Research Article - Journal of Cancer Clinical Research (2022) Volume 5, Issue 3
Evaluation of surgical risk in patients with liver cancer.
Mohamed Sikkander A1* and Khadeeja Yasmeen2
1Department of Chemistry, Velammal Engineering College, Tamil Nadu, India
2Department of Biotechnology, North East Frontier Technical University, Arunachal Pradesh
- Corresponding Author:
- Mohamed Sikkander A
Department of Chemistry, Velammal Engineering College, Tamil Nadu, India
E-mail: ams240868@gmail.com
Received: 08-Jun-2022, Manuscript No. AACCR-22-66176; Editor assigned: 09-Jun-2022, PreQC No. AACCR-22-66176(PQ);Reviewed: 23-Jun-2022, QC No. AACCR-22-66176; Revised: 27-Jun-2022, Manuscript No. AACCR-22-66176(R); Published: 30-Jun-2022, DOI:10.35841/aaccr-5.3.115
Citation: Sikkander MA, Yasmeen K. Evaluation of surgical risk in patients with liver cancer. J Can Clinical Res. 2022;5(3):115
Abstract
The most effective treatments for liver cancer are surgical resection (tumor removal via surgery) or a liver transplant. If all cancer in the liver is completely removed, your prognosis will be the best. Small liver tumors may be treated with other methods, such as ablation or radiation. A partial hepatectomy is a surgical procedure in which a portion of the liver is removed. This procedure is only available to people who have a strong liver function, are physically fit for surgery, and have a single tumor that has not spread into blood vessels. Imaging, such as CT or MRI with angiography, is used to determine whether the cancer can be completely removed. However, during surgery, it is sometimes discovered that the cancer is too large or has spread too far to be removed, and the intended surgery cannot be performed. The majority of people with liver cancer in the United States have cirrhosis. In someone with severe cirrhosis, even removing a tiny piece of liver tissue around the borders of a tumour may not leave enough liver to perform critical tasks.
Keywords
Liver cancer, tumor, cirrhosis.
Introduction
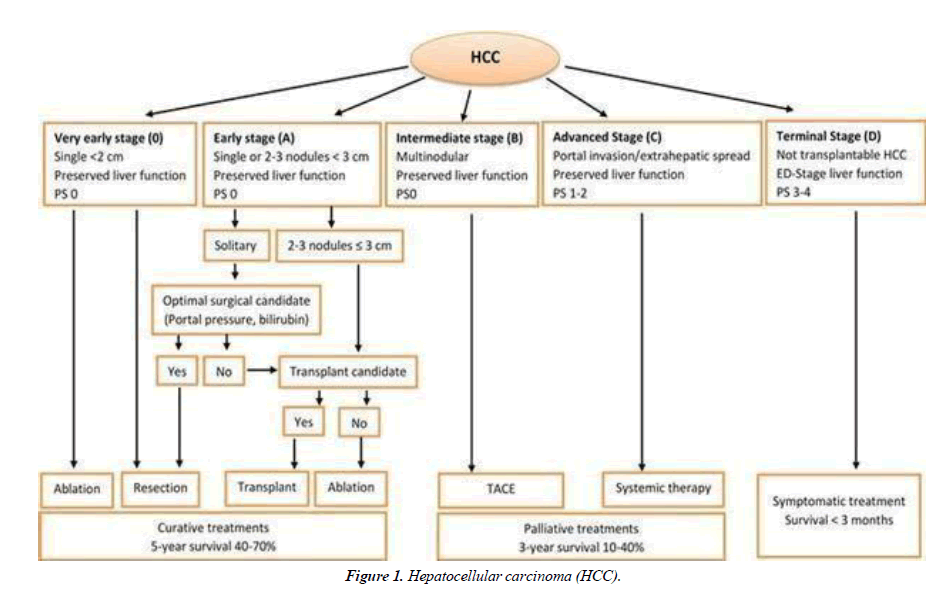
The majority of people with liver cancer in the United States have cirrhosis. In someone with severe cirrhosis, even removing a tiny piece of liver tissue around the borders of a tumor maynot leave enough liver to perform critical tasks [1]. Cirrhotic patients are usually candidates for surgery if there is only one tumor (that has not grown into blood vessels) and they retain a reasonable level of liver function (at least 30%) after the tumor is removed Figure 1.
