Case Report - Otolaryngology Online Journal (2019) Volume 9, Issue 3
Large Unilocular Radiolucent Lesions of the Jaws: A Pathologist’s Enigma and a Surgeon’s Conundrum
- *Corresponding Author:
- Colonel Priya Jeyaraj, MDS, Oral and Maxillofacial Surgery, Commanding Officer, Military Dental Centre (Gough Lines), Secunderabad, Telangana, India, Tel: +919596840303; E-mail: jeyarajpriya@yahoo.com
Received date: March 18, 2019; Accepted date: April 16, 2019; Published date: April 23. 2019
Abstract
Unilocular radiolucent lesions of the jaws, in particular, those which cause extensive destruction and hollowing out of the bone, are a major cause for concern, both, with regards to their correct diagnosis, as well as a timely institution of the most appropriate treatment procedure. A relatively aggressive lesion with considerable invasive and recurrence potential, such as an Odontogenic tumor may radiologically and sometimes even histopathologically masquerade as a seemingly innocuous pathology such as an Odontogenic cyst. It is imperative to precisely diagnose and completely eliminate the lesion, while at the same time, ensure least possible morbidity for the patient, such as pathological fractures, persisting neurological deficits, esthetic deformity, functional debility, and of course, recurrence or persistence of the lesion. Histopathological examination supplemented by Immunohistochemical analysis of biopsy specimens, using Tumor Markers such as Calretinin and Prognostic Indicators such as Ki-67 and Proliferating Cell Nuclear Antigen (PCNA), have proved invaluable in correctly distinguishing between Odontogenic cysts and tumors and indicating their likely prognosis, thereby aiding in their correct management.
Keywords
Immunohistochemistry; Unicystic lesions; Dentigerous cysts; Unicystic ameloblastoma; Ki-67; Proliferating cell nuclear antigen; Proliferation index; Labelling index
Introduction
The most common cause of a large unilocular lytic lesion of the jaws is the Odontogenic cyst, and when seen in association with an impacted tooth, it is most likely to be a Dentigerous cyst [1]. This is the most common non-inflammatory Odontogenic cyst which develops from the epithelial remnants of the dental follicle as a result of fluid accumulation between the follicular epithelium and crown of a developing or unerupted tooth.
Unless noticed on radiographs as an incidental finding, these cysts often remain undetected. They are capable of enlarging unobtrusively and asymptomatically, attaining quite large sizes, causing considerable hollowing out of the jaws. It is usually only when they are associated with pain, infection, inflammation or a visible bony expansion, that they are observed, investigated and diagnosed. A cause of concern is that these cysts may also transform into an Odontogenic tumor such as Ameloblastoma and its variants [2], or even into Mucoepidermoid carcinoma [3] or Squamous cell carcinoma. Accurate and precise diagnosis is crucial in order to institute the correct surgical treatment modality and manage the pathology adequately.
When Odontogenic tumors present as a Unilocular radiolucency, they exhibit marked similarities to the Odontogenic cysts, with even overlapping histological features. However, they vary considerably from the cysts in their biological behavior, in terms of invasiveness, aggressiveness, tendency for local destruction, recurrence and malignant transformation; and hence require vastly different therapies and treatment modalities from the former [4]. In this way, what may appear as an innocuous Unicystic lesion, mimicking an Odontogenic cyst, may in fact be an aggressive and destructive tumor, adding to its enigma and diagnostic dilemma for the Oral pathologist and a conundrum for the Maxillofacial surgeon as to its most appropriate and ideal management modality [5].
