Case Report - Case Reports in Surgery and Invasive Procedures (2017) Case Reports in Surgery and Invasive Procedures (Special Issue 2-2017)
Infective endocarditis on mitral annular calcification complicated with purulent pericarditis: A case report.
- *Corresponding Author:
- Takasumi Goto, MD
Department of Cardiovascular Surgery Osaka University Graduate School of Medicine Japan
Tel:+81668793154
Fax:+81668793163
E-mail: t-goto@surg1.med.osaka-u.ac.jp
Accepted date: May 26, 2017
Citation: Goto T, Toda K, Saito S, et al. Infective endocarditis on mitral annular calcification complicated with purulent pericarditis: A case report.Case Rep Surg Invasive Proced. 2017;1(2):8-11.
Abstract
can be a rare predisposing factor for infective endocarditis (IE). The surgical treatment strategy for such cases remains uncertain. Case presentation: Methicillin-resistant Staphylococcus aureus (MRSA) IE complicated with purulent pericarditis and ventricular septal abscess was diagnosed in an 81-year-old woman with no significant past medical history. The patient underwent surgical treatment in two stages. The first operation consisted of purulent effusion drainage and pedicled omental flap implantation. The second operation, involving mitral vegetation and ventricular septal abscess debridement, was performed 7 days after the first operation. During the admission, appropriate antibiotic therapy was continued. Within a week after the last surgery, patient status (inflammatory markers, fever, and respiratory function) improved remarkably. However, the IE recurred and the patient finally died of sepsis and acute heart failure due to severe mitral regurgitation on postoperative day 37. This report describes a rare case of IE on MAC due to MRSA, complicated with purulent pericarditis caused by extracardiac invasion. Conclusions: Depending on clinical state of the patients, if annular invasion is suspected and MAC is detected in patients with IE, aggressive debridement and reconstruction of mitral annulus and septum might be necessary for such cases.
Keywords
Infective endocarditis, Mitral annular calcification, Methicillin-resistant Staphylococcus aureus.
Abbreviations
IE: Infective Endocarditis; MAC: Mitral Annular Calcification; MRSA: Methicillin-Resistant Staphylococcus aureus; CPB: Cardiopulmonary Bypass
Background
Mitral annular calcification (MAC), which is considered a benign cardiac abnormality, is a common finding in elderly patients and in those receiving hemodialysis [1,2]. MAC can be a predisposing factor for infective endocarditis (IE), which is a rare, but life-threatening complication of MAC [3]. However, few cases of IE on an MAC complicated with purulent pericarditis have been reported, and the surgical strategy in such cases remains unclear.
Case Presentation
An 81-year-old woman with no medical history of immunosuppression, no previous hospitalization, and without any medication, was admitted to a local hospital because of sudden cardiovascular collapse associated with bradycardia. The electrocardiogram showed complete atrioventricular block, and temporary cardiac pacing was inserted. A coronary angiogram showed no coronary artery stenosis. An echocardiogram revealed a vegetation of 8.0 mm on the anterior leaflet of the mitral valve, an MAC on the medial side, and mild mitral regurgitation (MR). Systemic computed tomography showed no evidence of embolism, and confirmed the presence of MAC.
The patient was transferred to the cardiology department in our institution for the treatment of IE. At the admission, the body weight was 37.3 kg and the body height was 139 cm. Blood analysis revealed an increased white blood cell (WBC) count (13.510/μL) and C-reactive protein (CRP) level (34.6 mg/ dL). Because the vegetation was smaller than 10 mm, valve surgery was not performed initially and she received antibiotic therapy (ampicillin-sulbactam, 12 g/day; ceftriaxone, 2 g/day; and gentamicin, 60 mg/day). First collected blood cultures were positive for MRSA and antibiotic therapy was changed to vancomycin 1.5 g/day. Despite appropriate antibiotic treatment, the follow-up echocardiogram demonstrated vegetation enlargement (12 mm) and pericardial effusion (10 mm). Therefore, we attempted urgent mitral valve surgery 4 days after admission.