Doctors may assess liver function by providing a Child-Pugh score (see Liver Cancer Stages), a cirrhosis measure based on certain lab tests and symptoms. Child-Pugh class A patients are the most likely to have adequate liver function for surgery. Class B patients are less likely to be surgical candidates. For people in class C, surgery is usually not an option [2].
Liver resection is a major, potentially life-threatening procedure that should only be carried out by highly skilled and experienced surgeons. Because people with liver cancer frequently have other liver disorders in addition to the cancer, surgeons must remove enough of the liver to try to remove all of the cancer while still allowing the liver to function. Bleeding is a serious problem after surgery because the liver filters so much blood. Furthermore, the liver produces chemicals that aid in blood clotting. Damage to the liver (both before and during surgery) can exacerbate bleeding problems. Complications of anesthesia, infection, blood clots, and pneumonia.
A new liver cancer can form because the residual liver still carries the underlying illness that caused the cancer [3]. A liver transplant, when available, may be the best option for some people with liver cancer. Liver transplants may be an option for patients who have tumors that cannot be removed surgically, either due to the location of the tumors or because the liver has too much disease for the patient to tolerate removing a portion of it.
A transplant is typically used to treat patients with small tumors one tumor no larger than 5 cm across or two to three tumors no larger than 3 cm that have not grown into nearby blood vessels. It is also a rare option for patients with resettable cancers cancers that can be removed completely. A transplant not only reduces the risk of a second new liver cancer, but it also allows the new liver to function normally [4].
According to the Organ Procurement and Transplantation Network, approximately 1,000 liver transplants were performed in the United States in 2016, the most recent year for which data is available. Unfortunately, the availability of liver transplants is limited. Only about 8,400 livers are available for transplant each year, with the vast majority going to patients suffering from diseases other than liver cancer. Raising public awareness about the importance of organ donation is an important public health goal that could make this treatment available to more patients suffering from liver cancer and other serious liver diseases [5].
The majority of livers used for transplants come from people who have recently died. Some patients, however, receive a portion of a liver from a living donor usually a close relative for transplantation. If a portion of the liver is removed, it can regenerate some of its lost function over time. Nonetheless, the donor faces some risks as a result of the surgery. Each year, approximately 370 living donor liver transplants are performed in the United States. Only a few of them are for people with liver cancer.
People in need of a transplant must wait for a liver to become available, which can be too long for some people with liver cancer. While waiting for a liver transplant, a person may receive other treatments such as embolization or ablation. Alternatively, doctors may recommend surgery or other treatments first, followed by a transplant if the cancer returns.
A liver transplant, like a partial hepatectomy, is a major operation with serious risks that should only be performed by skilled and experienced surgeons Figure 2.
Possible hazards include: People who receive a liver transplant are given drugs to suppress their immune systems in order to prevent their bodies from rejecting the new organ. These drugs come with their own set of risks and side effects, most notably the risk of contracting serious infections.
Because these drugs suppress the immune system, any liver cancer that has spread outside of the liver maygrow even faster than before. Some of the drugs used to prevent rejection can also cause high blood pressure, high cholesterol, and diabetes, as well as weaken the bones and kidneys and even lead to the development of a new cancer. Anesthesia complications, blood clots new liver rejection: Following a liver transplant, blood tests are performed on a regular basis to look for signs of the body rejecting the new liver. Sometimes liver biopsies are taken to see if rejection is occurring and if changes to the drugs that prevent rejection are required.