Case Report
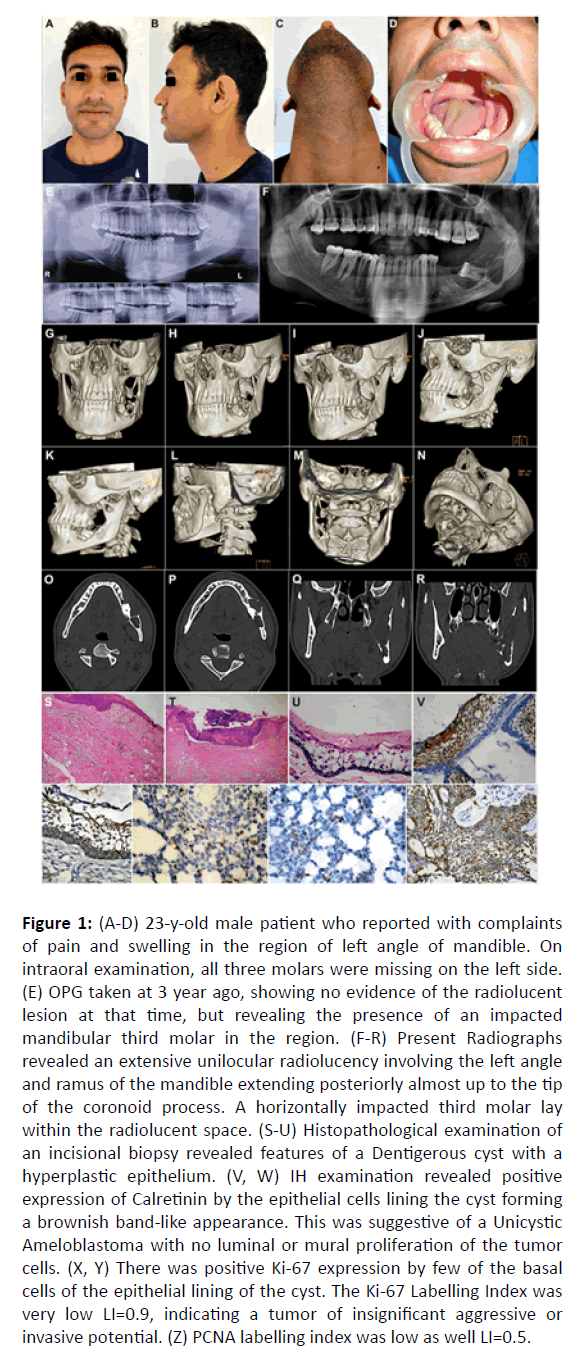
A 23-year-old male patient reported with the complaint of a swelling on the left side of the face in the region of the lower jaw, for the past five months, which over the past three days, had been accompanied by a dull, deep seated pain in the region. Clinical examination showed a diffuse, firm and tender swelling in the region of the left angle and ramus of the mandible, extending below to involve the inferior border of the mandible, and above, almost up to the Temporomandibular joint region. On intraoral examination, all three left lower molar teeth were missing and the alveolar mucosa in the region appeared swollen and inflamed. There was no sinus opening or purulent discharge noted intra- or extra orally. There was mild regional lymphadenopathy, and the patient was mildly febrile (Figure 1).
Figure 1: (A-D) 23-y-old male patient who reported with complaints of pain and swelling in the region of left angle of mandible. On intraoral examination, all three molars were missing on the left side. (E) OPG taken at 3 year ago, showing no evidence of the radiolucent lesion at that time, but revealing the presence of an impacted mandibular third molar in the region. (F-R) Present Radiographs revealed an extensive unilocular radiolucency involving the left angle and ramus of the mandible extending posteriorly almost up to the tip of the coronoid process. A horizontally impacted third molar lay within the radiolucent space. (S-U) Histopathological examination of an incisional biopsy revealed features of a Dentigerous cyst with a hyperplastic epithelium. (V, W) IH examination revealed positive expression of Calretinin by the epithelial cells lining the cyst forming a brownish band-like appearance. This was suggestive of a Unicystic Ameloblastoma with no luminal or mural proliferation of the tumor cells. (X, Y) There was positive Ki-67 expression by few of the basal cells of the epithelial lining of the cyst. The Ki-67 Labelling Index was very low LI=0.9, indicating a tumor of insignificant aggressive or invasive potential. (Z) PCNA labelling index was low as well LI=0.5.
History revealed that he had been operated for a large cystic lesion of the left mandibular angle and body, 11 years ago. Case records revealed that a marsupialization procedure had been carried out when he was a 12-year-old child, and the left lower first and second molar teeth had been removed during the same surgical procedure, however, the third molar tooth germ had been left in situ. The reason given by the then treating surgeon was that the bone of the mandible had been excessively hollowed out and was extremely weak, vulnerable and liable to fracture had removal of the third molar or enucleating of the entire lesion had been attempted in the young child.
The patient had been reviewed for a year, but had not been taken up for surgical enucleation of the remaining pathology and the remnant cyst lining. The patient had thereafter not reported back for follow up until three years ago, when an orthopantomogram had been taken. It did not reveal any obvious pathology or lesion within the bone, other than the horizontally impacted 38 lying in the angle region of the mandible (Figure 1).