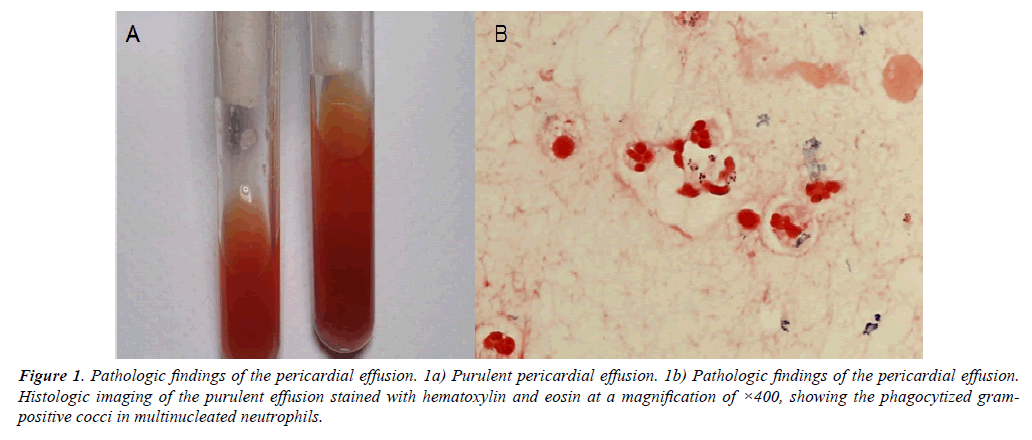
After the median full sternotomy, purulent pericardial effusion gushed out of the cardiac sac, and the heart was completely covered with pus. Histopathologic examination of the effusion revealed phagocytized gram-positive cocci in multinucleated neutrophils (Figure 1).
Figure 1: Pathologic findings of the pericardial effusion. 1a) Purulent pericardial effusion. 1b) Pathologic findings of the pericardial effusion. Histologic imaging of the purulent effusion stained with hematoxylin and eosin at a magnification of ×400, showing the phagocytized grampositive cocci in multinucleated neutrophils.
Considering these findings, we decided to postpone valve surgery and covered the heart with a pedicled omental flap after sufficient saline lavage.
Postoperatively, laboratory data, such as WBC counts and CRP levels, gradually improved. The culture of purulent pericardial effusion was also positive for MRSA. However, the subsequent echocardiogram revealed mitral annular abscess and vegetation enlargement (20 mm). Considering the possibility of uncontrolled infection under antibiotic therapy alone, redo-surgery was performed 7 days after the first operation.
The second operation revealed no purulent effusion in the cardiac sac. The mitral valve was exposed through a superior transept AL approach after bicaval cannulation for cardiopulmonary bypass (CPB). Vegetation was found attached to the mitral annulus at the medial commissure and not to both mitral leaflets. After the vegetectomy and debridement of mitral annulus from left atrium, MR was not detected visually. In the right atrium, there was an abscess in the Koch’s triangle extended from the mitral annulus. Crystal violet injection into the abscess cavity showed blue staining of the posterior wall of the right ventricle, suggesting abscess cavity perforation through the ventricular septum. As the patient was frail and elder, resection of MAC and septum abscess completely and reconstruction of mitral annulus and the septum were too invasive for the patient. Additionally, aggressive debridement of mitral annulus from the left side might expose the perforated abscess cavity to high pressure and potential septal or ventricular rupture, so annular abscess debridement was performed from the right atrium side after mitral valve repair. Subsequently, we covered the posterior wall of the right ventricle, where the abscess perforated, with a pedicled omental flap. The debrided tricuspid annulus was opened to the right atrium. After the patient was weaned from CPB, no remarkable MR was detected by transesophageal echocardiogram.
Postoperatively, complete atrioventricular block converted to normal sinus rhythm, and the laboratory data improved gradually until postoperative day 23. Subsequently, inflammatory marker levels increased again and a follow-up echocardiogram showed mitral annular abscess recurrence and severe MR. In spite of maximum antibiotic therapy, the patient died of sepsis and heart failure on postoperative day 37.
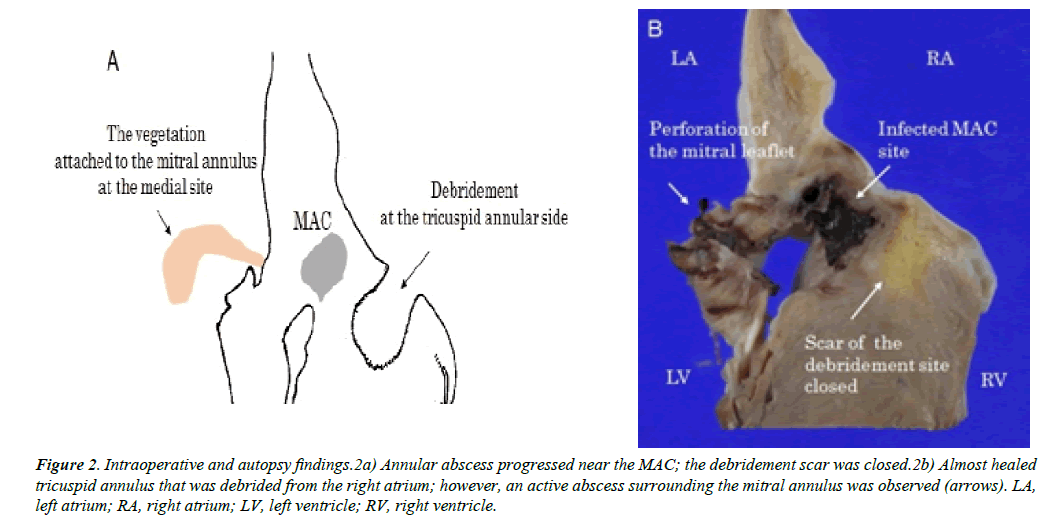
The autopsy showed anterior mitral leaflet perforation with a vegetation in the A3 segment (Figure 2).
Figure 2: Intraoperative and autopsy findings.2a) Annular abscess progressed near the MAC; the debridement scar was closed.2b) Almost healed tricuspid annulus that was debrided from the right atrium; however, an active abscess surrounding the mitral annulus was observed (arrows). LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle.
In the MAC area, an active-phase abscess of the mitral annulus was observed. However, the abscess surrounding the Koch’s triangle was almost healed. Necrotic tissue in the annular abscess was observed from the medial side of the mitral annulus to the cardiac sac, through the ventricular septum.
Discussion
MAC is usually found in elderly population and in patients receiving long-term hemodialysis for chronic renal failure [1-4]. It is supposed to be produced by a chronic degenerative process, and is usually considered a benign cardiac finding. However, MAC can be a predisposing factor for IE, which is not common, but life-threatening complication of MAC [3].
In the presented case, infected MAC was debrided from the right atrial side and exposed to the blood stream, and the patient’s condition was initially improved along with sinus conversion from complete atrioventricular block. However, infected MAC was not sterilized completely and annular abscess recurred, resulting in MR and sepsis. The autopsy specimen revealed the scar tissue in right atrial side and remaining infection in MAC (Figure 2). This finding suggested that healing process in the right atrium prevented further sterilization of abscess cavity by antibiotics in blood stream and surgery required more aggressive approach including complete resection of infected MAC with extensive reconstruction of mitral annulus as well as ventricular septum through which myocardial abscess spread to pericardial cavity causing purulent pericarditis.
A few successfully treated cases of IE on MAC have been previously described [2]. Tsunekawa et al. reported a case of IE on MAC complicated with pseudoaneurysm. Mitral leaflet resection, mitral annular decalcification, and mitral valve replacement with a mechanical valve were performed, and the patient showed no recurrence of infection. Resection of MAC and vegetation might be beneficial in selected patients for IE developed on MAC. However, in the present case, IE was active with positive blood culture and purulent pericarditis. In this setting, extensive reconstruction of annulus and septum with artificial materials was not an available option in our mind. Although careful consideration was necessary, there might have been optimal timing for more aggressive treatment for this frail patient during the process of surgical treatments.
The pathogen in this case was considered to be communityassociated (CA)-MRSA, which is a globally distributed pathogen that can cause lethal infections and the incidence of invasive infections caused by CA-MRSA, is growing at a faster rate than that of nosocomial MRSA [5,6]. Therefore, the infection recurrence in this case may be attributed not only to extensive expansion of IE in MAC, but also to CA-MRSA invasiveness.
Conclusions
We described a very rare case of extensive infection of MAC with CA-MRSA, complicated with purulent pericarditis due to extracardiac expansion of the myocardial abscess. Debridement and drainage of infected MAC from the right atrium did not result in definitive treatment and extensive debridement and reconstruction of the mitral annulus and septum was necessary during the process of the treatment.
Declarations
Funding
Not applicable.
Author’s Contributions
Takasumi Goto wrote this manuscript. Koichi Toda and Shunsuke Saito performed the procedure and proof-reading of this report. Katsutoshi Hirose and Eiichi Morii performed the autopsy of our patient. Yoshiki Sawa supervised this case report. All authors read and approved this manuscript.
Competing Interests
We have no competing interests to mention.
Consent for Publication
Informed consent was obtained from the patient’s family for its publication.
References
- Fulkerson PK, Beaver BM, Auseon JC, et al. Calcification of the mitral annulus: Etiology, clinical associations, complications and therapy. Am J Med.1979;66:967-77.
- Tsunekawa T, Kobayashi J, Tagusari O, et al. Infective endocarditis and pseudoaneurysm: Fatal complication of mitral annular calcification. Ann Thorac Surg. 2006;81:1881-82.
- Minardi G, Pino PG, Sordi M, et al. Infective endocarditis on mitral annular calcification: A case report. Case J. 2009;2:9072.
- Ross JD, Ura M, Kruger A, et al. Surgical management of mitral valve infective endocarditis with annular abscess and calcification in the setting of a leaking mycotic infrarenal abdominal aortic aneurysm: A case report. J Cardiothorac Surg. 2014;9:154.
- Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: A meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003;36:131-9.
- Lutmer JE, Yates AR, Bannerman TL, et al. Purulent pericarditis secondary to community-acquired methicillin-resistant Staphylococcus aureus in previously healthy children. A sign of the times? Ann Am Thorac Soc. 2013;10:235-8.