Review Article - Journal of RNA and Genomics (2022) Volume 18, Issue 1
Florida pain ethics problems in hospitals while having the mu-opioid receptor OPRM1 gene with the A118G SNP.
Orion V Erickson*
Department of Journalism, Santa Fe College, Gainesville, Florida
- Corresponding Author:
- Orion V Erickson
Department of Journalism, Santa Fe College, Gainesville, Florida
E-mail: orionerickson2000@gmail.com
Citation: Erickson OV. Florida pain ethics problems in hospitals while having the mu-opioid receptor OPRM1 gene with the A118G SNP. J RNA Genomics. 2022;18(1):1-18.
Abstract
My name is Orion Voss Erickson. I'm a 44 year old native Floridian. I grew up in Dunedin, FL, USA. I originally received a hip replacement right after my first degree in college, when I was around 22, due to avascular necrosis. This first surgery was followed by several more surgeries over the next twenty years that developed into a disturbing pattern. A pattern that has become a culture. A culture of pain and lack of compassionate care directly after surgeries. Recently, I found out that my opioid receptor gene had the characteristics of requiring more pain medication compared to the rest of the population. After several years of experiencing many painful surgeries and having to tolerate the stigma of being a former IV drug user, I feel obligated and compelled to tell my story so that others can avoid the trauma that I have experienced
Keywords
A118G, ORPM1, Pain management, Ethics, Addiction, Hospital ethics, Orion Erickson.
Introduction
My name is Orion Voss Erickson (Figure 1). I'm a 44 year old native Floridian. I grew up in Dunedin, FL, USA. I originally received a hip replacement right after my first degree in college, when I was around 22, due to avascular necrosis. This first surgery was followed by several more surgeries over the next twenty years that developed into a disturbing pattern. A pattern that has become a culture. A culture of pain and lack of compassionate care directly after surgeries. Recently, I found out that my opioid receptor gene had the characteristics of requiring more pain medication compared to the rest of the population. After several years of experiencing many painful surgeries and later having to tolerate the stigma of being a former IV drug user, I feel obligated and compelled to tell my story so that others can avoid the trauma that I have experienced.
My psychiatrist had me take a genomics test to determine which medications work best for my body which is known as pharmacogenetics. According to a 2020 article in Genet Med.
“Implementing pharmacogenetic testing in the clinical setting has the potential to improve patient care by decreasing failed treatment attempts due to medication ineffectiveness and/or adverse effects and by increasing effectiveness of improperly dosed medications” [1].
This is how I found out my μ (mu)-opioid receptor gene, OPRM1, that mediates the action of morphine, has the Single-Nucleotide Polymorphism (SNP) A118G or G-allele. And this SNP affects the gene’s function. In this particular SNP variation, “OPRM1 G carriers, compared with AA homozygotes, showed an overall reduction of baseline m-opioid receptor availability in regions implicated in pain and affective regulation” [2]. Which is kind of like saying my opioid receptors’ misfire and I’m not getting the full benefits of opioids. Out of the 43 identified SNPs in the OPRM1, the most studied is the A118G [3]. The conclusion of the article. The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: a systematic review and meta-analysis from pain physician was, “The results indicate that among the genetic SNPs we studied which include those affecting analgesic drug metabolism, transport of analgesic agents across the blood-brain barrier, and their activity at target receptors and ion channels and in the modulation of neurotransmitter pathways, the A118G allele variant of OPRM1 has the most potent influence on pain management of postoperative patients. Opioid receptor gene information may provide valuable information for clinicians to properly manage the analgesic use of opioids individually for better pain management.” Not to mention what the meta-analysis confirmed: out of 23 studies (a total of 5,902 patients), “The results showed that human mu-opioid receptor gene (OPRM1) 118G allele variant carriers consumed more opioids for analgesia.”
After understanding pharmacogenomics a little more, I could finally use this test to avoid humiliating, degrading responses to my pain and finally get some pain control after surgery! I wouldn't have to sit through endless surgeries in excruciating pain! Dealing with multiple hip surgeries, around 17 out of 20 (all in Florida), I could not get the correct amount of pain medication even on the day of surgery. When I did get the correct amount of pain medication that worked for my body, I started to receive pain relief. It's that simple.
But let's get this straight from the beginning, right now I'm not referring to pain medication they give you a few days later when you leave the hospital. I'm talking about waking up in the Post Anesthesia Care Unit (PACU) screaming in pain. Then the general scene would devolve: the nurse would call the doctor to raise my pain medication and they would just figure I'm lying and stop short on pain relief. I’m left in excruciating pain in the recovery room and wheeled to my room. Then it gets handed off to pain management who has the same disrespectful attitude of not believing I'm in pain. I average three days to a week of no sleep in pure agony with each hip surgery. This keeps happening, 17 out of 20, or specifically one doctor out of many.
One doctor, this is not ok
I know this may sound like a generalization, so I was going to detail each surgery. But since this has been going on for so long, I'm going to be realistic and refer to the multiple surgeries one by one from last year, 2020.
Surgery 1
About a year after my genomics test, April 2020, I developed an infection in my hip. My primary doctor thought I had an enlarged hernia, until I saw a specialist. It was not a hernia, but rather an infection. His office was across the street from the hospital, so I just hobbled to their Emergency Room (ER). I finally found a doctor who would take my case. They performed a biopsy and found a candida infection. So we scheduled surgery to remove my hardware. As we are discussing the surgery in detail, he informed me that he's not taking out the stem, just the other hardware. He told me this with surgery starting in minutes. In previous surgeries, my orthopedic surgeons told me that all hardware, including the stem must be removed, otherwise the infection would attach to it again. This was my infectious disease team of doctors’ stance as well and they were wringing their hands in disbelief as they rolled me into surgery without any other options or doctors to take my case, I went into surgery hoping for the best.