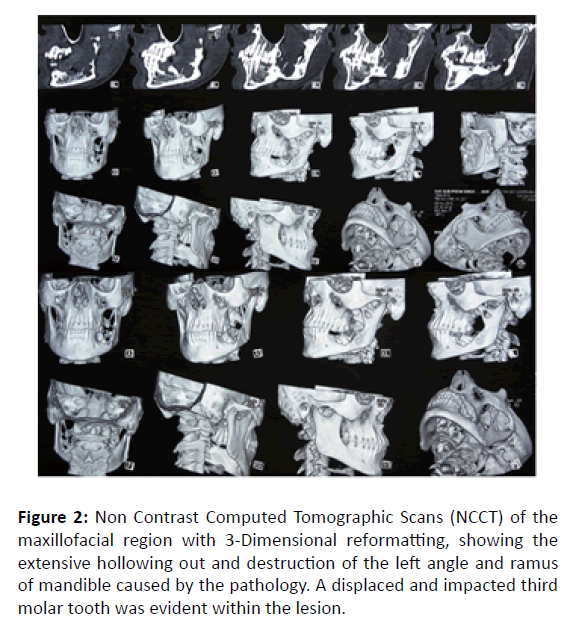
An Orthopantomogram was taken which revealed a large radiolucency involving the left angle and ramus of the mandible extending posteriorly almost up to the tip of the coronoid process and anteriorly up to the missing first molar region. A horizontally impacted third molar lay within the radiolucent space. Non Contrast Computed Tomographic Scans (NCCT) of the maxillofacial region showed extensive destruction and hollowing out of the bone in the region of the angle and ramus on the left side with buccal as well as lingual cortical perforation noted at various locations. On corroborating the clinical and radiographic findings with the history, a provisional diagnosis of a persisting and progressing cystic lesion of the left mandibular angle and ramus, most likely, a Dentigerous cyst in relation to the impacted mandibular third molar tooth, with secondary infection, was made. Differential diagnosis included odontogenic tumors such as Ameloblastoma or Keratocystic Odontogenic Tumor (KCOT) (Figure 2).
Figure 2: Non Contrast Computed Tomographic Scans (NCCT) of the maxillofacial region with 3-Dimensional reformatting, showing the extensive hollowing out and destruction of the left angle and ramus of mandible caused by the pathology. A displaced and impacted third molar tooth was evident within the lesion.
The patient was put on Oral Antibiotics and Antiinflammatory medication for five days, to which he responded very well with a complete resolution of the pain and reduction in size of the swelling. An incisional biopsy was carried out removing a small window of bone through the buccal cortical plate. Histopathological examination of the tissue sample revealed features of a dentigerous cyst with a hyperplastic epithelium. Immunohistochemical examination revealed positive expression of Calretinin by the epithelial cells lining the cyst, forming a brownish band-like appearance. This was suggestive of a unicystic Ameloblastoma with no luminal or mural proliferation of the tumor cells. There was positive Ki-67 expression by few of the basal cells of the epithelial lining of the cyst. The Ki-67 Labelling Index was very low LI=0.9, indicating a tumor of mild aggressive or invasive potential. PCNA labelling index was low as well LI=0.5.
