Research Article - Journal of Public Health Policy and Planning (2025) Volume 8, Issue 4
Factors affecting community-based health insurance enrolment among households in Degadamot District, Ethiopia: Community-based cross sectional study.
Melesse Belayneh1*, Mastewal Tamiru2
1Department of Health System and Health Economics, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
2Department of Inpatient Service, Tibebe Ghion Specialized Hospital, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
*Corresponding Author:
- Melesse Belayneh
- Department of Health System and Health Economics,
- College of Medicine and Health Science,
- Bahir Dar University,
- Bahir Dar, Ethiopia
- E-mail: meleseyayeh@gmail.com
Received: 05-Jan-2024, Manuscript No. AAPHPP-24-124473; Editor assigned: 09-Jan-2024, AAPHPP-24-124473 (PQ); Reviewed: 23-Jan-2024, QC No. AAPHPP-24-124473; Revised: 20-Jan-2025, Manuscript No. AAPHPP-24-124473 (R); Published: 27-Jan-2025, DOI: 10.35841/aaphpp-9.1.271
Citation: Belayneh M, Tamiru M. Factors affecting community-based health insurance enrolment among households in Degadamot District, Ethiopia: Community-based cross sectional study. J Public Health Policy Plan. 2025;9(1):271
Abstract
Background: Community-based health insurance is provided in several countries as part of the overall health funding approach, Including Ethiopia. Ethiopia has been utilizing the basic healthcare model and has endured a number of fundamental issues, such as insufficient service coverage, unequal access, and high out-of-pocket expenses. However, there are few studies showed that low CBHI enrolment. However, enrolment is a progressive activity, and there is updated evidence about factors of enrolment.
Objective: This study was focused on the factors affecting community-based health insurance enrolment among households in Degadamot district, Ethiopia in 2022. Methods: A community-based cross-sectional study was employed among 736 households from August 15 to October 15,2022. Participants were screened by using a two-stage sampling technique. Data were collected using interviewer-administered pre-tested questionnaire and entered into EPI-Info 7 and transported to SPSS version 26. Multi-variable logistic regression was performed to further analysis. A p-value less than 0.05 with a 95% confidence interval accounted significantly factors for dependent variables.
Result: The multivariate logistic regression analysis was showed that participants who were aged in years of 35-54 years (AOR=2.89; 95% CI: 1.78, 4.69), 55-74 years (AOR=3.84; 95% CI: 2.18, 6.75), >=75 years (AOR=2.25; 95% CI: 1.04, 4.89), family size of households who had 5 and above members (AOR=2.06; 95% CI: 1.43-2.95), primary education (AOR=2.10; 1.43, 2.95), secondary and above education(AOR=2.50; 95% CI: 1.88, 4.99), had own land (AOR: 1.62; 95% CI: 1.26, 3.54), had own domestic animals (AOR=2.11; 95% CI: 1.26, 3.54), enrolled in Safety net program (AOR=2.80; 95% CI: 1.52-5.15) and had good knowledge about CBHI (AOR=3.16; 95% CI: 2.08, 4.45) factors were significantly associated with CBHI enrollment.
Conclusion: community-based health insurance enrolment was affected by factors with age, family size, residence, educational status, owning land and domestic animals, and being enrolled in the safety net program and had good knowledge about CBHI were associated with CBHI enrolment. Hence, a strong monitoring and evaluation system, strategies to design to increase awareness levels about the CBHI scheme's benefits, special considerations for young age people, community based education and collaboration with social security sectors.
Keywords
Community-based, Health insurance, Associated factors, Degadamot, Ethiopia.
Abbreviations
AOR: Adjusted Odds Ratio; CBHI: Community-Based Health Insurance; COR: Crude Odds Ratio; SPSS: Statistical Package for the Social Sciences
Introduction
The Community-Based Health Insurance (CBHI) program is renowned as a successful method for achieving universal access to health services and enough financial protection from medical costs. Few low-income countries have been able to put in place the required payment structures for it, despite the World Health Organization suggesting it as one of its ideas for achieve universal health care. According to the data, many low-income countries had a difficult time keeping up their healthcare budgets during the past three decades and spent, on average, less than $23 per person [1, 2].