As usual, I woke up in the PACU screaming in pain. The multiple calls to the doctor to up my pain meds were not met with any sort of pain relief. Definitely not under the 50% pain threshold. My blood pressure did not go down whatsoever. My oxygen levels did not change. I was left in 100% pain then wheeled to my room. Since I wasn't able to discuss anything with pain management before the surgery, I could tell the pain management doctor in my case definitely had her negative opinion of me. It's kind of hard to present your case about genomics while in extreme pain, but I tried my best. I could see her unwillingness to believe what I was saying. I pleaded with her about the pain and in my disbelief she responded, word for word, "I'm not going to start throwing opioids at the problem!" Directly after surgery?! She had given me a very low dose of morphine. I told her that is very low and it’s not working. She may have gone up a little more on morphine, but I may have just been in shock that she gave me only 4 mg; which didn’t give me any relief.
I was cold sober; with raw, nonstop pain. Pain doesn’t hide and you can’t hide from pain. You can’t clock-out or take a break from pain. And pain doesn’t identify injustice. All you can try and do is distract yourself long enough to forget about the hell you’re currently in.
Let's take a step back here; I just had a major hip replacement with a current infection. This IS the time you DO use opioids for pain. I’m not some guy from the ER complaining about “back problems” with no imaging. I just had a hip revision, which is surgery to remove my hip hardware. This isn’t some minimally invasive anterior hip procedure; they made a giant footlong cut and pulled out my hip hardware. The pain management doctor then proceeded to prescribe a lidocaine patch and gabapentin. Gabapentin has shown limited analgesic efficacy in many case studies, specifically regarding hip replacements [4]. That didn’t help. According to the article Successful Pain Management for the Recovering Addicted Patient, “The goal of chronic pain treatment in addicted patients is the same as individuals without addictive disorders-to maximize functional level while providing pain relief” [5]. This doctor knew exactly what she was doing. If the goal is to ‘maximize functional level while providing pain relief’, then they failed.
Nothing has changed
The pain doesn’t stop after the sun goes down. Pain doesn’t care if you’re sleepy. As hard as I could scream, it did not help the pain. I would call my mom’s phone every few minutes just to hear her voice; focus on her voice to soothe this raw pain. She would repeat that she loved me. I would hold onto those feelings, all her love and comfort as if it were a womb. This would make everything safe. I may have escaped the brutal reality for a brief moment. Seconds I’ll take.
Then after a sleepless night of being ignored by multiple phone calls from my nurse pleading with pain management for something to stop me moaning in pain, the same pain management doctor greeted me the next day with an accusing, "What's going on with your face?” My body's physiological response to this pain developed this blinking tick and my mouth was grinding so hard, I probably looked like a cow chewing cud. I didn't realize I was doing that until she pointed it out. Then I realized something's seriously wrong. "The pain!" was my response to her. The doctor got real quiet after that. I think she may have realized what happened. This or my pain was never addressed or come to any solutions for the remainder of my stay at this hospital. Granted, three days after surgery, the pain usually goes down and can be stepped down. But when the baseline for my pain is way off, I still have an infection and my opinion isn’t accounted for; you can imagine the painful problems that may arise. Not to mention, I can’t take back those three days of hell!
My stay in the hospital was about two months for IV antibiotics. During this time, there was an internal struggle with Infectious Disease getting my surgeon to remove all the hardware still in my hip. He just wouldn't do it. No other doctor would take my case. It's also very hard to change surgeons, especially if the surgeon has already performed an operation. Most doctors are reluctant to take on new cases or stepping on other doctors toes, so much so: this happens. In the meantime I was still very under-prescribed and dealing with constant pain, stress and lack of sleep. Obviously, this is not the best condition for an infection to heal.
Let's have a discussion of how you feel as a human being after being ignored multiple times screaming in pain, with the solution in the same room. The same room that is supposed to be SAFE. It doesn't give you the best outlook on humanity. It gives you a sense of truly being alone. Helpless and hopeless. In the middle of a professional community that is supposed to protect me. I started questioning myself: Am I completely worthless? I already struggle with confidence. How can another human being do that to someone? Obviously, they don't think I'm important enough to listen to. They had to be breaking some kind of ethics code.
Surgery 2
At this point, my mother had flown down to help with my medical situation. While I was in the hospital I made some phone calls to set up an appointment with a private pain management doctor who also worked at the hospital. This was in hopes to humanize me and have a talk about my problems with pain. I managed to make an appointment for when I got out, but only the nurse practitioner was there to see me. She listened to me, wrote a script and I felt like a positive relationship with the main doctor was in the forecast.
About three days after I was discharged, my home health nurse came and saw how much pain I was in, she became very concerned. She called my doctor saying they need to up my pain meds stat. After her leaving, I almost passed out and it got so bad my mom called an ambulance. The EMT took a look at my hip and could tell it had popped out. On my way back to the hospital! I got there and I maybe saw a doctor, but I believe it was all nurses. I sat in a hospital bed in a lot of pain and no one would prescribe me anything whatsoever. They do have my charts and could see my multiple hip replacements. I sat there moaning in pain for hours. I overheard a nurse say that I was just trying to get drugs. That would be a serious addiction and a painful way of doing it. Once they realized they had to do something, they performed surgery within the week.