Types of surgery for liver cancer
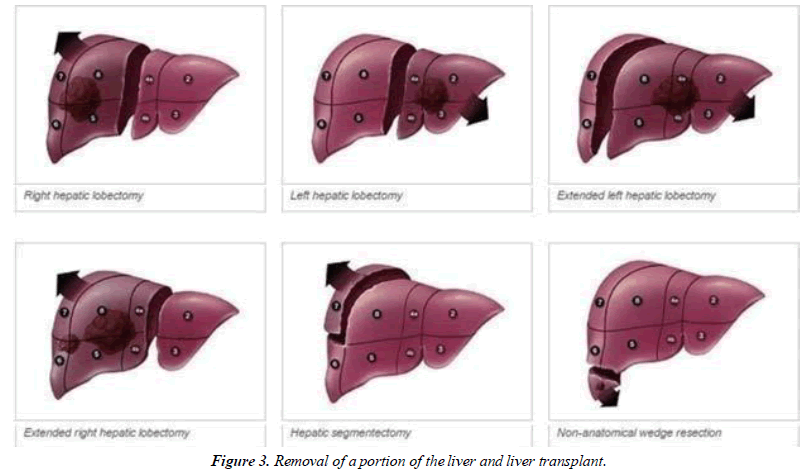
The best chance of curing primary liver cancer is through surgery. For early liver cancer, there are several surgical options [6]. These are as follows: removal of a portion of the liver (liver resection or lobotomy), and liver transplant. If, surgery may be an option for you Figure 3.The cancer has only spread to one part of your liver and has not spread to the rest of your body. You may be subjected to blood tests to determine how well your liver is functioning. The liver is a critical organ. As a result, the portion of the liver that remains after surgery must function adequately to keep you healthy. Blood test results assist your doctor in determining whether surgery is an appropriate treatment for you. If you have cirrhosis, your body may not have enough healthy liver to cope with removing a portion of it. In this case, you may need a liver transplant or other treatments.
Liver resection and lobectomy
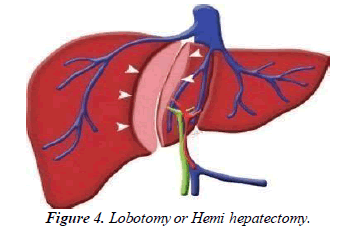
A resection is the surgical removal of cancer and surrounding tissues from your liver. Your surgeon will only consider a resection if the cancer is small, your liver is healthy, and the cancer has not spread to your blood vessels. A lobe of your liver may be removed by your surgeon [7]. This is referred to as a lobotomy or hemi hepatectomy Figure 4. If there are no underlying problems, such as cirrhosis, the liver can regenerate and function normally. People who do not have liver disease are more likely to develop fibro lamellar cancer, a type of liver cancer. This means that surgeryis frequently an option for these people.
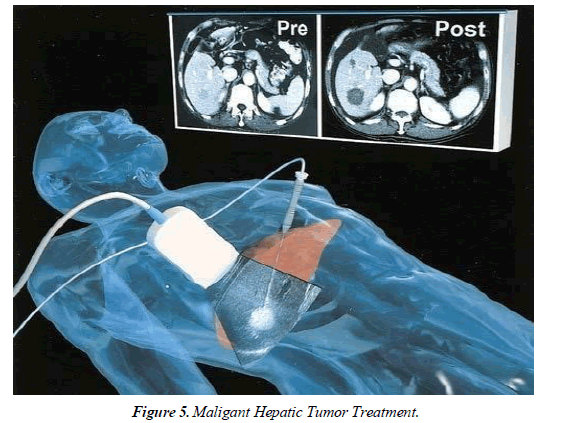
Laparoscopic procedures are less invasive than traditional open procedures and achieve the same results. The goal of a liver resection is to safely and efficiently remove a benign or cancerous liver mass. In comparison to an open procedure, a laparoscopic approach allows patients to have smaller incisions, allowing for faster recovery and a better cosmetic result. Patients are often in less pain and able to resume normal activities sooner [8]. To determine the best treatment plan for each patient, our specialists collaborate with a multidisciplinary team of physicians at Massachusetts General Hospital Figure 5.
After putting the patient to sleep with general anesthesia, three to seven small incisions are made to remove the liver mass. The procedure can take anywhere from one to seven hours, depending on the number and location of the lesions, as well as how much liver must be removed. Patients are encouraged to stay physically active and to limit their alcohol consumption in the weeks leading up to surgery. Prior to the procedure, patients will meet with their surgeon to go over the specific steps that must be taken. Most patients are given a gentle bowel preparation to help them move their colon during the procedure. The gentle bowel preparation also helps to prevent postoperative constipation.
