Case Report - Journal of Cardiovascular Medicine and Therapeutics (2018) Volume 2, Issue 4
Immature intrapericardial teratoma in twin pregnancy: A case report.
- *Corresponding Author:
- Jassim Abdulhamed
Department of Pediatric Cardiac Surgery Prince Sultan Cardiac Center Riyadh, Saudi Arabia
Tel: +966505469922
E-mail: dr_abdulhamed@yahoo.co.uk
Accepted date: November 28, 2018
Citation: Mohamed W, Mohsin S, Atiyah M, et al. Immature intrapericardial teratoma in twin pregnancy: A case report. J Cardiovasc Med Ther. 2018;2(4):19-21.
Abstract
Intrauterine pericardial teratomas are rarely seen. They are known to grow rapidly and can cause fetal hydrops and death. We report a rare case of fetal pericardial teratoma diagnosed at 33 weeks of gestation and was operated successfully in first week of life. The surgical results of symptomatic large pericardial teratoma is favorable.
Keywords
Pericardial teratoma, Teratoma, Cardiac surgery.
Introduction
Teratomas arising from the pericardium represent a rare cause of an intrathoracic mass. They can grow rapidly, leading to pericardial effusion and can result in to in utero cardiac tamponade physiology. Massive growth of tumor can compress the heart, leading to fetal hydrops and death. They constitute 18% to 25% of pediatric cardiac tumors. The tumor is composed of all three germ layers and may therefore contain calcium, bone and fat [1]. It is usually attached to the aortic root and pulmonary vessels by a pedicle. We report a twin pregnancy who underwent fetal echocardiography at 33 weeks, which showed a large intra pericardial mass most probably a tumor that was diagnosed to be teratoma post natally [2]. The other twin had normal fetal echocardiogram. No fetal intervention was attempted as there was no compression on the fetal heart with good biventricular function. The tumor was surgically resected after birth. Literature shows scarce reported cases on this rare entity hence we decided to report this case.
Case Report
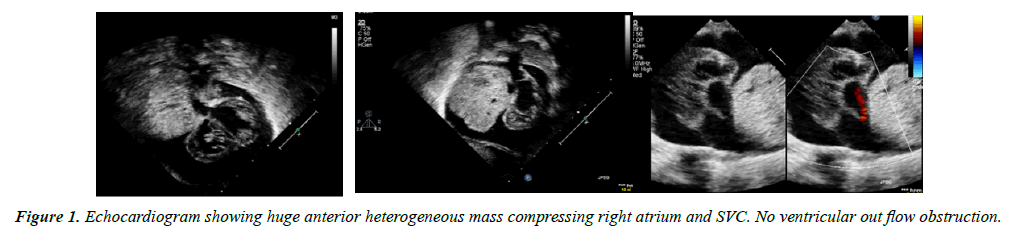
We report a Twin-1 baby girl who was born at 35 wks and 5 days, a product of in-vitro fertilization pregnancy to 36 yrs. old mother, with history of more than 10 years primary infertility. Diagnosed by fetal echocardiography at 33 weeks to have a large intra pericardial mas and pleural effusion, with no compression on the heart and normal biventricular function. The other twin had a normal fetal echocardiogram. They were delivered by emergency caesarian section. Both babies had good Apgar score after birth. Echocardiogram performed on twin-1 after birth showed the pericardial and pleural effusion to have increased from moderate to severe with no compression on Right ventricular out flow tract (RVOT) but mild compression on right Superior vena cava (SVC) (Figure 1). The patient was electively intubated and Echocardiogram guided pericardiocentesis was performed in Neonatal intensive care unit, 18 mls of Icteric pericardial fluid was drained and samples were sent for laboratory test including cytology.
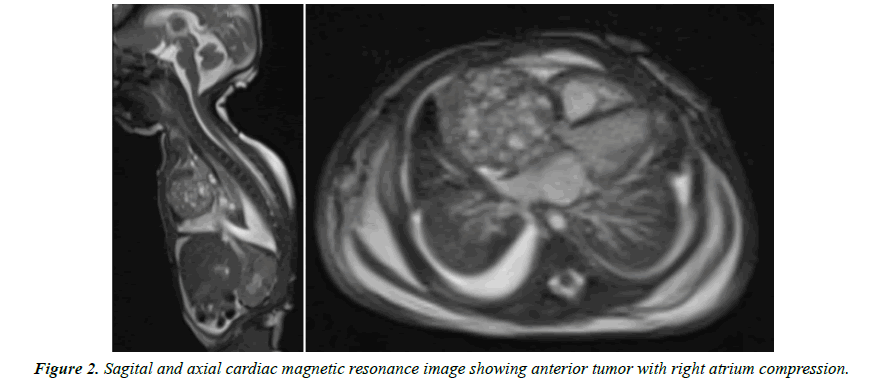
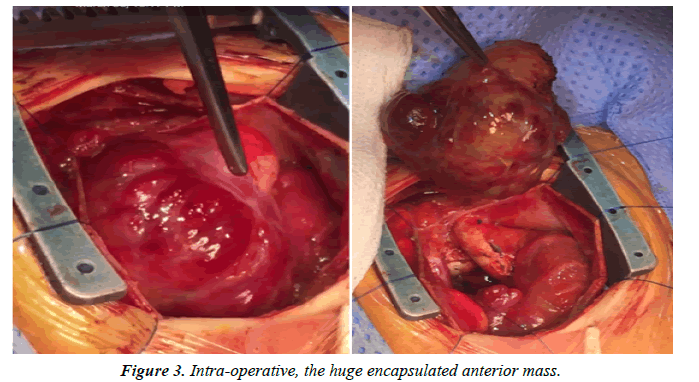
Magnetic resonance images (MRI) was done which showed well circumscribed large intrapericardial mass compressing SVC and RA. Later on, she showed signs of low cardiac output and was taken for surgical pericardial tumor resection on beating heart (Figure 2). Her intraoperative course went smooth and the tumor was found to be large in size 4.5 cm × 5 cm, arising from base of the heart, well encapsulated with no extension to the adjacent great arteries or mediastinum. It was completely resected (Figure 3).
She stayed in intensive care unit (ICU) for 5 wks. as she developed Chylothorax which required total parenteral nutrition (TPN) and octreotide. Her alpha-fetoprotein dropped from almost 70.000 to 20.000 in the first 2 wks. after tumor resection. Her Histopathology report revealed Large lobulated brown soft tissue tumor, measuring 4.5 × 4.0 × 3.0 cm. Her cytology confirmed the diagnosis of Immature teratoma.
The human chorionic gonadotrophin was monitored, and it remained less than 1. Her chromosomal analysis showed 46-XX an apparently normal female karyotype. She was discharged home after 5 wks. on full oral feeding with medium chain fatty acid formula with no pleural effusion ascites or pericardial effusion. Her six months follow up in outpatient department was unremarkable. She was asymptomatic, gained weight. Her alpha feto protein dropped further to near normal range, her echocardiogram showed normal heart with no remnants of tumor.
Discussion
Primary cardiac tumors in infants and children are extremely rare; with an estimated prevalence of 0.0017 to 0.28 in autopsy series. Due to this reason the published literature is scarce, and most knowledge is based on collections of surgical case reports [3]. Teratoma are rare primary heart neoplasms and are typically located at the base of the great vessels, accounting for signs of extrinsic compressions of these vessels [4,5]. Teratomas are commonly reported to have a pedicle with no encroachment on adjacent structure, thereby their resection usually is complete and did not usually endanger the adjacent structure [6]. The fetal and post- natal echocardiogram in our patient showed the pericardial tumor with heterogeneous appearance arising from right anterior heart border however, she underwent cardiac MRI for better delineation of the tumor and its relation to surrounding structures.
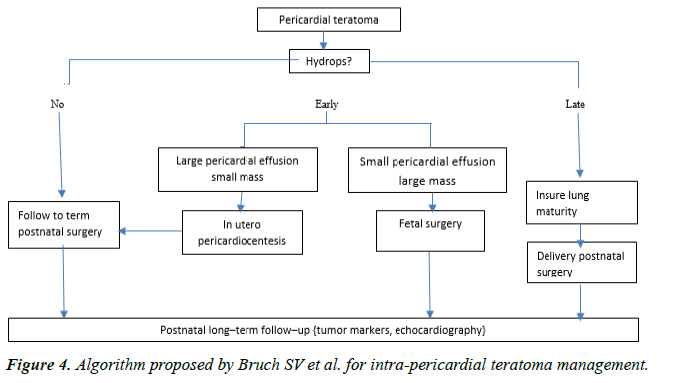
She was diagnosed at 33 weeks of gestational age after a fetal echocardiogram to have an intrapericardial mass with moderate pericardial effusion and pleural effusion, with no compression and no signs of low cardiac output. Since this was a twin pregnancy and there were no signs of low cardiac output it was decided to defer fetal intervention, following discussion with multidisciplinary team including cardiologist, neonatologist, obstetrician, literature review and parents counseling, so as not to risk the other twin. The management algorithm published by Bruch et al. also suggested the same. Bruch et al. concluded that in fetuses with no or mild hydrops it was safe to follow up with no fetal intervention, however, with development of Hydrops they suggested treatment with pericardiocentesis or in utero surgical resection [7] (Figure 4). Our patient’s status remained stable with no significant changes in the pericardial effusion, but the mother developed contraction and she was delivered by emergency caesarian section. Cardiac MRI was performed after birth and showed encapsulated tumor mass with no extension. The patient underwent tumor resection on the 2nd day of life.
Surgical resection is the treatment of choice and usually curative as these tumors are rarely malignant. Our case developed chylothorax, possibly as a postoperative complication needed fluid drainage, total parenteral nutrition and octreotide [7]. There are case reports in literature with pleural effusion but no reported evidence of chylothorax resulting from tumor compression of lymphatic system.
The MRI did not show any compression of lymphatic system by tumor mass. The histopathology showed immature teratoma. The tumor does not usually recur after resection even if not completely resected the patient was kept under follow up with cardiology and oncology for alpha fetoprotein and gonadotropin monitoring, as Teratomas can be mature or immature. On the 6 months follow up, the patient was asymptomatic, gaining weight adequately and her echocardiogram revealed no new growth, good ventricular function, no left or right ventricular outflow tract obstruction and no pericardial effusion. Her alphafetoprotein dropped to near normal range. Immature teratomas may have malignant potential, and hence post resection monitoring of plasma alpha-fetoprotein levels is necessary, which have diagnostic and prognostic values [8].
Another published Single center experience from Children’s Hospital of Philadelphia, from 2009-2015 showed 8 patients with pericardial tumor 6 of them found to have true intrapericardial tumor underwent surgical resection, one underwent fetal surgery at 24 weeks and one underwent ex-uterine intrapartum tumor resection with placental support at 31 weeks gestation with good over all result. The authors concluded that fetal intra-pericardial teratomas can be managed with serial follow up and treatment to be offered with onset of hydrops or increasing tumor size with reduced cardiac output [9]. They also stated that surgical resection in fetus is a possibility with good outcome.
Conclusion
Fetal intra-pericardial tumors can be followed serially with treatment advised if there is development of Hydrops or increase in severity of hydrops in fetal life. Otherwise it is safe to resect the tumor postnatally with no life-threatening complications to the patient or other twin.
References
- Cyr DR, Guntheroth WG, Nyberg DA, et al. Prenatal diagnosis of an intrapericardial teratoma: A cause for non-immune hydrops. J Ultrasound Med. 1988;7(2):87-90.
- McAllister HA Jr. Primary tumours of the heart and pericardium. Pathol Annu. 1979;14:325-55.
- Uzun O, Wilson DG, Vujanic GM, et al. Cardiac tumors in children. Orphanet J Rare Dis. 2007;2:11.
- Dimassi A, Dimassi W, Arnaout MS. Giant right ventricular fibroma co-existing atrial septal defect in a 15-year-old girl. Cardiol Young. 2009;19(6):630-2.
- Padalino MA, Basso C, Moreolo GS, et al. Left atrial myxoma in a child: Case report and review of the literature. Cardiovasc Pathol. 2003;12(4):233-6.
- Becker AE. Primary heart tumors in the pediatric age group: A review of salient pathologic features relevant for clinicians. Pediatr Cardiol. 2000;21(4):317-23.
- Bruch SW, Adzick NS, Reiss R, et al. Prenatal therapy for pericardial teratomas. J Pediatr Surg. 1997;32(7):1113-5.
- Roy N, Blurton DJ, Azakie A, et al. Immature intrapericardial teratoma in a new born with elevated alpha-fetoprotein. Ann Thorac Surg. 2004;78(1):6-8.
- Rychik J, Khalek N, Gaynor WJ, et al. Fetal intrapericardial teratoma: Natural history and management including successful in utero surgery. Am J Obstet Gynecol. 2016;215(6):780.