This time I woke up and something was different. Pain didn’t hit me with a ton of bricks. Confused, I started asking when they’re going to do the surgery. The present nurses said my hip had been replaced. I was completely bewildered! I kept asking the nurses if they were joking. Since the surgeon was long gone, I couldn’t get any specific info on why this was happening. Something like this doesn’t change overnight. For me not to be screaming for more pain medication in the recovery room was a miracle. Hopefully my team of doctors can use the data from the required strength of medication it took for my perioperative pain as a base; to receive adequate pain control; because I know it must have been high. But somehow there is a disconnect between the correct opioid analgesia received directly after surgery and the amount you receive when pain management takes control; which is the same day of surgery. There are evidently no working opioid system guidelines or analgesic ladder in place for addicts. If so, I should have received more pain medication after surgery than before. As of now, I have fallen off the ladder. Or as Dr. Josh Bloom, who is the American Council on Science and Health’s (ACSH) Director of Chemical and Pharmaceutical Science, points out,
"It is now common knowledge that you are just about as likely to get opioids in an emergency department as at a Dairy Queen" [6,7]. And this was a 2019 out-of-state article written specifically about one of the first of many draconian prescribing bills, HR217, coming out of Florida.
I never did find out what happened to wake up painless. I’ve stressed with every surgeon over the past twenty years the importance of dealing with my pain, which I assume has been looked at as drug-seeking. But when asked about a pain-block for my hip, I would always get the same answer, “It can’t be done.” So far, I can’t find any literature as to why not, but I do know there are many factors involved.
Whatever I was on when I woke up painless and surprised, wore off. That familiar feeling I kept telling myself should not be familiar, had become familiar again. I kept denying the past in hopes of forgetting or at least muddling some of the details. My confidence in stating something that has so far been treated as a lie over and over, just starts to dwindle my own self-worth. They seem to have the same mantra: Opioids’ bad!; in a time they are needed most.
My x-ray looked like the surgeon grafted or welded a new spacer (temporary hip) directly to my hip. All I know is something wasn’t right because every movement was excruciating. I also had to wear a medical brace around my upper torso so my spacer wouldn't pop out again. I was not doing walker parkour or anything remotely extreme. It popped out while I was sitting on the couch with my mother. This new spacer was so painful! The brace was hard to get comfortable in bed, plus any movement was very painful. Does this guy know what he's doing? He's already ignored Infectious Diseases' recommendation to take the whole hip out. I had the feeling they didn’t really care more than charging my insurance.
Then I remembered I had a private pain doctor. But I never saw the guy. I was immediately put on a low pain medication the same day of surgery. Since he was my pain doctor, no one would change anything no matter what I said. This happened the whole stay. It turns out he was on vacation and I was abandoned with no pain doctor. I almost lost it. I was about to get up and probably do a face plant since I didn’t have a say or choice in anything at this point, then the hospitalist came in. He kept saying he was so sorry he couldn’t do anything, but he said he’d at least change the frequency of a medication. That never happened. I wrote a grievance and detailed everything.
I had to find another solution, but I felt like I was stuck. Insurance would just tell me to call surgeons and see if they'll take my case. I called some surgeons and I had to make an appointment. I can't see them while I'm in the hospital. Plus, I literally do not have the time to make appointments that can be months out, with multiple surgeons, just to roll the dice, in the middle of a nasty infection stuck.
Surgery 3
My mother called with exciting news that we found a surgeon that will take out all the hardware and this painful stem! Her friend had used this doctor and he’s known for specialty cases. And the surgeon was in Tampa, Florida which was perfect because my parents live around Tampa. They could help me when I'm out, because it's tough with just a walker, not to mention pain. We got an appointment in a few days. My father drove down to the South Florida hospital and rescued me. What a relief! Now I have a fresh doctor at a prominent teaching hospital and I can have a chance to talk to him directly about what is going on and explain my genomic problem and the problems I’m having with pain management doctors.
Our conversation with the surgeon and fellow came up with a great game plan. The surgeon and the fellow were professional. It was scheduled for a few weeks and they were going to get me in sooner if possible. I think we found the right guy!
I waited until the end of my appointment to discuss my pain issue. By that time the fellow had left and it was just me, my father and the doctor. I delineated my genomic disorder and he said word for word, "It just looks like you're trying to get pain medication." I responded that when I get enough pain medication, I'm ok. I could tell he wasn't taking me seriously. Then he proceeded to turn to my father and give some speech about the dangers of opioids. I felt like a teenager and my father was talking to the principal about something bad. I was 43 and, at least before these surgeries, I looked much younger. So I don’t know if looking young is in this equation of distrust, along with being labeled an IV drug user. I could tell I failed his morality test.
I was so livid, I didn't really catch too much more. But he said it in a way that resonated with an attitude of, "You're in pain until we decide you are not." Unfortunately, all he could focus on were the negative and I felt like everything from here on, I wasn’t going to be taken seriously. My father wheeled me out of the office in their wheelchair. My heart sank. All I could see was red! Dad had to get me to the car quickly because I was so upset that I was loud and cursing. It takes a lot for this introvert to get upset, but I made it out without causing too much of a scene. A five hour drive from the last hospital with such high hopes, made this disappointing news that much lower.