Patients will stay in the hospital for one to six nights, depending on the extent of their liver operation. A surgeon will discuss the specifics of the postoperative recovery period with each patient based on the procedure [9]. Because the liver regenerates, the recovery time will be determined by how much of the patient's liver needs to regenerate. The majority of patients will experience significant fatigue for two to four weeks following surgery. Ibuprofen and low-dose narcotic pain medication are used to manage pain. Patients who are physically stronger usually recover more quickly after the procedure. Walking for 15-30 minutes every day, both before and after surgery, hastens recovery.
Before and after the operation, patients should limit their intake of alcohol and other liver-toxic substances. Your doctor will assist you in identifying any supplements or medications that may be taxing on your liver. In general, patients tolerate the procedure very well. Any significant procedure carries risks. Many studies, however, have shown that outcomes are better in hospitals that perform a high volume of procedures, such as Mass General.
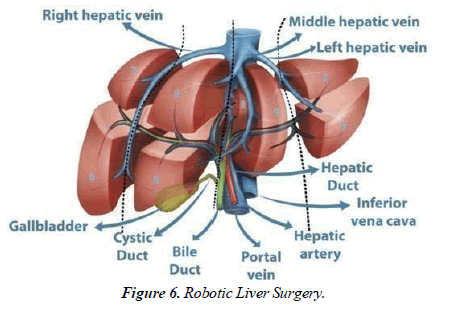
A surgeon will go over these risks in detail before performing anysurgical procedure. U.S. News & World Report consistently ranks Mass General as one of the best hospitals in the country. Our surgeons are used to seeing both local and international patients with a variety of medical conditions, and they have extensive experience performing complex hepatobiliary and laparoscopic procedures. We try to offer a laparoscopic liver procedure to all patients; however, depending on the location of the lesion and/or prior operations the patient has had, a laparoscopic approach may not be the best approach for every patient Figure 6.
Patients may experience less pain and be able to move around more frequently after a laparoscopic procedure than after an open procedure. Because of the reduced pain associated with a laparoscopic procedure, patients frequently require lower doses of pain medication. The amount of liver that needs to regenerate determines a significant portion of a patient's recovery. A laparoscopic approach has no effect on the amount of liver regeneration required. Our goal is always to keep the patient safe while performing the best surgery possible. Our objectives remain the same whether the procedure is open or laparoscopic.
Because significant medical breakthroughs for effective curative non-surgical treatment of HCCs are lacking, surgery will continue to play an important role in the multidisciplinary management of HCC patients in the future. Surgical treatment is currentlythe onlytherapeutic option that can cure the patient. Even for patients with cirrhosis as a type of "precancerosis," liver transplantation provides the opportunity - within the legal framework - to relieve the patient of both the tumour burden and the tumor-favoring disease.
If a patient can and will benefit from liver surgery for HCC, it must be carefully evaluated in a multidisciplinary context to provide the best benefit to the patient, the lowest risk of complications and procedure-related mortality, and the highest quality of life. From the perspective of a surgeon, surgery is the primary treatment option for tumor treatment, and thus the most effective therapy for providing patients with the best overall survival and recurrence-free survival.
Surgery will become even more important as new evidence emerges that the indications for liver resection for HCC can be expanded to tumor staged beyond the current recommendations. Additional treatment options are valuable and constantly improving tools for patients who are unable to undergo surgery, and they may become even more important in multimodal settings with possible preoperative use of percutaneous, intravascular, or pharmacological approaches.
Liver transplant
A liver transplant is a surgical procedure that involves removing your liver and replacing it with a healthy liver from a donor. Some people with hepatocellular liver cancer may be candidates for a liver transplant. If you have a single tumor no larger than 5 cm across, a single tumor 5 to 7 cm across that has not grown for at least 6 months, and no more than 5 small tumors any larger than 3 cm across, you may be eligible for a liver transplant. A donor liver that is a close match to yours is required for a liver transplant.
Unfortunately, you may have to wait a long time for a liver, during which time the tumor may grow. You and your family may experience anxiety while waiting for a liver transplant. In the meantime, your doctor may consider other treatments, such as ablation or chemoembolization. If you have severe liver scarring, you may not be able to receive a transplant (cirrhosis). A specialist transplant surgeon will review all of your test results and determine whether you are likely to recover well from surgery.
