: The average meiboscore for 52 males was 3.04 ± 1.44 and that for 47 females was 3.11 ± 1.35 (Table 1). No significant difference was observed between the meiboscores of the males and females (Mann-Whitney U-test, P=0.940). The mean age of all subjects was 62.82 ± 9.32 years. The mean age for males was 62.13 ± 8.82 years and that for females was 63.57 ± 9.88 years (Table 1). The correlations between meiboscore and age is significant (r=0.217, p=0.031) (Table 2).
| Meiboscores | |||
|---|---|---|---|
| Correlation coefficient | p | ||
| Age | 0.217? | 0.031 | |
| Ocular Surface Disease Index | 0.431* | 0 | |
| Noninvasive tear breakup time (first) | 0.017* | 0.821 | |
| Noninvasive tear breakup time (average) | -0.24* | 0.745 | |
| Tear meniscus height | -0.32* | 0.676 | |
?Spearman’s correlation test was used. *Kendall’s correlation test was used.
Table 2. Correlation coefficients between subjective symptoms and meinoscore.
Correlation between meiboscore and subjective symptoms: Table 1 showed that there were ninety-five of the subjects fell into the mild, moderate, to severe class (symptomatic), whereas the remaining 4 subjects fell into the normal class (asymptomatic) (Table 1). The average OSDI score was 28.08 ± 9.82 (range 0-60.7) and a significant correlation was observed between meiboscore and OSDI (Kendall’s r=0.431) (Table 2).
Correlation between meiboscore and objective examination: The average of TMH, NIBUT-first and NIBUTaverage was 0.20 ± 0.11 (range>0.20 mm), 6.34 ± 4.93 s and 8.42 ± 5.51 s, respectively (Table 1). The correlations between the meiboscore and the various ocular surface examinations were evaluated by Kendall’s correlation. The correlations among TMH, NIBUT-first, and NIBUT-average are not significant (Table 2).
Discussion
Cataract surgery has given innumerable patients good visual acuity, but many patients are beleaguered by dry eye, which has become one of the most important factors influencing quality of life (QOL) after the procedure. Dry eye is closely related to the meibography, especially the extent of MG dropout. However, in clinical work, ophthalmologists pay more attention to patient’s cornea, lid margin, MG orifice than MG dropout before cataract surgery. Traditional method to check lid and lid margin is using slit-lamp biomicroscopy, however, it does not allow visualize of morphological changes to the MG in the tarsal plate. Meibography is the only method available for the assessment of MG because it can visualize and photograph the morphology of MG structures, although confocal microscopy has also been used to assess the acinar density recently [17-19]. In this study, we investigated the morphological changes of the MG in patients with cataract disease without obvious lid margin changes and fluorescein corneal staining. We used a keratography 5M to obtain the data of NIBUT-first, NIBUT-average, THM and to visualize MG dropout. We also explore the relation between meiboscore and tear-film function and OSDI score, which will help ophthalmologists better understand the underlying cause of dry eye after cataract surgery and provide assistance regarding the management of the MG condition during follow-up to prevent or reduce damage to the ocular surface.
We found that there was a massive loss of MG in almost cataract patients, who without significant changes of the lid margin and fluorescein corneal staining. The average meiboscore was 3.07 ± 1.39 and the OSDI score was 28.08 ± 9.82. A significant correlation was observed between meiboscore and OSDI score, which is in agreement with previous studies [20]. In previous studies, inconsistent findings have been reported on the correlation between MG and dry eye. The United States and Japan accounted for 20%–55% of MG abnormalities in normal populations [21] and up to 65% abnormalities in dry eye patients [22]. Researchers in Spain found that nearly half of the patients with dry eye disease suffered from MGD [23]. MGD studies in China and Taiwan found no correlation between the symptoms of MGD and those of dry eye disease [9,11]; However, other studies have found correlations between them [24]. The reason for these inconsistencies in the published data is probably due to different diagnostic criteria. No standard criterion for MGD diagnosis was available until the recently published international workshop diagnosis on MGD in 2011 [6].
We also found that no significant correlation was observed between meiboscore and objective examination (NIBUT-first, NIBUT-average and TMH), this finding is in accordance with a previous report [9-11]. The TMH represents the aqueous volume of tear film, it is reasonable that it did not correlate with MG changes. Moreover, tear film BUT depends not only on the oily layer of the tear film but also on the aqueous and mucous layers, so it is not surprising that MG changes were not correlated with tear film BUT. Taken together, various factors including MG changes may be involved in the development of dry eye syndrome and ocular surface disorders. The clinical significance of these meibography finding in the diagnosis of dry eye and MGD should be evaluated in future studies of patients with dry eye and MGD. According to a recent Japanese study [25], MG dropout is an important cause for dry eye in patients. MG lipid abnormalities can lead to chronic eye irritation and epithelial damage of the ocular surface and photographic score ≥ 3 have clinical significance. In our study, 66.7% (65 eyes) of the patients with meiboscore ≥ 3 without lid margin changes. This result confirms that MG dropout is a very common and often overlooked problem related to dry eye disease. Lipid abnormalities lead to the tear film that cannot be sustained evenly on the surface, resulting in tear film excessive evaporation and instability [6,22]. Early detection of morphological changes in the cataract patients without lid margin changes is very important, and ophthalmologist should be aware of the possibility of MG changes at the follow-up.
MG dropout occurs as an age-related atrophic process [26]. Our study showed a correlation between age and the MG photographic score (r=0.217, P=0.035), suggesting that MG dropout becomes worse with age, as reported previously [9,21]. Meibography has been studied for over three decades, initially, meibography was done using a probe which is invasive and discomfort. To overcome these difficulties, new inspection equipment and techniques was invented [11]. Keratograph 5M is a non-invasive, non-contact device and it provides a rapid and objective clinical method of capturing images of the MG. Measurements of NIBUT obtained with this newly developed corneal topography may provide a simple, noninvasive screening test for dry eyes with acceptable sensitivity, specificity and repeatability [15]. Meibography may provide a simple and fast way for MG morphology evaluation for patients with irritated eyes. In addition to its usage as a diagnostic tool to help physicians, meibography may offer easy demonstration regarding the MG disease for the patient’s education. If meibography becomes a routine test before cataract surgery, ophthalmologists will discover abnormal MG disorder early and patients can be educated. Thus, the dissatisfaction rate in patients with dry eye after cataract surgery will be reduced. In this study, subjective digital grading scales instead of Image J software was used to analyze the meibography images, which was easy to undertake and was consistent with the majority of the published literature on meibography [9,17,22]. However, development of appropriate cutoff values for these images requires further work.
This study had certain limitations. First, this study was conducted in a relatively small number of subjects and a large sample is needed to confirm our findings. Second, only morphologic changes but no quality changes of the MG were evaluated in this study. Sullivan et al. [27] reported that aging is associated with alterations in the lipid profiles of MG secretions. The relative significance of these quality changes in the meibum and the morphologic changes of MG in the diagnosis and pathogenesis of MGD remain to be clarified. Third, this study lacks the analysis of these subject’s ocular parameters after cataract surgery, because some of patients choose elective surgery, we will continue the further research. In summary, our results provide important information showing that a large proportion of MG dropout cases in Chinese cataract patients without significant changes of the lid margin and keratoconjunctiva, which maybe the underlying cause of dry eye after cataract. In order to discover MG disorder and educate patients early, we should make meibography become a routine test before cataract surgery. The keratography 5M is a useful and non-contact, non-invasive inspection equipment to obtain information about the MG structure.
References
- Cetinkaya S, Mestan E, Acir NO, Cetinkaya YF, Dadaci Z, Yener HI. The course of dry eye after phacoemulsification surgery. BMC Ophthalmology 2015; 15: 68.
- Han KE, Yoon SC, hn JM, Nam SM, Stulting RD, Kim EK, Seo KY. Evaluation of dry eye and meibomian gland dysfunction after cataract surgery. Am J Ophthalmol 2014; 157: 1144-1150.
- Li XM, Hu L, Hu J, Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea 2007; 26: S16-20.
- Shimazaki JSM, Tsubota K. Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch Ophthalmol 1995; 113: 1266-1270.
- McGinnigle S, Naroo SA, Eperjesi F. Evaluation of dry eye. Survey Ophthalmol 2012; 57: 293-316.
- Tomlinson A, Bron AJ, Korb DR, Amano S, Paugh JR, Pearce EI, Yee R, Yokoi N, Arita R, Dogru M. The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Visual Sci 2011; 52: 2006-2049.
- Bron AJ, Tiffany JM. The contribution of meibomian disease to dry eye. Ocul Surf 2004; 2: 149-165.
- Nichols KK. The international workshop on meibomian gland dysfunction: introduction. Invest Ophthalmol Visual Sci 2011; 52: 1917-1921.
- Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 2008; 115: 911-915.
- Feng Y, Gao Z, Feng K, Qu H, Hong J. Meibomian gland dropout in patients with dry eye disease in China. Cur Eye Res 2014; 39: 965-972.
- Srinivasan S, Menzies K, Sorbara L, Jones L. Infrared imaging of meibomian gland structure using a novel keratograph. Optometry Vision Sci 2012; 89: 788-794.
- Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 2000; 118: 615-621.
- Sullivan BD, Whitmer D, Nichols KK, Tomlinson A, Foulks GN, Geerling G, Pepose JS, Kosheleff V, Porreco A, Lemp MA. An objective approach to dry eye disease severity. Invest Ophthalmol Visual Sci 2010; 51: 6125-6130.
- Walt JGRM, Stern KL. Evaluating the functional impact of dry eye: The Ocular Surface Disease Index. Drug Inf J 1997; 31: 1436.
- Hong J, Sun X, Wei A, Cui X, Li Y, Qian T, Wang W, Xu J. Assessment of Tear Film Stability in Dry Eye With a Newly Developed Keratograph. Cornea 2013; 32: 716-721.
- Best N, Drury L, Wolffsohn JS. Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye 2012; 35: 171-174.
- Nichols JJ, Berntsen DA, Mitchell GL, Nichols KK. An assessment of grading scales for meibography images. Cornea 2005; 24: 382-388.
- Wei A, Hong J, Sun X, Xu J. Evaluation of age-related changes in human palpebral conjunctiva and meibomian glands by in vivo confocal microscopy. Cornea 2011; 30: 1007-1012.
- Matsumoto Y, Sato EA, Ibrahim OM, Dogru M, Tsubota K. The application of in vivo laser confocal microscopy to the diagnosis and evaluation of meibomian gland dysfunction. Mol Vis 2008; 14: 1263-1271.
- Pult H, Riede-Pult BH. Non-contact meibography: keep it simple but effective. Contact lens & anterior eye. J Br Contact Lens Assoc 2012; 35: 77-80.
- Den S, Shimizu K, Ikeda T, Tsubota K, Shimmura S, Shimazaki J. Association between meibomian gland changes and aging, sex, or tear function. Cornea 2006; 25: 651-656.
- Shimazaki J, Sakata M, Tsubota K. Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch Ophthalmol 1995; 113: 1266-1270.
- Viso EGF, Rodriguez-Ares MT. The association of meibomian gland dysfunction and other common ocular diseases with dry eye: a population-based study in Spain. Cornea 2011; 30: 1-6.
- Pult H, Purslow C, Murphy PJ. The relationship between clinical signs and dry eye symptoms. Eye (Lond) 2011; 25: 502-510.
- Obata H. Anatomy and histopathology of human meibomian gland. Cornea 2002; 21: S70-74.
- Jie Y, Xu L, Wu YY, Jonas JB. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye (Lond) 2009; 23: 688-693.
- Sullivan BD, Evans JE, Dana MR, Sullivan DA. Influence of aging on the polar and neutral lipid profiles in human meibomian gland secretions. Arch Ophthalmol 2006; 124: 1286-1292.