My family and I discussed our situation. We came to the conclusion that this is our only option. I would have to discuss my pain issues with pain management. I was trying my best to be optimistic. I tried finding a pain management doctor who also had a private practice, so I could have a serious talk with them. But I could not find or call a private pain management doctor that worked at the hospital anywhere.
I had to go to the hospital early because the infection was getting worse and the pain between that and the “experimental” spacer pain was unbearable. After the usual waiting times in the ER, I got a bed. I ended up talking to one of the ER nurses about my concern with being under prescribed in the most dire moments. I discussed my genomic test and the issues I’ve been having regarding opioid analgesia. She listened to me. She listened to me! First time! She recommended Ketamine as an alternative. I wasn’t aware of analgesic properties of a dissociative, but I’ll try anything that’s not an opiate that would help with surgical pain! The authors of the Revision of expert panel's guidelines on postoperative pain management have concluded: “Intraoperatively, small doses of ketamine in patients on general anaesthesia are recommended in the two following situations: 1/ surgery with high risk of acute pain or chronic postoperative pain; 2/patients with vulnerability to pain, and most particularly patients taking long-term opioids or addicted to opioids” [8].
After a strange mix of covid, blood and screaming in the ER, I made it to floor seven. The orthopedic floor. The ortho floor is where it’s usually a rotating joke with the nurses, that I'm the youngest guy there. I started having a detailed conversation with my new pain management doctor. I mentioned my genomic problem with opioids. She listened to me and we were going to come up with a plan. But I quickly realized I was stuck in the same situation, when the same doctor told me it was “...illegal to go up more than 5 mg on my oxycodone.” I was hit with flashbacks from the last hospital: pain, degradation, lies and utter hopelessness. Then there was an issue with my last script of morphine that got entered into the e-forcse, Florida’s prescription drug monitoring program database completely wrong. My private pain management doctor from South Florida told me he was writing a script to take three morphine sulfates a day. Unbeknownst to me, the bottle had two times a day misprinted on it. But it was an easy explanation. I explained that all my medications I brought in were for 30 days. Yes, I brought in all my unused pain medication. And just like those medications, this medication was meant for 30 days as well. The quantity, 90, equaled taking the medication exactly three times a day for 30 days. Pain management decided it was a 45 day supply of taking two a day. They knew that was wrong. I had three medications from that doctor for 30 days. So, here I am with a massive infection, with an extremely painful spacer and they are giving me less pain medication than I was prescribed outside of the hospital?! They ended up going up 5 mg of oxycodone. I was still in constant pain. They did not help explore any of the pain alternatives previously discussed. Since I had checked in earlier, I was just painfully waiting for surgery. Waiting eleven days while arguing with pain management to no avail. My hip-revision involved taking out the hard to get metal stem. It was so difficult to remove that they had to break my femur. I respect and thank the surgeons for taking on and removing all the hardware, even if they had to break my femur. But please be completely honest with me before the surgery so I can try to prepare mentally. I have the right to know that I will be under-prescribed, so as to prepare a way to cope. Then again, I also have a right not to be in pain. Don’t I?
Turns out: "According to international human rights law, countries have to provide pain treatment medications as part of their core obligations under the right to health; failure to take reasonable steps to ensure that people who suffer pain have access to adequate pain treatment may result in the violation of the obligation to protect against cruel, inhumane and degrading treatment" [9]. This is not being followed. My hospital surgeries were cruel, inhumane and degrading. Also, the United Nations (UN) Universal Declaration of Human Rights (UDHR) is clearly being violated. Or more specifically: Article 1, 2, 3, 5, 6, 7, 9, 12, 19, 21 SEC 2, 22, 25 SEC 1, 27 SEC 1, 29 SEC 3 [10]. This was originally designed to help third-world countries and a response to the ethical horrors of World War II. Not to force the hand of the leader of the free world. There are other similar guidelines like this that challenge the misconceptions of things like “the use of opioid analgesics will trigger a return to uncontrolled opioid use” [11]. To try and point out “...inadequate pain control may lead to relapse, as the patient may attempt to manage their pain through illicit drug use” [12]. When someone is irresponsibly left in pain, they are leaving the hospital with a gun. Not a loaded gun. Street pain relief is the bullet that gets put in the gun for a Russian roulette spin.
Out of sight, out of mind
I received a phone call while in the hospital from the pain doctor I first wrote a grievance about. His office said they were not going to charge me anything from the last “visit” in the hospital and offered free appointments. I said I’m done with that hospital and hung up. I was impressed that I did cause some change for the better, but I can’t keep shaming doctors. The damage had already been done and now I’m at a hospital five hours away. This doesn’t help my case now.
The surgery day arrives and I get wheeled to the surgery waiting room. I’m not sure what I talked to the surgeon about, but it was probably trying to convince him again that I need higher pain medication after the surgery. All these talks about this issue are just looked at as drug-seeking. It’s a vicious cycle of under-prescribing, then blaming me for drug-seeking although I’m in pain and actually need pain medication for pain since them under-prescribed me in the first place. My approach isn’t working.
