Research Article - Biomedical Research (2017) Volume 28, Issue 16
Ethnicity differences in the hospital costs, disease constitution and hospital characteristics for patients in Northwest China
1Department of Health-Related Social and Behavioural Science, West China School of Public Health, Sichuan University, No.17, 3 Section South Renmin Road, Wuhou District, Chengdu, PR China
2School of Humanities and Management, Heilongjiang University of Chinese Medicine, Harbin, 24 Heping Road, Xiangfang District, Harbin, PR China
- *Corresponding Author:
- Ningxiu Li
Department of Health-Related Social and Behavioural Science
West China School of Public Health
Sichuan University, Wuhou District, Chengdu, PR China
Accepted date: July 21, 2017
Abstract
This study aimed to analyze ethnicity differences in the hospitalization services utilization in the New Cooperative Medical Scheme (NCMS). The data was taken from the NCMS office of Touying town, Guyuan County, Ningxia Hui Autonomous Region. Among 2,362 patients admitted to the hospitals, 1,037 (43.9%) were of Hui ethnicity and 1,325 (56.1%) were of Han ethnicity. Approximately one-half were female in both groups. The mean age was 36 y for the Hui versus 44 y in the Han group. Non- Provincial Hospitals (NPH) admitted the largest proportion of patients in both groups, at 93 and 91%, respectively, for the Hui and Han. Overall mean cost of hospitalization was 4,624 RMB per patient, Out- Of-Pocket payment (OOP) was 2,615 RMB, 46% cost was reimbursed. In Provincial Hospitals (PH), the median hospital costs were 6,141 RMB for Hui and 9,750 RMB for Han. The median reimbursement rate in PH and NPH was 35% and 52%, respectively. In the 5-14 y age groups, Hui had a much larger proportion of injury causes than Han group. Our findings demonstrate ethnicity differences in the hospitalization services utilization in the NCMS and provide the guide for the development of preventive health care service in the minority areas.
Keywords
Hospital costs, Hospital characteristics, Disease constitution, Hui ethnic group, New cooperative medical scheme (NCMS), Reimbursement rate
Introduction
The New Cooperative Medical Scheme (NCMS) was implemented in 2003, which is a main component of China’s new rural medical insurance system. NCMS largely concentrates on catastrophic illness and reimburses mostly for inpatient expenses. By the end of 2009, 95.3% of all counties and 91.5% (815 million) of the rural population would be covered by NCMS [1]. These policies were designed to further resolve illness-led poverty and the poor health care in the local area.
Several studies had reported that patients who had participated in NCMS were more likely to look for health care service [2]. NCMS improved the utilization of hospitalization services for rural residents [3]. In China, more than 60% of populations reside in rural communities, and rural hospitals constitute 16% to 34% of all hospital discharges. Hospitalization plays a vital role in the health of rural residents.
Previous studies have shown that the variations in the cost of hospitalization and reimbursement were largely attributed to the length of hospital stay, insurance coverage/payer, racial/ ethnic and socioeconomic position, designated hospitals, hospital characteristics and physicians [4-13]. Ethnic minority regions in China have specific socioeconomic conditions and policy environments worthy of exploration to assist in the development of rural health insurance schemes [14]. However, there are few studies reporting on the effects of ethnicity on the cost of hospitalization and reimbursement. In this study we aimed to analyze ethnicity differences in the hospitalization services utilization in the New Cooperative Medical Scheme (NCMS). We enrolled the inpatients of Touying Town, Guyuan County, Ningxia Hui Autonomous Region in 2011.
Methods
Data and sampling
In this study the data was taken from the NCMS office of Touying town, Guyuan County, located in the Southern mountainous area of Ningxia Hui Autonomous Region (NHAR). During 2011, total 2,362 patients were admitted to the hospitals and their medical cost was covered by NCMS, and all of them were selected and their data were analyzed. NHAR had a GDP per capita of 11,784 RMB (about 1,571.2 US$) in 2012. 48.8% of the area’s population is Hui ethnic minority group, a Muslim minority adhering to Islamic principles, culture, diet and lifestyle. Guyuan has the greatest concentration of Hui ethnic minority in any county in China. Touying town is located in a less developed region, windy and sandy with frequent droughts, and has a mixture of both Hui and Han groups.