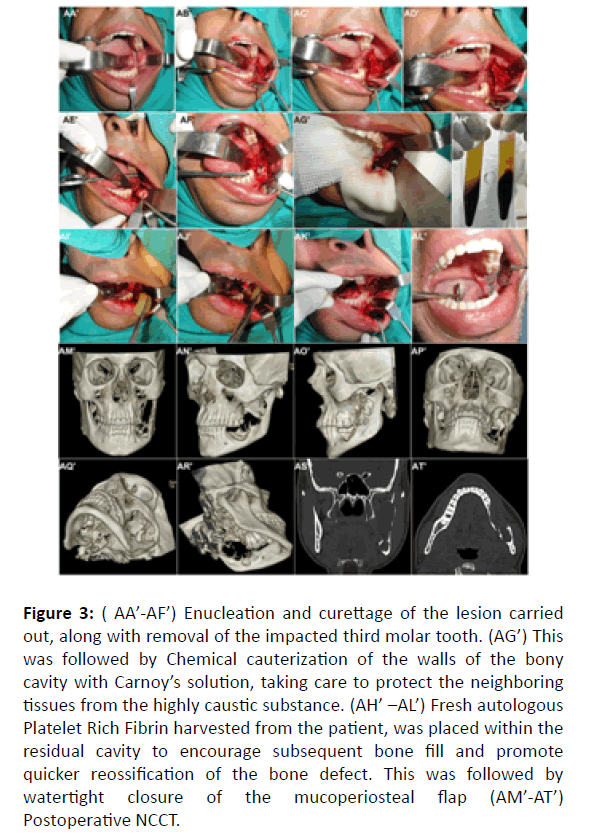
The patient was taken up for Enucleation and Curettage of the cystic lesion of the left angle and ramus of the mandible via an intraoral approach, removal of the horizontally impacted third molar tooth lying within the lesion, and peripheral ostectomy of the residual bony walls. This was followed by chemical cauterization of the walls of the bone defect using Carnoy’s solution, in order to completely eliminate any persisting or residual tumor cells in the vicinity. Autologous Platelet Rich Fibrin was then placed within the bony cavity to accelerate both soft tissue healing in the operated site as well encourage and hasten bone fill with the residual large bony defect of the mandible, so as to facilitate an early rehabilitation of the young patient subsequently with dental prostheses for the missing molar teeth (Figure 3).
Figure 3: ( AA’-AF’) Enucleation and curettage of the lesion carried out, along with removal of the impacted third molar tooth. (AG’) This was followed by Chemical cauterization of the walls of the bony cavity with Carnoy’s solution, taking care to protect the neighboring tissues from the highly caustic substance. (AH’ –AL’) Fresh autologous Platelet Rich Fibrin harvested from the patient, was placed within the residual cavity to encourage subsequent bone fill and promote quicker reossification of the bone defect. This was followed by watertight closure of the mucoperiosteal flap (AM’-AT’) Postoperative NCCT.
Discussion
The importance and value of the correct diagnosis as well as an indication of the likely prognosis of a destructive jaw lesion cannot be stresses enough. Immunohistochemistry is of immense value, both, as a diagnostic indicator as well as a prognostic indicator, guiding the ideal management protocol to be employed, on a case to case basis [6].
Enucleation is the procedure of choice for removal of most cysts and other benign pathology of the oral and maxillofacial region, and involves complete removal of the entity. It is suitable for those pathologies which are surrounded by a capsule that is anatomically distinct and cleaves easily from the surrounding tissue, and is thus amenable to this type of therapy. Physical or chemical curettage may be added to the enucleation procedure in certain pathologies that require additional removal of surrounding bone suspected to have microscopic invaginations of the lesion or satellite cysts/ tumours, to help ensure their complete removal and to decrease the persistence and recurrence of the lesion [7]. Curettage may be completed with a sharp curette or a round diamond/tungsten carbide bur with copious cool irrigation to remove 1 to 2 mm of bone containing any pathology remnants.
Meticulous technique in the procedure of enucleation and curettage is particularly important in the surgical management of lesions that tend to have high recurrence or persistence rates, in which case, the addition of Carnoy’s solution to curettage or peripheral ostectomy has been shown to be even more effective in decreasing the recurrence rate than are the enucleation procedures alone [8]. This procedure was employed, in this case of Dentigerous cyst showing histopathological evidence of ameloblastomatous change, which by means of corroborating the histopathological as well as Immunohistochemical findings, was precisely diagnosed as Unicystic Ameloblastoma of the luminal subtype.
Immunohistochemical analysis helped in diagnosing the presence of Ameloblastoma by means of the positive expression of Calretinin which is a tumor marker specific for Ameloblastoma and its variants [9]. This diagnosis could have been missed entirely, had histopathological examination alone been relied upon. Further, the low Labelling Index of the Immunohistochemical Proliferative Markers (Ki-67 and PCNA) [10], also helped prevent overtreatment in the form of Jaw resection in this young patient. Institution of additional measures in terms of a vigorous and thorough curettage with peripheral ostectomy of a 5 mm margin of bone all along the periphery of the lesion, in addition to chemical cauterization of the bony walls of the residual defect to destroy any remnant tumor cells, would help prevent future recurrence of the lesion.