Something has to change
“More than 80% of surgical patients experience postoperative pain, the under treatment of which results in a variety of negative consequences and remains a considerable problem worldwide. Persistent Postsurgical Pain (PPP), the incidence of which being up to 30%–50%, originating from surgical intervention and acute postoperative pain without adequate management, has major negative effects on the individual’s quality of life and places a heavy burden to the society disturbing millions of people globally and challenges for perioperative physicians. The severity of postoperative pain has been suggested as a key risk factor of PPP, and adequate analgesia for acute pain during the early postsurgical period may be associated with less incidence of PPP” [13]. There needs to be some kind of recognition of serious surgeries that need high pain medication no matter what they think of your lifestyle. After surgery, my screaming in the PACU wasn’t answered. I knew this was their attitude. I was put on a Patient-Controlled Analgesia (PCA) pump. By the time they got it close to eight on the pain scale, it was day three. That’s typically when they take you off the PCA. I somehow talked them into leaving me on one more day. And of course this nasty nurse came in and said condescending comments about being on the PCA for an extra day. That’s not helpful. I may have mentioned the broken femur.
The fear of stepping down to pills really got me anxious. I was taken off the PCA and received the same mg in pills as I was on before the surgery. I complained for two weeks and nothing changed. It’s like they’re executing an advance directive I signed to “stay in pain.” I never agreed to limit my pain medication. The focus should focus on my pain.
Like the last hospital, I started my grievance. It reflected what happened and is happening. I still had an active infection that keeps causing abscesses. That’s why I’m still in pain! When I started waiving the grievance around, it eventually got the attention of the head pain management doctor. I told her I had been complaining about being in pain for almost two weeks, then I handed her my eight page hand written grievance I worked so hard on. She read a few sentences and said they would increase one of my pills. And they did. Too little too late is an understatement. The damage had been done. I’ll later kick myself for not turning in that grievance to be documented.
I knew I’d be at this hospital for at least another six weeks for the IV antibiotics.
But now I’m stuck in a catch-22. If the pain starts to go down, I can slowly taper off this pain medication. If I do that, the next time I’m here, my pain medication base would be low again. I can’t go through that process of arguing with pain management while being in excruciating pain. Unfortunately the pain didn’t go down. The highest amount I was prescribed was just slightly more than my base when I was completely opioid naive. I know this because I’ve made a conscious effort to come off of previous pain medications. I was prescribed a high amount for several years.
It turns out my G-allele is also known for processing alcohol into more dopamine than most people [14]. This means I feel great when others are intoxicated. I’m still intoxicated, but the dopamine gives me a more positive euphoria. Or to be more specific. “The 118G allele, which encodes an amino-acid substitution [Asn40Asp] in the N-terminal extracellular loop of the receptor, confers a higher striatal DA (dopamine-activation) in response to alcohol regardless of whether it occurs in the context of other markers within its haplotype block or not” [15]. The same may be similar with drugs. Once I understood my body a little better, down to the cellular level, I took a step back and looked at my behavior to combat these issues. I knew there was a better way to live once I was able to manage my pain with tylenol. The stigma and the anxiety of running out of my prescribed pain medication and risking horrible withdrawals is something no one wants to be a slave to. So I did. I went to a safe place to go through monitored withdrawals that anyone, including the Pope, would have if prescribed opioids only for a month. It was hell, but I had to do it. Then I decided to stay and live in a sober-living house to put up the necessary checks and balances I needed at the time. I felt strange and I couldn’t sleep for three months, but I pushed on. I got a humbling job bussing tables. I eventually slipped a few times, but I learned from that, picked myself up and applied it to my recovery. I even had surgery and was put back on opioids, then returned to the same place to withdrawal and live in sober-living again. I know what it’s like not having to rely on a substance and I miss that. But when they are needed, they are needed.
Currently, I give my parents control of my pain medications. That works best for me since I know I can’t take the meds more than prescribed; even though I’m in pain all the time. I’m prescribed a pain medication that has a four hour half-life and it’s prescribed every eight hours. The outpatient pain management doctors prescribed exactly one-quarter of the amount of opioids I was previously prescribed for months. So I had to battle withdrawals right out of the hospital. Thanks to Florida statute chapter 893 drug abuse prevention and control, outpatient pain management cannot go over 90 mg of morphine a day [16,17]. That number was recommended by the CDC17, then when several states decided to make mandatory 90 mg morphine laws, the CDC retracted and said, “The guideline does not support abrupt tapering or sudden discontinuation of opioids. These practices can result in severe opioid withdrawal symptoms including pain and psychological distress, and some patients might seek other sources of opioids. In addition, policies that mandate hard limits conflict with the guideline’s emphasis on individualized assessment of the benefits and risks of opioids given the specific circumstances and unique needs of each patient” [18]. Pain management doctors are even cutting people off high doses as we speak. It’s like they’re setting us up to fail. May be they just assume I’m going to get some fentanyl for the twelve-hours I’m in pain over twenty-four hours. It’s simply unrealistic.
My biopsy results came in and they found a pretty nasty, slow growing infection: nontuberculous Mycobacterium abscessus; along with Corynebacteriumstriatum. But no candida grew this time. When a doctor told me that Mycobacterium is “kind of a bitch” to treat, I knew I was deep in it and this horror is going to continue for some time. Mycobacterium is known for being multi-drug resistant, with a slew of other bad things [19].
I spent two to three months in the hospital on IV antibiotics. The infection was still active when multiple abscesses formed where the drainage tubes had been from surgery. One ended up closing, but the other opened and started draining. The surgeon decided to put a wound vac on my draining abscess.
