Short Communication - Annals of Cardiovascular and Thoracic Surgery (2020) Volume 3, Issue 2
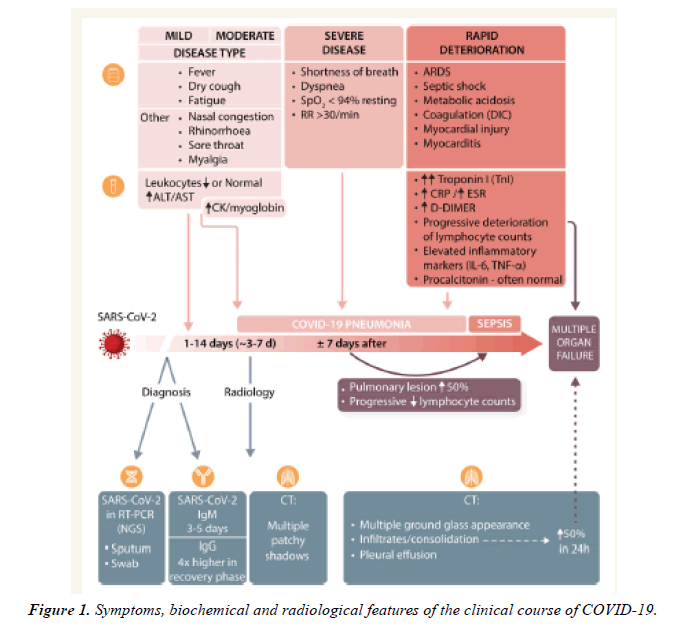
Key symptoms, biochemical and radiological features of the clinical course of COVID-19.
Ankita Singh*
Department of Biotechnology, Modern College of Arts, Science and Commerce, Ganeshkhind, Pune, Maharashtra
- *Corresponding Author:
- Ankita Singh
Department of Biotechnology, Pune University, India
E-mail: ankitabiotechnologist@gmail.com
Accepted July 30, 2020
Citation: Singh A. Key symptoms, biochemical and radiological features of the clinical course of COVID-19. Ann Cardiovasc Thorac Surg. 2020;3(2):5-7.
Abstract
The time period between contact and therefore the first set of symptoms is typically 1–14 days (but up to 24 days in individual cases). The median time between registered exposure and first symptoms is 5.1 days with a mean of 6.1 days. Duration of viral supermolecule shedding ranges between 8 to 34 days (median 20 days) after the initial symptoms. The main clinical symptoms develop within 11.5 days (95% confidence interval (CI) 8.2-15.6 days) and include fever, dry cough, fatigue, ageusia, anosmia, and headache. Other non-specific symptoms have also been reported, including nasal congestion, rhinorrhea, pharyngitis, myalgia, poor appetite, and diarrhoea. Fever and cough typically appear concomitantly, followed by shortness of breath and severe fatigue, which appear around 6-76 day and are related to the development of severe bilateral (and occasional unilateral) pneumonia.
Introduction
The time period between contact and therefore the first set of symptoms is typically 1-14 days (but up to 24 days in individual cases). The median time between registered exposure and first symptoms is 5.1 days with a mean of 6.1 days. Duration of viral supermolecule shedding ranges between 8 to 34 days (median 20 days) after the initial symptoms. The main clinical symptoms develop within 11.5 days (95% Confidence Interval (CI) 8.2-15.6 days) and include fever, dry cough, fatigue, ageusia, anosmia, and headache. Other non-specific symptoms have also been reported, including nasal congestion, rhinorrhea, pharyngitis, myalgia, poor appetite, and diarrhoea. Fever and cough typically appear concomitantly, followed by shortness of breath and severe fatigue, which appear around 6-76 day and are related to the development of severe bilateral (and occasional unilateral) pneumonia. The most common radiological findings include multiple patchy shadows and interstitial changes in moderate disease, with consolidation, a ground glass appearance, in 56.4% of cases and extremely occasional pleural effusions in severe cases. In such severe cases, pneumomediastinum and pneumothorax are described. Pathological investigations of the lungs of deceased individuals indicate blockade of bronchi and bronchioles with large amounts of mucus plugs and bronchial vegetative cell damage. Lymphocyte and mononuclear cell infiltrates are present in alveolar septal spaces. Fibrinous exudate and high hyaline membranes fill alveolar cavities. Polynuclear giant cells are prominent. There’s marked proliferation of type II alveolar epithelial cells. Such severe manifestations appear only during a fraction of patients. A recent study of COVID-19 cases in China reported up to twenty-eight January 2020 indicated that severe illness may occur in 16% of cases, resulting in an overall fatality rate estimated at 1.4% of the overall reported cases 22 to 4.61% within the WHO reports (accessed on 28 March 2020). In some geographical regions, thanks to unexplained reasons, mortality is also higher (current estimates are 11.9% in Italy, 9.0% in Spain, and 7.9% in the UK consistent with the JHU Corona virus Resource Center, accessed on 2 April, 2020). it's important to notice, however, that charge must be taken when calculating fatality rates supported currently available data, as these will be overestimated in respect to insufficient testing within the community or underestimated, because of long lagtime between test positivity and death or the actual fact that there are large differences in attributing COVID-related mortality (‘dying with’ versus ‘dying from’ further as differences in performing post-mortem testing). Limitations of healthcare systems, abruptly overwhelmed by a surge of patients needing mechanical invasive ventilation, have also been considered a possible source of the differences. Finally, these differences may result from population structure, as Italian patients are older than the common age reported within the Chinese patients. The typical clinical course of disease is summarized in figure. The heterogeneity of responses between individual patients is striking. This indicates that it's unlikely that COVID-19 may be considered from the purpose of view of one disease phenotype. Rather, it seems possibly that host characteristics, which at the instant remain unknown, promote progression of the disease with a spread of different presentarions, e.g. mild, severe multiorgan failure, and cytokine release storm. While clinical symptoms of the disease are predominantly respiratory and related to severe pneumonia, both direct and indirect involvement of other organs is common, with the CV system being particularly affected. Moreover, pre-existing conditions, largely linked to CVD, increase the risk of severe outcomes of the infection (Figure 1).