Variable definitions
Patient’s characteristics: We obtained the information about patient’s characteristics, including ethnicity group, gender, and age. Ethnicity group was identified as a dichotomous variable: Hui or Han. Gender was male or female. Patients were classified into five age groups, which were coded as: 1=0-4 y old age, 2=5-14 y old age, 3=15-45 y old age, 4=45-65 y old age and 5 ≥ 65 y old age.
Hospital characteristics: The patients were hospitalized in 79 medical institutions which were classified into 2 categories: Provincial Hospitals (PH) or Non-Provincial Hospitals (NPH).
Disease constitute: We used the patient’s diagnosis from primary, the causes of admission were classified according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), a medical classification list by the World Health Organization (WHO).
Hospital costs: A claims database analysis of all hospitalization costs and reimbursed of the NCMS in Touying town, was conducted to identify differences in the total inpatient hospital costs, Out-Of-Pocket payment (OOP) (hospital costs minus reimbursement costs), and the reimbursement rate (reimbursement divided by inpatient hospital costs).
Statistical analysis
All statistical analyses were performed using IBM SPSS 22.0 software. Categorical variables were reported as frequency and percentage (%) and examined using chi-squared tests. Hospital costs were reported as mean (SD), median, interquartile range, 25% and 75%, minimum and maximum, and examined using Mann-Whitney tests due to the highly skewed distribution. Regression analysis was performed to test multivariate associations among the variables. P values were two-tailed and P<0.05 was considered statistically significant.
Results
Demographics of the sample
A total of 2,362 inpatients were analyzed in this study, 1,037 (43.9%) were of Hui and 1,325 (56.1%) were of Han ethnicity. Approximately one-half were female in both groups (x2=2.021, P=0.16). The mean age was 36 y for the Hui versus 44 y for the Han ethnicity (Table 1). The proportions of patients hospitalized were similar for both groups. NPH comprised the largest proportion of patients in both groups at 93% and 91%, respectively, for the Hui and Han. PH represented a small proportion of Hui and Han at 7 % and 9%, respectively.
| Demographic characteristics | Hui (n=1,037) | Han (n=1,325) | x2 | P | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Age (y), mean(SD) | 36.56 (25.27) | 44.05 (24.65) | 49.134 | <0.001 | ||
| 0-4 | 179 | 17.41 | 158 | 11.95 | ||
| 5-14 | 84 | 8.17 | 68 | 5.14 | ||
| 15-44 | 339 | 32.98 | 365 | 27.61 | ||
| 45-64 | 245 | 23.83 | 400 | 30.26 | ||
| ≥ 65 | 181 | 17.61 | 331 | 25.04 | ||
| Gender | ||||||
| Male | 504 | 48.6 | 605 | 45.66 | 2.021 | 0.16 |
| Female | 533 | 51.4 | 720 | 54.34 | ||
| Hospital facility | ||||||
| PH | 75 | 7.23 | 114 | 8.6 | 1.486 | 0.25 |
| NPH | 962 | 92.77 | 1211 | 91.4 | ||
Table 1. Distribution of patient demographic characteristics by ethnic group.
Hospital costs, OOP and reimbursement rate
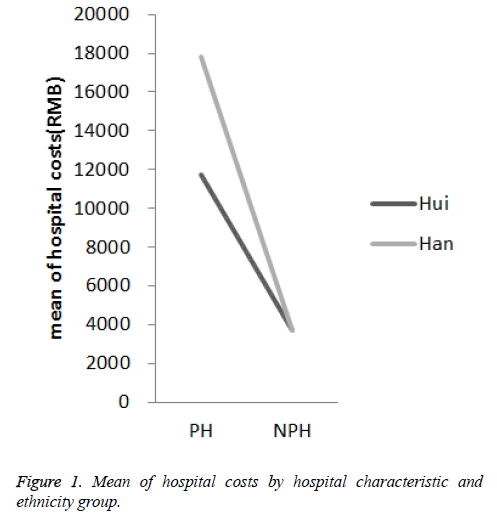
The total charges of the hospitalization during the study period were 10.9 million RMB, the average annual hospitalization charge was 4,624 RMB for inpatients, 46% of which was reimbursed by NRCM. Table 2 showed hospital costs, OOP, and reimbursement rate by hospital characteristics and ethnic group. For patients in PH, the median hospital costs was 6,141 RMB for the Hui and 9,750 RMB for the Han (Mann-Whitney test, P=0.016), the median OOP was 3,456 RMB for Hui and 4,896 RMB for the Han (Mann-Whitney test, P=0.037). However, for patients in NPH, the Hui-Han had similar median hospital costs and OOP, at 2,647-2,552 RMB (Mann-Whitney test, P=0.840) and 1,252-1,221 RMB (Mann-Whitney test, P=0.877), respectively. The median reimbursement rate of the Hui and Han was similar in both PH (35% vs. 36%) and NPH (52% vs. 52%).
| Hospital cost (RMB) | OOP (RMB) | Reimbursement rate | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PH | NPH | PH | NPH | PH | NPH | |||||||
| Hui | Han | Hui | Han | Hui | Han | Hui | Han | Hui | Han | Hui | Han | |
| Mean | 11728 | 17787 | 3677 | 3697 | 7319 | 10949 | 1992 | 2035 | 0.42 | 0.43 | 0.47 | 0.46 |
| Std. deviation | 12348 | 19488 | 3975 | 4611 | 8613 | 12791 | 2488 | 2971 | 0.16 | 0.15 | 0.17 | 0.17 |
| Median | 6141 | 9750 | 2647 | 2552 | 3456 | 4896 | 1252 | 1221 | 0.35 | 0.36 | 0.52 | 0.52 |
| Interquartile range | 15495 | 21038 | 3329 | 2926 | 10386 | 14254 | 1786 | 1563 | 0.31 | 0.27 | 0.31 | 0.31 |
| Minimum | 1099 | 869 | 189 | 126 | 741 | 618 | 89 | 48 | 0.13 | 0.05 | 0.06 | 0.04 |
| Maximum | 50760 | 79738 | 52513 | 75457 | 43760 | 54738 | 32513 | 50457 | 0.69 | 0.8 | 0.82 | 0.82 |
| Percentiles | ||||||||||||
| 25 | 3382 | 4815 | 1450 | 1544 | 1656 | 2192 | 695 | 754 | 0.32 | 0.33 | 0.31 | 0.31 |
| 75 | 18876 | 25853 | 4778 | 4471 | 12042 | 16446 | 2481 | 2316 | 0.63 | 0.61 | 0.62 | 0.62 |
Table 2. Hospital costs, OOP, and reimbursement rate by hospital characteristics and ethnic group.
Distribution of diseases by frequency and costs of hospitalization
All causes of hospitalization were shown in Table 3. In the 10 most frequent causes, diseases of the circulatory system, diseases of the respiratory system and diseases of the digestive system were the leading causes of hospitalization, followed by injury, poisoning and certain other consequences of external causes, diseases of the genitourinary system, pregnancy, childbirth and the puerperium. Certain conditions originating in the perinatal period and diseases of the eye and adnexa were the seventh and eighth most common causes of hospitalization, respectively, and the 10 together caused 2,120 hospitalizations by NCMS, which was nearly 90% of all inpatients. We observed major differences in the ranking of causes between the Hui and Han. In the Han, diseases of the circulatory system was in the first place, which were nearly twice as the Hui, the proportion were 23% and 15%, respectively. In the other ranking of hospitalization, the Hui and Han were roughly same.