Since this was a teaching hospital, I would occasionally see a doctor with a group of students. They came to visit again and I discussed with the head teaching-doctor my problem with receiving less morphine than I was prescribed by my private pain management doctor. All I needed to do was get a copy of the original script or what the script says before the pharmacy entered it into the e-forcse database. The doctor and her students were going to handle this. They could tell I was in pain and we had found a solution to help mediate this problem; or at least help find a better base to start. Not too long after that, the same nurse from before walked in with pain management right behind her. In her condescending tone, the nurse told the doctor that it’s not the hospital's job to help correct the script. The doctor didn’t miss a beat and totally agreed with her. Cancel help stat! It’s almost like it was rehearsed. I really don’t know what this nurse's problem is. I thought she was just having a bad day the first few times. But she was trying to score points with pain management. And each point was getting exponentially agonizing. Ever since I wrote my long grievance, pain management seemed to be trying to discredit me; which is evident in my medical “records”. This nurse would sometimes “forget” something in my room, or at least that’s what she said when she kicked the door open to catch me doing only God knows what she had imagined. I was shortly discharged without my pain medication being corrected.
The pain management doctors have the final say on behalf of my pain, with no checks and balances. Now surgeons can hire a pain management specialist, to decide if I’m morally allowed to take opioids. If not, my opioids are under-prescribed. And this “specialist” would determine which screams was actually pain. Evidently, I don’t know my own body. The same day of surgery. I must be lying about it? How does this go unchecked?
It’s not like I can get help from the state. Our Florida attorney general, Joseph Ladapo, who is a cardiologist, with no infectious disease training, in the middle of a pandemic, is known for being “unprofessional” and won’t wear a mask even in front of a cancer patient [20]. This is how things work in Florida. It’s like a reality show.
For any of this to change, it needs attention. Unfortunately, in today’s society, the only thing that really gets people’s attention is money. In the medical community, lawsuits get attention. Since pain is an inherently subjective experience, I imagine it’s hard to prove “without a doubt” in court about said pain. The latest lawsuit involving not enough pain medication, that actually won, was about 20 years ago and that resulted in death of an 85 year old man [21]. It seemed a far stray from malpractice standards. Although, I just found a new lawsuit and it involved the suicide of a woman’s father from being cut off from his pain medication [22]. But that lawsuit would never see the light of day in Florida. Without a way for anyone to prove they are in pain, this cycle will remain unchecked and people will continue to suffer.
Surgery 4
My surgeon recommended a “wash-out” or irrigation, where he and his team would cut out the infected muscle and tissue that had developed inside my right femur/hip. All to help heal the infection.
I was ready as I was wheeled into the surgery waiting room. This time I had my Genomic Report gripped tightly in my hand. I started talking to the anesthesiologist about my report and how it related to my pain receptors. She mentioned a genomic study where Asians had problems with anesthesiology. We discussed how the g-allele I carry is more prevalent in Asians. Then we discussed how unfortunately she was not my anaesthesiologist. I have been told in the past that the anesthesiologist is the doctor that's in charge of pain control directly after surgery. So I started to explain to the correct nurse about the document in my hand and she brushed me off as she took it and said we already had it on file. It was later evident I didn't make the best impression with my anesthesiologist.
My hip and femur were burning! By the time I realized, I couldn't believe I was stuck in the same situation! This time, panic had set in quickly! Knowing how this has happened in the past, I knew what to expect. I hold a little optimism each time (or I at least tell myself it will be different), in hopes that someone will listen to me and treat me with a level of respect this time. A level of respect above dogs. Even though most dogs with owners are helped when in pain, until they are out of distress. Or at least “taken out of misery”. As with any human being, I did not stop trying to break this perpetual cycle of avoidable torment.
My attending nurse in the recovery room had dehumanized me from the get go. The racing thoughts of the past negative outcomes hit me at once. My screams were met with, “Does that noise you're making help?” Yelling from pain is even understood by my dog. Yet, why is it foreign to a nurse? Not understanding the most primal human emotional call for help, is in and of itself an example of dehumanization; which is far from an exaggeration. The constant phone calls the nurse made to the doctor about pain control were met with leaving me in excruciating pain. I was wheeled out of the recovery room pleading with the nurse that I was still in pain. The last thing I could remember exclaiming was, “You can’t do this!”.
How have these basic human conditions been scapegoated psychologically?! The only thing I could compare this to is similar to what cognitive steps our brains take to dehumanize people during times of war [23]. We are in the middle of an opioid epidemic or rather a drug war. In hospitals, instead of drug and alcohol addiction being treated as a medical problem, it’s still, to this day, being treated as a moral problem. I’m just seen as an IV drug user. Seen as the problem and the enemy. Enemies are seen as evil and evil drug users cannot be trusted. Seen as a cancer to our society who doesn’t deserve the same care as thy neighbor. Black and white. Not to examine the shades of gray that encompasses the yen and yang of our culture, just black and white. Good and evil [24]. This makes communication difficult.
I get to my hospital room. The surgeons had just removed some of the infection inside my hip, including infected tissue and muscle. My hip was constantly burning in pain and I let everyone know! By this time it was late at night and doctors were not around. I could tell my nurse had some compassion as he got frustrated trying to get Pain Management to call him back. Since my hands were tied, I did what I knew my only option was: call my parents.