In addition, numerous studies have recently made recommendations on how community health insurance may improve access to care and give financial protection in addition to covering the expenses of illness for these disadvantaged individuals [3]. Ethiopia has been utilizing the primary healthcare model since 1978, yet the country has faced a number of fundamental issues, such as insufficient service coverage, unequal access, and high out-of-pocket expenses.
CBHI schemes have been implemented in Ethiopia to reduce the financial shock caused by unforeseen and irregular out-of pocket expenses and to encourage resource pooling for healthcare, which would improve access to and usage of health services. In order to provide health care for its citizens, Ethiopia's government heavily relies on outside donations (50%) and personal contributions (34%). Ethiopia, one of the developing countries, has developed a health policy and health insurance strategy to meet the needs of people through a payment system based on ability, with specific assistance mechanisms for those who cannot afford to pay for their healthcare need.
Beginning in thirteen districts chosen from four regional states (Oromia, SNNPR, Amhara, and Tigray) in the middle of 2011, the CBHI pilot was implemented. According to a survey, after CBHI was implemented in these areas, healthcare spending per person increased by a factor of two. Nevertheless, there is little information available regarding the extent of its use. For program administrators and decision-makers, data on Community-Based Health Insurance (CBHI) enrolment and its contributing factors at the district and national levels is crucial. Nonetheless, it is uncommon [4,5].
Researchers reported that there are a number of factors that influence on the enrolment of community based health insurance in Ethiopia. Some of these factors are: Age, sex, educational status, family size, income, good awareness about CBHI scheme, perception towards community based health insurance affordability of premium payment wealth index, perceived health status, perceived quality of care, timing of collecting premium, chronic disease, community solidarity, treatment choice, trust on program, poor healthcare worker attitudes and long waiting times [6-11].
Despite their increased of performance and unique vulnerability, there is no evidence in the study area. Therefore, this study focused on factors affecting community-based health insurance enrolment among households in Degadamot district, Ethiopia, in 2022.
Materials and Methods
Study design, period and setting
A community-based cross-sectional study was conducted among households from August 1 to August 30, 2022, in the Degadamot district. Degadamot district is located 239 kilometers from Bahir Dar, the capital city of the Amhara region, and 465 kilometres from Addis Ababa, the capital city of Ethiopia. According to data from the district health office, the district has a population of 152,345 people and 33,336 households. There are 29 rural kebeles, six health centres, 29 health posts, seven private primary clinics, and one primary public hospital in the district.
Sample size determination
The sample size was calculated using a single proportion formula by considering the following: 66.3% proportion of community based community-based insurance, 95% Confidence Interval (CI), 5% margin of error and 95% CI, Zα/2=critical value=1.96, applied as:
n=(Zα /2)2 × P (1-P)/d2
=((1.96)2 × 0.66 (1-0.66))/(0.05)2=446
Design effect (1.5) was used a two-stage sampling technique, and a 10% non-response rate was considered. The final sample size for the study was 736 households.
Sampling techniques
A two-stage random sampling was employed to select eligible participants. First, using simple random selection, representative kebeles were chosen from a total of 29 kebeles that were available. Next, the number of households in the sampling frame of the chosen kebeles was divided proportionately to the total number of homes included in the study. The Community Health Information System (CHIS) is used by all health posts, therefore the family folders that are available in each kebele were where the sampling frame with a list of every household was gathered. Finally, respondents (household heads) were chosen from framed lists of households using systematic random sampling, which was a number between one and the sampling interval (12th). The first respondent was the seventh from the register which was selected by lottery method. Every 12th interval taken to study participants. Households aged 18 and above who had lived in the kebele for at least six months were included. Participants who had less than one year CBHI enrolment and seriously ill were excluded.
Data collection tools and procedures
A standardized and structured questionnaire was developed based on previously available information and published studies. The questionnaire was first prepared in English and then translated into the local language (Amharic) to easily understand it for data collection and translated back to English for data analysis. The questionnaires contain socio- demographic and socio-economic characteristics, CBHI enrolment, sources of information and knowledge of community-based health insurance enrolment. Face-to-face interviews were conducted by seven trained BSc public health professionals. Households were not present during data collection date, two times visit was conducted to their home. They were closely monitored under the supervision of one supervisors and a principal investigator. The questionnaire was pretested among 5% of the sample (n=37) household heads in non-selected kebeles. Minor modifications, like ambiguity words and incorrect statements were edited. The principal investigator and supervisor were responsible for monitoring the data collection process.
Operational definition
Community based health insurance enrolment: Households that were CBHI members as evidenced by their renewed membership cards and new CBHI members were classified as ‘’Yes,’’ whereas those that were not members and households that have dropped out were classified as ‘’No’’ [12].
Good knowledge: Study subjects who scored the mean and above CBHI knowledge related questions [13].
Poor knowledge: Study participants who scored below the mean on CBHI knowledge questions.
Household wealth index: Households were given scores based on the number and kinds of consumer goods they own. Each typical household member was given a score, which was then used to rank each member of the household population according to that score to create wealth quantiles.
Data analysis
Data were transferred into Epi Info 7 version 2.5 and then exported to SPSS version 26 for cleaning and analysis. Finally, descriptive and summary statistics were presented using texts and tables. The bivariate analysis was carried out to determine the association between CBHI enrolment and associated factors, and the variables were chosen for multivariate analysis by p-value 0.25. To mitigate any potential confounding effects, a multivariable logistic regression analysis was used. Hosmer and Lemeshow's test for the model's goodness of fit revealed appropriate(X2=8.46, p-value=0.19). The Adjusted Odds Ratios (AOR) with a 95% confidence interval and p-value 0.05 were used to identify the variables that had significant association.
Ethical approval and consent to participate
Ethical clearance and supportive letters were obtained from College of Medicine and Health Sciences Bahir Dar university Institutional Review Board (IRB). Before proceeding with actual data collection, a formal letter was written to the Degadamot district health office. To maintain confidentiality, individual identifier were excluded. Written informed consent was obtained from participants. Consent was documented on a paper consent. In addition, respondents were informed of the purpose, possible advantages and disadvantages, the right to continue or stop to the interview.
Results
Socio-demographic characteristics of study participant
A total of 736 participants completed the interview, giving it a response rate of 100%. Of these, 80.2% (593) were male respondents. 43.3% (319) of the respondents were in the age range of 35 to 54 years, while the mean age (SD) of the study participants was 44.9 (± 16.5) years. Around 71.7% (528) of the respondents had no formal education. In terms of household members, more than half of the 53.9% (397) had 5 or more members. According to the wealth index, one-third (32.7%) were middle-class. Regarding respondents' awareness of CBHI, 53.9% (397) of them heard about CBHI, and they were classified as an aware group. Respondents who had ever heard about the CBHI scheme were nearly three-fifth (59.6%) heard from CBHI officials and political cadres (Table 1).
| Variable | Category | Frequency | Percent |
| Sex | Male | 593 | 80.6 |
| Female | 143 | 19.4 | |
| Age | 20-29 years | 93 | 12.6 |
| 30-39 years | 277 | 37.6 | |
| 40-49 years | 148 | 20.1 | |
| 50-60 years | 139 | 18.9 | |
| 60-70 years | 79 | 10.7 | |
| Educational status | No formal education | 528 | 71.7 |
| Primary education | 166 | 22.6 | |
| Secondary and above | 42 | 5.7 | |
| Family size | Less than 5 members | 339 | 46.1 |
| 5 and above members | 397 | 53.9 | |
| Under five children in household | Less than 3 children | 402 | 54.6 |
| 3 and above children | 334 | 45.4 | |
| Wealth index | Poorest | 103 | 14 |
| Poorer | 193 | 26.2 | |
| Middle | 241 | 32.7 | |
| Richer | 161 | 21.9 | |
| Richest | 38 | 5.2 | |
| Knowledge about CBHI | Good | 397 | 53.9 |
| Poor | 339 | 46.1 | |
| Sources of information first time about CBHI | Neighbours or friends | 132 | 17.9 |
| CBHI officials and political cadres | 439 | 59.6 | |
| Mass media (Radio, Tv, Social media) | 168 | 22.5 |
Table 1. Socio-demographic characteristics of study participant in Degadamot District, Ethiopia (n=736).
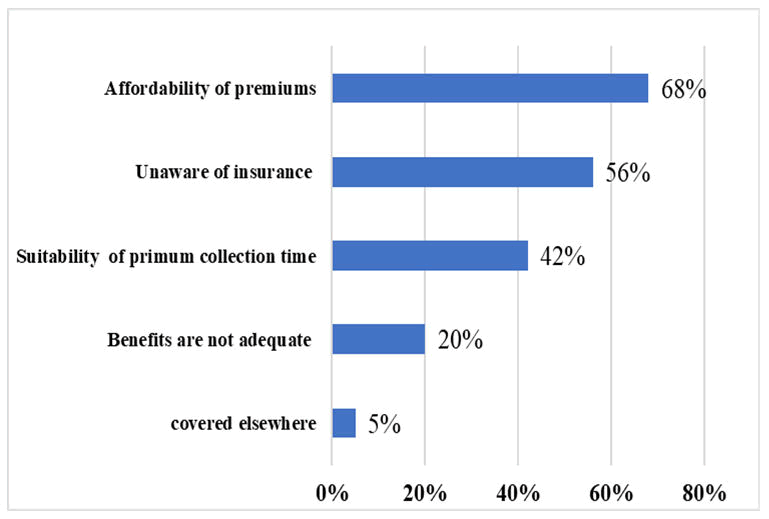
Reasons for not enrolling in community-based health insurance
The finding showed that more than two third (68%) household heads were responded that the premium is not affordable, still more than half (56%) of the participants have not clear about insurance affordability and two in five participants said that time of premium collection is not suitable for enrolling to CBHI (Figure 1).
Figure 1. Reasons for not enrolling in community based health insurance in Degadamot daistrict 2023.
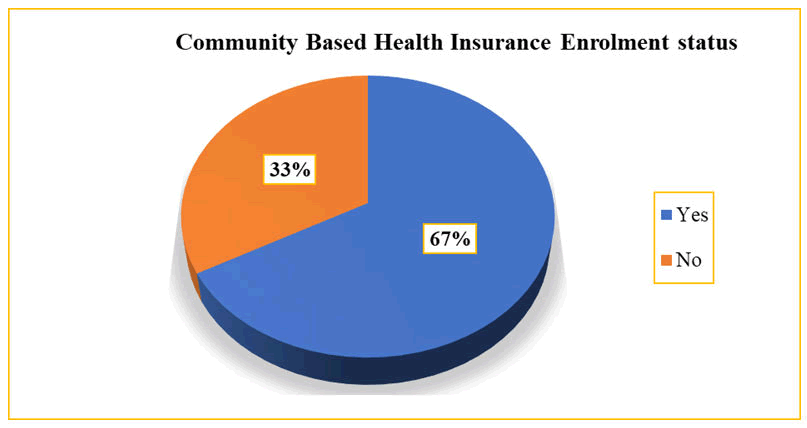
Magnitude of community based health insurance enrolment
Among the total of 736 respondents, 33% (245) (29.2% 38.1%) of them reported that they were not enrolling to CBHI scheme (Figure 2).
Figure 2. Community based health insurance enrolment status in Degadamot district 2022 (n=736).
Factors affecting community based health insurance enrolment
Both bi-variable and multi variable logistic regression analyses were employed. In the bi-variable analysis variables such as age, sex, family size of household, educational status, marital status, own domestic animals, wealth status, enrolled in Safety net program, knowledge about CBHI were significantly associated with community-based health insurance enrolment. Variables with a p-value of <0.25 in the bi-variable logistic regression analysis were entered into multi variable logistic regression analysis.
The multivariate logistic regression analysis revealed that participants who were aged in years of 35-54 years (AOR: 2.89; 95% CI: 1.78, 4.69), 55-74 years (AOR: 3.84; 95% CI: 2.18, 6.75), >=75 years (AOR: 2.25; 95% CI: 1.04, 4.89), family size of households who had 5 and above members (AOR:2.06; 95% CI: 1.43-2.95), primary education (AOR: 2.10; 1.43, 2.95), secondary and above education (AOR: 2.50; 95% CI: 1.88, 4.99), had own domestic animals (AOR: 2.11; 95% CI: 1.26, 3.54), enrolled in Safety net program (AOR: 2.80; 95% CI: 1.52-5.15) and who had good knowledge about CBHI (AOR: 3.16; 95% CI: 2.08,4.45) were more likely significant factors of CBHI enrolment (Table 2).
| Variable | Categories | Enrolment of CBHI | COR (95% CI) | AOR (95% CI) | |
| Yes | No | ||||
| Age in years | 20-29 years | 42 | 51 | 0.81 (0.44-0.92) | 0.63 (0.32-0.89)* |
| 30-39 years | 204 | 73 | 2.73 (1.63-4.56) | 1.78 (1.13-3.21)** | |
| 40-49 years | 104 | 44 | 2.31 (1.31-4.05) | 1.64 (1.11-3.18)** | |
| 50-60 years | 101 | 38 | 2.59 (1.45-4.62) | 181 (1.04-3.52)* | |
| 60-70 years | 40 | 39 | 1 | 1 | |
| Sex | Male | 404 | 189 | 1.38 (0.94-2.01) | |
| Female | 87 | 56 | 1 | ||
| Family size of household | Less than 5 members | 194 | 145 | 1 | 1 |
| 5 and above members | 297 | 100 | 2.22 (1.62-3.03) | 2.06 (1.43-2.95)*** | |
| Educational status | No formal education | 16 | 26 | 1 | 1 |
| Primary education | 113 | 53 | 3.46 (1.85-6.78) | 2.10 (1.43-295)** | |
| Secondary and above education | 362 | 166 | 3.54 (1.72-6.70) | 2.50 (1.88-4.99)* | |
| No | 69 | 80 | |||
| Own domestic animals | Yes | 450 | 59 | 3.48 (2.26-5.37) | 2.11 (1.26-3.54)*** |
| No | 41 | 186 | 1 | ||
| Wealth status | Poorest | 55 | 48 | 0.83 (0.39-1.77) | |
| Poorer | 22 | 16 | 1.03 (0.52-2.08) | ||
| Middle | 113 | 80 | 2.40 (1.18-4.89) | ||
| Richer | 116 | 45 | 1.88 (0.90-3.89) | ||
| Richest | 185 | 56 | 1 | ||
| Enrolled in safety net program | Yes | 73 | 17 | 2.34 (1.35-4.7) | 2.80 (1.52-5.15)*** |
| No | 418 | 228 | 1 | 1 | |
| Knowledge about CBHI | Good | 286 | 111 | 3.94 (2.23-5.02) | 3.16 (2.08-4.45)*** |
| Poor | 134 | 205 | 1 | 1 | |
| Note: *p<0.05, **p<0.01, ***p<0.001, n=number, COR: Crude Odds Ratio; AOR: Adjusted Odds Ratio; p = 0.05 was taken as the level of significance and 1=reference | |||||
Table 2. Factors affecting community based health insurance enrolment in Degadamot district, Ethiopia (n=736).
Discussion
The purpose of the study identified factors associated with CBHI enrolment in Degademot district west Gojjam zone. In parallel to this, the magnitude of CBHI in the study area was also assessed. This study showed that the magnitude of CBHI enrolment among participants was 66.7% (63.2%–70.1%) in Degadamot District, West Gojjam Zone, Ethiopia. This finding was comparable with studies done in Akaki district, Oromia (66.3%), and Debub Benchi district (67%). This study was lower than national plan (80%) of Ethiopia. On the other hand, the proportion of CBHI enrolment in this study was higher when compared with other similar studies done in Bassona Worena District in the North Shewa Zone, Gida Ayanan District, Oromia Region, West Ethiopia, and Uganda. This might reflect different methodologies, access to information, sample size, and study population. Furthermore, there is a lack of managerial commitment at the lowest levels [14,15].
In this study, household heads aged 20-29 years were 37% less likely to use CBHI than those aged 60-70 years, while those aged 30-39 years (1.78 times), 40-50 years (1.64 times), and 50-60 years (1.04 times) were more likely to enrol CBHI than those aged 60-70 years. This finding was consistent with Jimma zone, 60-year-old and older households were more likely to use CBHI than younger households, and Ethiopian MEDHS, 2019 [16-18]. However, this finding was not consistent with studies in the Gidda Ayana district. This disparity could be attributed to a time difference in studies and socio-demographic factors, as well as a misunderstanding of the CBHI benefit package.
In this study, households with five or more members (2.06) were more likely to enrol CBHI than households with fewer than five members. This study was in agreement with studies conducted in Fogera district, Southern Ethiopia, Bugna district, and Sabata district of Ethiopia [19,20]. The inconsistent study in Akaki district, Oromia, found that families with less than five members had a 3 times higher CBHI enrolment rate when compared to those with more than five members. This difference might be due to time study differences, understanding the benefits of the CBHI, or socio demographic factors.
This study demonstrated that participants who had primary education (2.10 times) and secondary or higher education (2.5 times) were four times more likely to be CBHI members than those who did not have formal education. This study was in agreement with a study conducted in Ethiopia, Kenya, and Sri Lanka. The possible explanation is education improves the understanding of health services.
In this study, those enrolled in the safety net program had 2.80 times more likely CBHI enrolment when compared to those who had not enrolled. The finding is consistent with a study in Ethiopia and Nigeria. It demonstrates that taking part in the safety net program increases the likelihood of taking CBHI. The rationale may be that low-income households prefer to sign up for CBHI because they cannot afford high out-of pocket costs or because their CBHI premium is waived as a result of their low income.
This study found that respondents who had good knowledge of CBHI were 3.16 times more likely to enrol community-based health insurance than those who had not. This study was in agreement with the findings of another studies. This could be due to being knowing of the benefits of enrolling in CBHI and its impact on health-seeking behaviour. This study is also inconsistent with studies done in Ethiopia and Nigeria. The difference might be in the efforts of concerned bodies to create awareness, the timing of the scheme's launch in the study area, and the study period.
Limitation of the study
The study was used cross sectional study design, which could not show the cause and effect relationships among CBHI enrolment and associated factors. In addition, study might be prone to social desirability and information bias.
Conclusion
Factors affecting community based health insurance enrolment, such as, age, family size, residence, educational status, domestic animals, being enrolled in the safety net program, and had knowledge about CBHI were associated with CBHI enrolment. As a result, this study recommends that the district health office serve as a strong monitoring and evaluation system for local-level information dissemination about the CBHI scheme's benefits, strategies to deliver c health education to increase their knowledge, about CBHI special considerations for young age people, community based education and collaboration with social security sectors. This study will serve as a baseline for future studies on this topic to investigate the low CBHI enrolment. These findings suggest that policy makers, providers, and CBHI schemes need to prepare strategies to improve CBHI knowledge.
Consent for Publication
Not applicable.
Availability of Data and Materials
The datasets generated during the current study are available from the author on reasonable request.
Competing Interests
The author declares no competing interests.
Funding
Not applicable.
Author Contribution
MB came up with the concept for the study and wrote the framework. MB contributed to the study design and statistical analysis, critically revised the research, edited the manuscript, and delivered the final edition. The final manuscript was read and approved by the author.
Acknowledgements
The authors thank Bahir Dar University for approving their application and for offering their critical input on this work. Thank you to everyone who participated in the study voluntarily, including the data collectors and participants.
References
- Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Trop Med Int Health. 2005;10(8):799-811.
[Crossref] [Google Scholar] [PubMed]
- Mukangendo M, Nzayirambaho M, Hitimana R, et al. Factors contributing to low adherence to community-based health insurance in rural Nyanza District, Southern Rwanda. J Environ Public Health. 2018;2018(1).
[Crossref] [Google Scholar] [PubMed]
- de Allegri M, Sauerborn R, Kouyate B, et al. Community health insurance in sub-Saharan Africa: what operational difficulties hamper its successful development?. Trop Med Int Health. 2009;14(5):586-96.
[Crossref] [Google Scholar] [PubMed]
- Mebratie AD, Sparrow R, Yilma Z, et al. Enrollment in Ethiopia’s community-based health insurance scheme. World Dev. 2015;74:58-76.
- Geferso AT, Sharo SB. Community-Based Health Insurance Utilization and Its Associated Factors among Rural Households in Akaki District, Oromia, Ethiopia, 2021. Adv Public Health. 2022;2022(1).
- Fite MB, Roba KT, Merga BT, et al. Factors associated with enrollment for community-based health insurance scheme in Western Ethiopia: Case-control study. PloS One. 2021;16(6).
[Crossref] [Google Scholar] [PubMed]
- Mirach TH, Demissie GD, Biks GA. Determinants of community-based health insurance implementation in west Gojjam zone, Northwest Ethiopia: a community based cross sectional study design. BMC Health Serv Res. 2019;19:1-8.
[Crossref] [Google Scholar] [PubMed]
- Chanie MG, Ewunetie GE. Determinants of enrollment in community based health insurance among Households in Tach-Armachiho Woreda, North Gondar, Ethiopia, 2019. PloS One. 2020;15(8).
[Crossref] [Google Scholar] [PubMed]
- Taddesse G, Atnafu DD, Ketemaw A, et al. Determinants of enrollment decision in the community-based health insurance, North West Ethiopia: a case-control study. Global Health. 2020;16(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Adebayo EF, Uthman OA, Wiysonge CS, et al. A systematic review of factors that affect uptake of community-based health insurance in low-income and middle-income countries. BMC Health Serv Res. 2015;15:1-3.
[Crossref] [Google Scholar] [PubMed]
- Nageso D, Tefera K, Gutema K (2020) Enrollment in community based health insurance program and the associated factors among households in Boricha district, Sidama Zone, Southern Ethiopia; a cross-sectional study. PLoS One 15(6).
[Crossref] [Google Scholar] [PubMed]
- Haile M, Ololo S, Megersa B. Willingness to join community-based health insurance among rural households of Debub Bench District, Bench Maji Zone, Southwest Ethiopia. BMC Public Health. 2014;14:1-10.
[Crossref] [Google Scholar] [PubMed]
- Getahun T, Teklesilassie L, Habtemichael M, et al. Magnitude of community-based health insurance utilization and associated factors in Bassona Worena District, North Shoa Zone, Ethiopia: a community-based cross-sectional study. BMC Health Serv Res. 2022;22(1):1405.
[Crossref] [Google Scholar] [PubMed]
- Negash B, Dessie Y, Gobena T. Community-Based Health Insurance Utilization and Associated Factors among Informal Workers in Gida Ayana District, Oromia Region, West Ethiopia. East Afr J Health Biomedical Sci. 2019;3(2):13-22.
- Nshakira Rukundo E, Mussa EC, Nshakira N, et al. Determinants of enrolment and renewing of community-based health insurance in households with under-5 children in rural south-western Uganda. Int J Health Policy Manag. 2019;8(10):593–606.
[Crossref] [Google Scholar] [PubMed]
- Garedew MG, Sinkie SO, Handalo DM, et al. Willingness to join and pay for community-based health insurance among rural households of selected districts of Jimma zone, southwest Ethiopia. Clinicoecon Outcomes Res. 2020:45-55.
[Crossref] [Google Scholar] [PubMed]
- Moyehodie YA, Mulugeta SS, Amare Yilema S. The effects of individual and community-level factors on community-based health insurance enrollment of households in Ethiopia. Plos One. 2022;17(10).
[Crossref] [Google Scholar] [PubMed]
- Atafu A, Kwon S. Adverse selection and supply-side factors in the enrollment in community-based health insurance in Northwest Ethiopia: A mixed methodology. Int J Health Plann Manage. 2018;33(4):902-14.
[Crossref] [Google Scholar] [PubMed]
- Negash B, Dessie Y, Gobena T. Community based health insurance utilization and associated factors among informal workers in Gida Ayana District, Oromia Region, West Ethiopia. East Afr J Health Biomed Sci. 2019;3(2):13-22.
- Abdilwohab MG, Abebo ZH, Godana W, et al. Factors affecting enrollment status of households for community based health insurance in a resource-limited peripheral area in Southern Ethiopia. Mixed method. PloS One. 2021;16(1).
[Crossref] [Google Scholar] [PubMed]