The enucleation and curettage procedure is limited in the treatment of multicystic lesions [11] for which the treatment of choice might otherwise be the Unicystic counterpart [12]. Benign multicystic lesions of the oral and maxillofacial region may have numerous loculations and invaginations that would make access extremely difficult using even an extraoral approach and almost impossible if using an intraoral approach. In addition, the enucleation process may not remove the pathology in its entirety, and physical and chemical curettage may not be able to access or remove all remnants of the lesion. This will invariably lead to persistence of the lesion, particularly a high-recurrence lesion like the Keratocystic Odontogenic Tumor, or in aggressive benign lesions such as the Solid/ Multicystic Ameloblastoma [13].
Conclusion
In cases of extensive Unilocular lesions of the jaws, where ambiguity often exists in both diagnosis and appropriate treatment plan, Immunohistochemistry can serve as an invaluable tool in establishing the precise diagnosis, guiding the treatment plan, as well as indicating the likely prognosis of these lesions. Thus, it is of utmost importance to correlate histopathologic findings with clinical and radiographic features as well as Immunohistochemical analysis, to arrive at a correct definitive diagnosis as all such lesions may have prognostically different biologic behaviors and the final diagnosis may alter the therapeutic decision significantly.
Compliance with Ethical Standards
Disclosure of potential conflicts of interest
The author of this article has not received any research grant, remuneration, or speaker honorarium from any company or committee whatsoever, and neither owns any stock in any company. The author declares that she does not have any conflict of interest.
Research involving human participants and/or animals
All procedures performed on the patients (human participants) involved were in accordance with the ethical standards of the institution and/or national research committee, as well as with the 1964 Helsinki declaration and its later amendments and comparable ethical standards.
Ethical Approval
This article does not contain any new studies with human participants or animals performed by the author.
Informed Consent
Informed consent was obtained from all the individual participants in this study.
Funding
This study was not funded by any organization/ society.
References
- Freitas DQ, Tempest LM, Sicoli E, et al. Bilateral dentigerous cysts: Review of the literature and report of an unusual case. Dentomaxillofac Radiol. 2006;35:464?48.
- Rosenstein T, Pogrel MA, Smith RA, et al. Cystic ameloblastoma-Behaviour and treatment of 21 cases. J Oral Maxillofac Surg. 2001;59:1311-16.
- Gulbranson SH, Wolfrey JD, Raines JM, et al. Squamous cell carcinoma arising in a dentigerous cyst in a 16?month?old girl. Otolaryngol Head Neck Surg. 2002;127:463?64.
- Scariot R, da Silva RV, da Silva Felix Jr W, et al. Conservative treatment of ameloblastoma in child: A case report. Stomatologija. 2012;14: 33-6.
- Chapelle KA, Stoelinga PJ, Wilde PC, et al. Rational approach to diagnosis and treatment of ameloblastomas and odontogenic keratocysts. Br J Oral Maxillofac Surg. 2004;42:381-90.
- Goncalves CK, Fregnani ER, Leon JE, et al. Immunohistochemical expression of p63, epidermal growth factor receptor (EGFR) and notch-1 in radicular cysts, dentigerous cysts and Keratocystic odontogenic tumors. Braz Dent J. 2012;23:337-43.
- Ramesh RS, Manjunath S, Ustad TH, et al. Unicystic ameloblastoma of the mandible-An unusual case report and review of literature. Head Neck Oncol. 2010;14:2-7.
- Lee PK, Samman N. Unicystic ameloblastoma- Use of Carnoy’s solution after enucleation Int. J Oral Maxillofac Surg. 2004;33:263-67.
- De Villiers P, Liu H, Suggs C, et al. Calretinin expression in the differential diagnosis of human ameloblastoma and keratocystic odontogenic tumor. Am J Surg Pathol. 2008;32:256-60.
- Piattelli A, Fioroni M, Santinelli A, et al. Expression of proliferating cell nuclear antigen in ameloblastomas and odontogenic cysts. Oral Oncology. 1998;34:408-12.
- Pogrel MA, Montes DM. Is there a role for enucleation in the management of ameloblastoma? Int J Oral Maxillofac Surg. 2009;38:807?12.
- Navarro CM, Principi SM, Massucato EM, et al. Maxillary unicystic ameloblastoma. Dentomaxillofac Radiol. 2004;331:60-2.
- Nakamura N, Higuchi Y, Mitsuyasu T, et al. Comparison of long term result between different approaches of ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:13-20.