This treatment as a whole was really affecting my parents, especially my mother. They have been with me for every surgery including the outcomes of post-surgical pain; mainly over the phone because of the COVID limitations and hours. It has got to be frustrating for them to hear their only child scream in pain because the hospital wouldn’t believe he is in pain. Frustrating because the surgery at the hospital caused the pain. Frustrated that those who were supposedly there to provide comfort after surgery did not take into consideration my genomics report, let alone basic needs. Frustrating because I have insurance. Frustrated because they charged my insurance $600,000 to remove my hip. I called my father and he informed me that Mom just couldn’t take it anymore; that the repetition of hearing me in pain is affecting her mentally. Sometimes it’s hard to imagine everyone who is affected as a whole, when the situation is so dire. It’s tough for me to see it from another point of view. But now that it was addressed, I could understand. But it gave her a reason not to talk and I still needed the only thing that could give me hope: Mom’s voice.
My father called the charge nurse and explained I needed immediate action. Pain Management refused to change my medication or even see me that night. I started to panic. I picked up the phone to call 9-1-1, played out the scenario in my head, put down the phone. I wanted to die. The seventh floor window didn’t open. No sharp objects present, plus that would just make things more painful. “Please kill me!!” I’d yell to whomever would listen. “Please kill me!” I’d yell at my nurse.
I didn't know how I survived until I saw my pain management doctor. She said she didn’t come to see me yesterday because she gave me “the same dose they gave me last time”. At this point I was so irritated and exhausted, but I managed to tell her it wasn’t enough. What she had done was use the exact same dose that didn’t work the last surgery. The exact same dose that had to be moved up several times to over three times the original amount. Somehow that part in my chart wasn’t read. This surgery I received less morphine on the PCA than the last operation. This surgery I received a blood transfusion from the amount of blood I lost during a long and serious surgery. Less morphine. This is where I kicked myself for not turning in the original grievance for this hospital. I had to get something on the record.
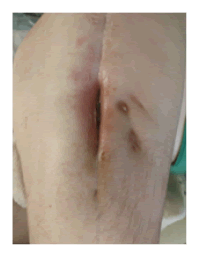
Something: I wrote a long grievance and it once again got the attention of the head pain management doctor before I turned it in. This was the same doctor that took a glance at my last grievance and solved one of the problems I had listed. But I made the mistake of celebrating a small victory over focusing on my future well-being. Since nothing was documented, nothing changed. This time I didn’t have that much to discuss with the doctor, I just wanted it documented. The mistake I’ve made from not reporting all of this can be directly related to just wanting to forget all of this. Immediately that pattern has been happening because the last thing I wanted to do was think about every detail that came with these memories, let alone write about it. My mind is now flooded with these memories. I have racing thoughts about them 24/7. It seems longer to comprehend things now since my total focus is about being in pain in the hospital. Hopefully writing about this will help me mentally. I’ve been working on this for over a year. My mouth is still grinding with an unforeseen tight underbite. Luckily, the ticks have almost stopped. I still don’t have a hip with an active infection and I have the same surgeon and hospital (Figure 2 and 3). When my infection heals I get a hip put back in. But thoughts of going back to that hospital scares the hell out of me!
Not including the washout surgery, I was at the hospital for another six-week IV antibiotic treatment. Patient relations had called me to clarify the grievance I finally turned in. I had explained in the grievance that it was the second grievance I had written, but only the first one I had turned in. Having explained that to her, I had referred to the first grievance as far as avoiding all of this again if I had turned in. I think this just confused them. I eventually turned in the first grievance, but I didn’t have the highest hopes. Like previous doctors I had asked, patient relations had said that there is nothing they can do about pain medication, and then referred me to Pain Management. It was here where I found out the only people that reviewed my grievance was pain management. That was not what I had hoped for. Since I had a medical team working on me, at least the whole team should have seen that. Back to square one.
These complaints and grievances weren’t met with any solution. Since it had now been documented, they would have to take a hard look at what had happened. The most I could get out of the floor nurse was saying that they had used a lot of pain medication in the recovery room. That was exactly what I have been making a big deal about as so all of this could have been avoided! It was obvious they were just trying to cover-up anything that may have made them look bad, instead of just addressing the issue. When did the hippocratic oath turn into the oath of admission to the Florida bar?
It’s the demeaning conundrum that gets dug-into with the mere mention of some sort of discussion; even if said medication strength is less than prescribed prior to the hospital! The other doctors that saw me in pain have somehow compartmentalized their specialty to overlook this. Have things gotten so petty and immoral, that they would rather risk me suffering in severe surgical pain than feel an ounce of chemically induced “happiness”?! Opioids’ bad! Is this punishment?!
In a response to a comment about an article regarding harmful anti-opioid propaganda, Dr. Bloom states: “That’s why I will smuggle in my own pain meds into the hospital the next time I need surgery. I absolutely distrust hospitals to provide adequate pain relief. And, of course, if I am undertreated I will throw a massive shit fit in the presence of a witness with a video camera and hopefully a reporter and a lawyer. That will get their attention.” This is the Director of Chemical and Pharmaceutical Science for ACSH.
Something is seriously wrong
In an article with the new England journal of medicine, surgeon general Dr. Vivek H. Murthy wrote in ending the opioid epidemic-a call to action regarding addicts: “Finally, we have to do all these things without allowing the pain-control pendulum to swing to the other extreme, where patients for whom opioids are necessary and appropriate cannot obtain them” [25].
I’m a white male. God only knows how many marginalized people are being taken advantage of and forgotten. My hopes are this will give others in similar situations a fighting chance of avoiding some serious trauma. Since their voice is silent, maybe this spotlight will attract some empathy for action. Or at least, bend the arc. Because I may be the first and only canary in this coal mine.