For example, they will examine the level of alpha fetoprotein in your blood. If this level is too high, you may not be a good candidate for a transplant. Before a transplant, you will be evaluated to determine how well your liver is functioning and whether a transplant is the best treatment for you. These tests are typically performed as an outpatient procedure, but you may require a brief hospital stay. You've had blood tests, including liver function tests. Your specialist will examine the level of alpha fetoprotein in your blood. If this level is too high, you may not be a good candidate for a transplant. Other tests, such as an ultrasound scan, will be performed on you.
A liver transplant necessitates extensive planning by various health care professionals. These people will be introduced to you during the assessment. Take advantage of this opportunity to ask as many questions as you want. This allows you to feel well prepared for the operation. If you and your doctor decide to proceed with the liver transplant, you will have several more tests before your surgery.
This could simply being admitted to the hospital a few days before your surgery. A donor liver that is a close match to your own is required for a liver transplant. Unfortunately, there are more people in need of a liver than there are available livers. It's possible you'll have to wait a long time. During this time, the cancer may progress, preventing you from receiving a transplant. You may be offered alternative treatment to reduce this risk. The goal is to keep the cancer under control while you wait. This treatment could include destroying cancer cells (ablation), injecting chemotherapy directly into the blood vessel feeding the liver cancer, and cutting off the blood supply (chemoembolization).
Conclusion
HCC management is improving due to the development of newer therapies that are combined with liver resection and liver transplantation. Even in patients with advanced liver disease, these therapies become more tolerable and precise. Better surveillance of cirrhotic patients allowed for earlier detection of HCC and higher cures rates for treatments. For patients with HCC and moderate to severe liver insufficiency, liver transplantation remains an important method of eliminating the cancer and curing the underlying liver disease with a lower risk of recurrence than resection or ablation.
Patients with small solitary tumours have the best outcomes for liver resection, but there is a high rate ofdisease recurrence due to cell dissemination prior to treatment. Improved survival for patients with advanced HCC treated with Sorafenib increases enthusiasm for additional HCC therapies. Nowadays, improved surveillance will allow early detection of HCC when loco- regional treatment is effective and transplantation is reserved for select cases. In high-risk individuals, alpha-fetoprotein and ultrasound scansshould be used every6 months for surveillance.
The mainstay of treatment for primary and secondary liver tumours is surgical resection. Morbidity and mortality rates from this surgery have decreased due to the increased use of newer surgical techniques, such as laparoscopic LR using RFA for the transection of the liver parenchyma. Patients with HCC who meet the local transplant criteria should be considered. If LT is not an option or if the patient is ineligible for transplantation, hepatic resection and/or other antitumor treatments should be considered. In metastatic NET, cytoreductive surgery may successfully control symptoms and prolong survival. Hepatic resection remains the best treatment option for CLM patients. The outcomes for resection of NCNN metastases are less promising and vary depending on the tumour of origin.
References
- Cartwright PD. Pain control after surgery: a survey of current practice. Ann R Coll Surg Engl. 1985;67(1):13.
- Merion RM, Schaubel DE, Dykstra DM, et al. The survival benefit of liver transplantation. Am J Transplant. 2005;5(2):307-13.
- Yan Y, Cai X, Geller DA. Laparoscopic liver resection: a review of current status. J Laparoendosc Adv Surg Tech. 2017;27(5):481-6.
- Bosch FX, Ribes J, Diaz M, et al. Primary liver cancer: worldwide incidence and trends. Gastroenterol. 2004;127(5):S5-16.
- Anwanwan D, Singh SK, Singh S, et al. Challenges in liver cancer and possible treatment approaches. Biochim Biophys Acta Rev Cancer. 2020;1873(1):188314.
- Balajee KL, Ramachandran N, Subitha L. Awareness and attitudes toward organ donation in rural Puducherry, India. Ann med health sci res. 2016;6(5):286-90.
- Dyer O. New MRSA strain is not at epidemic level, expert says.
- Kok B, Abraldes JG. Child–Pugh Classification: Time to Abandon?. InSeminars in liver disease. Thieme Medical Publishers. 2019 ;39(1):96-103.
- Fornari F, Civardi G, Buscarini E, et al. Cirrhosis of the liver. Digestive diseases and sciences. 1990;35(11):1403-8.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref