Case Report - Ophthalmology Case Reports (2025) Volume 9, Issue 3
Fraser syndrome: A rare case of syndromic cryptophthalmos.
Subhojit Chakraborty*
Department of Pathology, Malda Medical College and Hospital, Singatala, Uma Roy Sarani, West Bengal, India
- *Corresponding Author:
- Subhojit Chakraborty
Department of Pathology
Malda Medical College and Hospital
Singatala, Uma Roy Sarani
West Bengal, India
E-mail: scchocos@gmail.com
Received: 18-Mar-2024, Manuscript No. OER-24-129960; Editor assigned: 20-Mar-2024, OER-24-129960 (PQ); Reviewed: 03-Apr-2024, QC No. OER-24-129960; Revised: 10-Jun-2025, Manuscript No. OER-24-129960 (R); Published: 17-Jun-2025, DOI: 10.35841/oer-9.3.272
Citation: Chakraborty S. Fraser syndrome: A rare case of syndromic cryptophthalmos. Ophthalmol Case Rep. 2025;9(3):272
Abstract
Fraser syndrome is a rare ophthalmic presentation with autosomal recessive inheritance. It is observed in 1 in 200,000 newborns accounting for 1 in 10,000 fetal deaths. Mutation in the FRAS1 gene, retinoids, maternal vitamin A deficiency play a role. Globally only few cases are reported. A 20-day-old child born to non-consanguineous parents was referred from the newborn care unit He suffered from perinatal asphyxia. There was no maternal history of radiation, trauma, or drug exposure. On examination, bilateral complete cryptophthalmos, hypertelorism, and head circumference below the third percentile were observed. Additionally, syndactyly cleft palate, dysplastic ears, umbilical hernia, and anorectal defects were identified. Imaging modalities revealed a rudimentary globe, no orbital cyst with the absence of the crystalline lens in the left eye. Unilateral renal agenesis and cryptorchidism were discovered. He was managed conservatively. Three staged reconstructive surgeries with MMG were planned. Genetic counseling of parents was followed. Fraser syndrome can be diagnosed by antenatal ultrasound at 13 weeks of gestation. In families with previously affected children or stillbirths, ultrasounds are crucial at 14-16 weeks. Ocular treatment is multifaceted, determined by the degree of exposure to keratopathy and the presence of visual potential.
Keywords
Cryptophthalmos, Fraser, Renal agenesis, Rehabilitation, Genetic.
Introduction
Fraser syndrome has an estimated prevalence of 0.2 cases per 100,000 births [1,2]. Genetic factors involved include FRAS1 (4q21)/FREM 2 (13q13.3)/GRIP1, Hemicentin 1 (HMCN1), Furin, and Fibrillin 2 gene mutations [3,4]. Maternal deprivation of vitamin A and retinoids are also considered contributing factors [5]. Fraser syndrome is classified into complete, incomplete, and abortive types. Complete cryptophthalmos involves both upper and lower eyelids, while incomplete or atypical cryptophthalmos is distinguished by a poorly defined palpebral fissure, primitive conjunctival sac, a poorly developed globe and microphthalmos [6,7]. The abortive variety is also known as congenital symblepharon type, where the lower lid is normal but the upper lid covers and adheres to the upper cornea via a symblepharon [8].
Clinical diagnosis can be made using Thomas Criteria, which include cryptophthalmos, syndactyly, abnormal genitalia, and an affected sibling [7]. Minor criteria include cleft lip and/or palate, skeletal defects, and congenital malformation of the nose, ears, and larynx. Keratinization and vascularization of the cornea can occur, posing hazard to vision [6]. Other findings reported include facial asymmetry, upward slanting palpebral fissures, hypertelorism, tongue of hair extending from the anterior hairline to the forehead, brows, and upper-outer edge of the orbit, bilateral coloboma of the eyelid, broad nose and/or nasal bridge (8-84%), short neck, cleft lip and palate (11%), high arched palate (12%), airway abnormalities (laryngeal compromise) in 21-83% of patients, and other uncommon earnose- throat defects such as subglottic stenosis and laryngeal webs or atresia.
Case Presentation
Patient information: A 20-day-old male child was referred following a history of perinatal asphyxia. The gestational age of the child at birth was 36 weeks and birth weight 2.3 kilograms. He was the third child born to non-consanguineous parents delivered through vaginal route. There was no maternal history of genito-urinary infections or systemic illnesses, radiation exposure, trauma, or drug use.
Clinical findings: Gross examination showed:
• Bilateral microphthalmia, pseudo-hypertelorism, low-set ears, broad nasal bridge with bifid nasal tip, bilateral syndactyly on hands and feet.
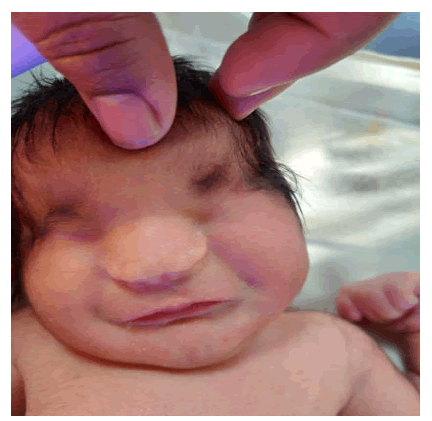
• Head circumference was lower than the third percentile (32.5 cm) (Figure 1 and 2).
Figure 1. Figure showing bilateral complete cryptophthalmos.
Figure 2. Figure showing syndactyly of left hand.
• Scalp hair extended in the left parietal region onto the forehead.
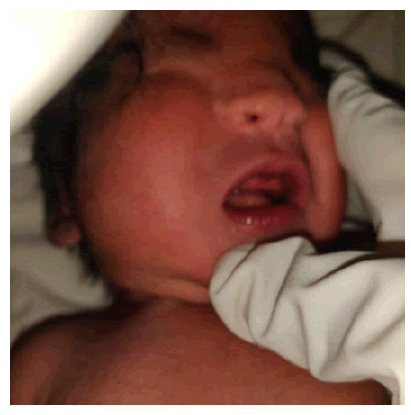
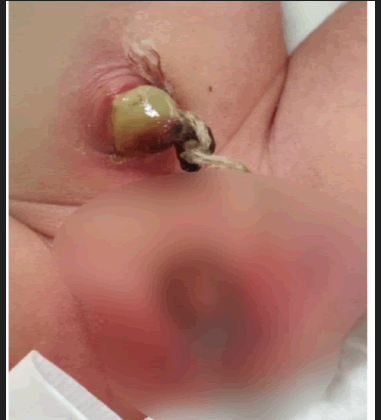
• Ambiguous genitalia, umbilical hernia, anorectal defects (Figure 3 and 4).
Figure 3. Figure showing bifid nasal tip, cleft palate, dysplastic ears.
Figure 4. Figure showing umbilical hernia, ambiguous genitalia, anorectal defects.
• Respiratory examination showed signs of respiratory distress and consolidation of the base of the left lung.
Timeline: This patient was hospitalized with fever and treated with piperacillin-tazobactam 150 mg /24 h intravenously (IV) in three divided doses and paracetamol 15 mg/kg/06 h IV. He was administered oxygen through nasal prongs. The child remained ill on the second day, but showed no temperature or respiratory distress. On the sixth day, he improved. Genetic analysis was not performed due to financial constraints.
Diagnostic assessment: Following investigations were done and the findings were noted:
• Ultrasound B-scan axial length of the right eye was 15.2 mm with a shallow anterior segment and of left eye was 15.7 mm with absence of crystalline lens.
• MRI brain showed shallow sulci, flattening of frontal eminence, and absence of meningo-encephalocele.
• MRI orbit showed dysplastic globes and absence of orbital cyst.
• Ultrasound of kidney and urinary bladder showed unilateral renal agenesis and bilateral empty hemiscrotum.
• Serum urea: 11 mg/dl, serum creatinine:1.2 mg/dl
• Skiagrams of skull, and wrist were normal.
• VEP showed delayed P100 latency.
Therapeutic intervention: The following treatment was initiated:
• Moist oxygen at 2-3 litres per minute
• Intravenous dextrose D-10 at 4 liters per hour
• Injection caffeine 30 milligrams intravenously in 20 milliliters of 0.9% normal saline over 20 minutes, tapered to 75 milligrams intravenously once daily.
• Injection of piperacillin-tazobactam 150 milligrams thrice daily.
• Infusion paracetamol 15 mg/kg/06 h intravenously
Follow-up and outcomes: Post-operative visits at the outpatient department were uneventful. The patient was referred to the pediatric surgical unit of a tertiary care center for further evaluation.
Discussion
Fraser syndrome can be diagnosed by antenatal ultrasound at 13 weeks gestation, showing hyperechoic lungs and renal agenesis. In families with previously affected children or stillbirths ultrasounds are crucial at 14-16 weeks. Genetic counseling was not done in this case due to financial constraints [5].
Differential diagnoses include Manitoba oculotrichoanal syndrome/MOTA syndrome characterized by a bifid nose, hypertelorisma, microphthalmia and trigonocephaly 2 which exhibits mental impairment due to a FREM1 gene mutation and triangular-shaped heads [4].
European research found 28-35% consanguinity in families There was no history of consanguinity in our indexed case [9]. Prenatal diagnosis can be made at 18th week of pregnancy with an ultrasound scan. Quantitative amniotic fluid estimation is indicative of respiratory system and/or urogenital tract defects [6].
Ocular treatment is multifaceted, determined by degree of exposure keratopathy and presence of visual potential. Prognosis is determined by the severity of congenital anomalies, particularly respiratory tract deformities, and mortality occurs often during the perinatal period [8].
Surgery aims at cosmesis and visual development, with aid of a multidisciplinary team. Eyelid reconstruction is done with oral mucous membrane grafts in combination with local myocutaneous or lid-sharing grafts [10]. Incomplete and partial cryptophthalmos require proper corneal surgery, mucous membrane grafts, and underlying globe repair.
Conclusion
Rehabilitation following surgery is challenging without agreed guidelines. Early surgery helps prevents amblyopia. In cases with painless eyes, surgery is deferred as more tissue is available for reconstruction. Orbital development should be considered. Genetic counseling of couples with affected children is advisable. In-utero therapy may be the final frontier for this potentially fatal disorder.
Informed consent
All relevant clinical documentation is provided with written informed consent from patient’s attendant.
Conflict of interest
Nill.
Financial interest
Nill.
References
- Fraser G. Our genetical ‘load’. A review of some aspects of genetical variation. Ann Hum Genet. 1962;25(4):387-415.
- Chaudhary A. Case report: Cryptophthalmos. IP Int J Ocul Oncol Oculoplasty 2021;7(1):99-101
[Crossref]
- Coulon P, Lan PT, Adenis JP, et al. Bilateral complete cryptophthalmos. Illustration with a case. Review of the literature. J Fr Ophtalmol. 1994;17(8-9):505-12.
[Google Scholar] [PubMed]
- Zehender W. Eine Missgeburt mit haütuberwachsenen Augen oder Kryptophthalmus. Klin Monatsble Augenheilkd. 1872;10:224-34.
- Francois J, Matton-van Leuven MT, de Rouck A, et al. Malformative syndrome with cryptophthalmos. Acta Genet Med Gemellol (Roma). 1969;18(1):18-50.
[Crossref] [Google Scholar] [PubMed]
- Slavotinek AM, Tifft CJ. Fraser syndrome and cryptophthalmos: Review of the diagnostic criteria and evidence for phenotypic modules in complex malformation syndromes. J Med Genet. 2002;39(9):623-33.
[Crossref] [Google Scholar] [PubMed]
- van Haelst MM, Scambler PJ. Fraser Syndrome Collaboration Group, Hennekam RC. Fraser syndrome: A clinical study of 59 cases and evaluation of diagnostic criteria. Am J Med Genet A. 2007;143(24):3194-203.
[Crossref] [Google Scholar] [PubMed]
- Thomas IT, Frias JL, Felix V, et al. Isolated and syndromic cryptophthalmos. Am J Med Genet. 1986;25(1):85-98.
[Crossref] [Google Scholar] [PubMed]
- Barisic I, Odak L, Loane M, et al. Fraser syndrome: Epidemiological study in a European population. Am J Med Genet A. 2013;161(5):1012-8.
[Crossref] [Google Scholar] [PubMed]
- Saleh GM, Hussain B, Verity DH, et al. A surgical strategy for the correction of Fraser syndrome cryptophthalmos. Ophthalmology. 2009;116(9):1707-12.
[Crossref] [Google Scholar] [PubMed]