I adhere to Buddhist philosophy. Other than taking a vow not to cause suffering to any sentient being, Buddhists also believe in interdependence. Interdependence means all things are dependent upon each other: If you suffer, I suffer. Your grief is my grief. My peace is your peace. Just like microscopic cells that rely on other cells to keep us alive, nothing is separate on its own or self-reliant. Having witnessed this first hand, I have confidence this will reach the right people through compassion and we can all experience less suffering; which is the Buddha’s main goal. And since Buddha is not much different than ourselves, it should be our main goal. Even if we bend the arc in favor of compassion, we still need the correct education for the rest of the medical community; with reliable checks and balances.
Conclusion
My experience in living this, then writing about it, is to stimulate a discussion of the prescribing inadequacies of patients with the mu-opioid receptor, OPRM1, with the A118G SNP, receiving appropriate amounts of opioids directly after surgery, specifically in Florida hospitals. I don’t want others to experience the horrors of what I've been through; which have negatively impacted my day to day quality of life.
References
- Anderson H, Crooks K, Kao D, et al. The landscape of pharmacogenetic testing in a US managed care population. Genet Med. 2020;22(7):1247-1253.
[Crossref], [Google Scholar], [Indexed]
- Peciña M, Love T, Stohler CS, et al. Effects of the Mu opioid receptor polymorphism (OPRM1 A118G) on pain regulation, placebo effects and associated personality trait measures. Neuropsychopharmacol. 2015;40(4):957-965.
[Crossref], [Google Scholar], [Indexed]
- Ren ZY, Xu XQ, BaoYP, et al. The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: A systematic review and meta-analysis. Pain Physician. 2015;18(2):131-152.
[Crossref], [Google Scholar], [Indexed]
- Kang J, Zhao Z, Lv J, et al. The efficacy of perioperative gabapentin for the treatment of postoperative pain following total knee and hip arthroplasty: A meta-analysis. J Orthop Surg Res. 2020;15(1):332.
[Crossref], [Google Scholar], [Indexed]
- Prater CD, Zylstra RG, Miller KE. Successful pain management for the recovering addicted patient. Prim Care Companion J Clin Psychiatry. 2002;4(4):125-131.
[Crossref], [Google Scholar], [Indexed]
- Bloom J. Florida officials successfully withheld pain meds from surgical patients. aren't they special?. Amer Council Sci Health. 2019.
- Ahern, Avila, Fant, et al. The Florida Senate. HR 21. 2018.
[Crossref], [Google Scholar], [Indexed]
- Aubrun F, Gaulain KN, Fletcher D, et al. Revision of expert panel's guidelines on postoperative pain management. Anaesth Crit Care Pain Med. 2019;38(4):405-411.
[Crossref], [Google Scholar], [Indexed]
- Lohman D, Schleifer R, Amon JJ. Access to pain treatment as a human right. BMC Medicine. 2010;8(1):8.
[Crossref], [Google Scholar], [Indexed]
- Roosevelt E, Chang E, Malik C, et al. Universal declaration of human rights. United Nation.1948.
[Crossref], [Google Scholar], [Indexed]
- https://www.ncbi.nlm.nih.gov/books/NBK64089/
- Wasan AD, Correll DJ, Kissin, et al. Latrogenic addiction in patients treated for acute or subacute pain: a systematic review. J Opioid Manag 2006;2:16-22.
[Crossref], [Google Scholar], [Indexed]
- Luo J, Min S. Postoperative pain management in the postanesthesia care unit: an update. J Pain Res. 2017;10:2687-2698.
[Crossref], [Google Scholar], [Indexed]
- Ray LA, Bujarski S, Squeglia LM, et al. Interactive effects of OPRM1 and DAT1 genetic variation on subjective responses to alcohol. Alcohol Alcohol. 2014;49(3):261-270.
[Crossref], [Google Scholar], [Indexed]
- Ramchandani VA, Umhau J, Pavon F, et al. A genetic determinant of the striatal dopamine response to alcohol in men. Mol Psychiatry. 2011;16:809–817.
[Crossref], [Google Scholar], [Indexed]
- http://www.leg.state.fl.us/statutes/index.cfm?App_mode=Display_Statute&URL=0800-0899/0893/0893ContentsIndex.html.
- https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf
- https://emergency.cdc.gov/newsletters/loader.html?site=https://emergency.cdc.gov/newsletters/coca/050219.html.
- To K, Cao R, Yegiazaryan A, et al. General overview of non tuberculous mycobacteria opportunistic pathogens: mycobacterium avium and mycobacterium abscessus. J Clin Med. 2020;9(8):2541.
[Crossref], [Google Scholar], [Indexed]
- Licon AG. Florida's top doctor refuses mask, is told to leave meeting. 2021.
[Crossref], [Google Scholar], [Indexed]
- https://edition.cnn.com/2001/LAW/06/13/elderabuse.lawsuit/index.html.
- Joseph A. Her husband died by suicide. She sued his pain doctors-a rare challenge over an opioid dose reduction. Health. 2021.
[Crossref], [Google Scholar], [Indexed]
- Vetter S. Understanding Human behavior in times of war. Mil Med. 2007;172(2):7-10.
[Crossref], [Google Scholar], [Indexed]
- Bloom J. 4 Out of 5 want to avoid opioids after surgery? A painful lie. ACSH. 2021.
[Crossref], [Google Scholar], [Indexed]
- Murthy VH. Ending the opioid epidemic-A call to action. N Engl J Med. 2016;375:2413-2415.
[Crossref], [Google Scholar], [Indexed]