| Variables | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| B | S. E | t | Sig. | B | S. E | t | Sig. | |
| Constant | 9.799 | 0.139 | 70.26 | 0 | 9.35 | 0.42 | 22.24 | 0 |
| Hospital (PH=ref.) | -1.331 | 0.061 | -21.713 | 0 | -0.91 | 0.199 | -4.56 | 0 |
| Ethnic group (Hui=ref.) | -0.056 | 0.034 | -1.647 | 0.1 | -0.227 | 0.261 | -0.87 | 0.384 |
| Gender (Male=ref.) | -0.026 | 0.034 | -0.761 | 0.447 | 0.074 | 0.108 | 0.682 | 0.495 |
| Age (0-4 y old=ref.) | 0.248 | 0.013 | 18.826 | 0 | 0.09 | 0.021 | 4.361 | 0 |
| Ethnic group × Age | 0.406 | 0.041 | 9.799 | 0 | ||||
| Ethnic group × Hospital | -0.224 | 0.119 | -1.88 | 0.061 | ||||
| Ethnic group × Gender | -0.077 | 0.066 | -1.18 | 0.24 | ||||
| R2 | 0.249 | 0.28 | ||||||
| F change | 194.158 | 33.941 | ||||||
Table 3. Multiple regression analyses of hospital, ethnic group, gender, age, and ethnic group by age, hospital and gender
There are major differences in hospital costs by ethnicity group and major cause grouping. Overall, diseases of the circulatory system, diseases of the digestive system and injury, poisoning and certain other consequences of external causes were the leading of hospital costs, followed by diseases of the respiratory system, neoplasms, diseases of the genitourinary system. The 6 together cost 8.79 million RMB, which was about 80% of the total hospital costs.
The reasons for hospitalization were different in the age group. In the 0-4 y age group, Hui-Han disease categories were similar, nearly half were diseases of the respiratory system (47.5%). Certain conditions originating in the perinatal period accounted for nearly a quarter (23.5%, 27.8%, respectively). In the 15-44 y age groups, diseases of the digestive system were nearly 19% (20.1%, 18.4, respectively). Injury, poisoning and certain other consequences of external causes were nearly 17% (18.9%, 15.6%, respectively). Pregnancy, childbirth and the puerperium were about 14%. In the 45-64 y age group, diseases of the circulatory system were 29%. Diseases of the digestive system were 22%. In the ≥ 65 y old group, Hui-Han classification of diseases were similar, but the proportion was different, diseases of the circulatory system for Hui and Han were 37%, 47%, respectively. In the 5-14 y age group, Hui had a much larger proportion of injury, poisoning and certain other external causes (27% vs.7%) but a much lower proportion of respiratory diseases (13% vs. 42%) than the Han group. Digestive diseases had similar proportion in both groups (25-26.5%).
Ethnic group as a moderator of the relationship between age, hospital characteristic, and gender with hospital costs
In model 1, the hospitals and age were significantly associated with hospital costs, and the model explained 24.9% of the observed variability (Table 3). In model 2, multiple regression analyses revealed a significant interaction between age and ethnic group (B=0.406, p<0.001) and a marginal significant interaction between hospital and ethnic group (B=-2.224, p=0.061) on hospital costs.
In order to demonstrate the moderate effect and the size of the effect of ethnic group on the association between the level of hospital and hospital costs, the average number of hospital costs for the Hui and Han in PH and NPH was calculated and plotted. As shown in Figure 1, there was a negligible difference in the hospital costs between Hui and Han in NPH (mean=3,688, 95% CI=3506-3871). In contrast, in PH average hospital costs of Han group was 1.5 times (mean=17,787, 95% CI=14171-21403) of Hui group. The effect size of the difference was in the small to medium rang (Cohen’s d= 0.37).
Discussion
The difference of disease spectrum and hospital costs in PH
By analyzing the composition of hospital diseases, we can know current health hazards of common diseases and provide the rational distribution of medicine and health resources. In our study, overall disease spectrum of Hui and Han was different. For the Han, diseases of the circulatory system ranked the first and diseases of the digestive system ranked the third. For the Hui, diseases of the digestive system ranked the first and diseases of the circulatory system ranked the third. Diseases of the respiratory system ranked the second in both Han and Hui. This is related to unique diet, living habit and genetic background of Hui and Han. In addition, the average age of Hui patients was 7.5 y lower than Han patients. The incidence of diseases of the circulatory system is known to be positively correlated to the age. These data suggest that health policy makers should employ different health service and disease prevention strategies for Hui and Han.
Hui and Han patients showed no difference in the choice of medical institutions, but the hospital costs were different. Han patients spent more money in high-grade medical institutions, and the amount spent was more dispersed. A large number of studies have shown that the cost is related to the type of disease, the severity of the disease, length of hospital stay, economic condition, and the religious culture. The reason for the difference need further study.
Graded reimbursement system
The average compensation rate was 46%, consistent with previous studies. Some studies suggest that the reimbursement system does not achieve grade ladder medical expenses. This study supported this view; high-level hospital reimbursement rate is lower while low-level hospital reimbursement rate is higher. The cost of hospitalization is a non-normal distribution of data, so the median is usually used. The proportion of reimbursement in this study was 35% and 52% at PH and NPH, respectively.
However, the real reimbursement rate of hospitalized patients was much lower than the nominal, especially in NPH with the range of 60-90%. OOP was 2,615 RMB, about more than half the average annual wage in Guyuan County. The proportion of compensation is affected by the patient’s medical institutions and the complexity of reimbursement procedures. Furthermore, high OOP NCMS hospitalized patients may be banned from receiving necessary medical care, especially for those living in poor rural areas [15].
The difference of diseases prevention and treatment for 5-14 y old children
In this study, Hui children inpatients accidental injuries are the first largest contributor to ethnicity disparities in incidence rate. Hui cases were nearly four times as many as those of Han and more than half of the hospitalizations were attributed to fractures. Home injuries and falls are responsible for the majority of the injuries. Parents play an important role in the prevention of child prevalence of unintentional injuries. Many studies have demonstrated that family with lower socioeconomic status was associated with children intentional injury risk [16]. Generally, Hui get married at a younger age. Younger parents are usually less experienced to care their children. On the other hand, due to Family Planning Policy and special fertility culture, Hui has more children than Han. As a result, Hui did not have enough time to take care of their children. Hui parents should pay special attention to 5 to 14 y kids. Teachers should assist parents to help children, thereby reducing the rate of injuries.
Children are susceptible to respiratory disease. Of particular concern are the in inpatient rates among 5-14 y old. Within this group, Han had over three times the rate of their Hui peers. The reason may be low smoking rate in Hui. Passive smoke is particularly dangerous for children. Children exposed to second-hand smoke are at higher risk of respiratory diseases. Therefore, it is particularly important to strengthen the education of tobacco control and enhance their guardian’s health protection awareness.
In conclusion, our study showed the differences in the hospitalization services utilization in Hui and Han. These findings provide the guide for the development of preventive health care service in the minority areas in Northwest China.
Conflicts of Interest
The authors declare no conflict of interest.
References
- China Ministry of Health: China Health Statistical Yearbook. Peking Union Medical College Press, Beijing 2009.
- Zou J, Yang W, Cook DM, Yuan Z, Zhang, L, Wang X. New cooperative medical financing policy and hospitalization in rural china: Multi-stage cross-sectional surveys. Int Health 2016; 8: 59-66.
- Yu B, Meng Q, Collins C, Tolhurst R, Tang S, Yan F, Bogg L, Liu X. How does the new cooperative medical scheme influence health service utilization? A study in two provinces in rural china. BMC Health Serv Res 2010; 10: 116.
- Wei JW, Heeley EL, Jan S, Huang Y, Huang Q, Wang JG, Cheng Y, Xu E, Yang Q, Anderson CS. Variations and determinants of hospital costs for acute stroke in china. PLoS One 2010; 5.
- Lorch SA. Equivalent lengths of stay of paediatric patients hospitalized in rural and non-rural hospitals. Paediatrics 2004; 114: 400-408.
- Hagiwara M, Juarez DT, Yamada S, Miyamura J, Sentell T. Inpatient hospitalization costs: A comparative study of Micronesians, native Hawaiians, Japanese, and whites in Hawai’i. Int J Environ Res Public Health 2016; 13: ijerph13010029.
- Cook CB, Naylor DB, Hentz JG, Miller WJ, Tsui C, Ziemer DC, Waller LA. Disparities in diabetes-related hospitalizations: Relationship of age, sex, and race/ethnicity with hospital discharges, lengths of stay, and direct inpatient charges. Ethn Dis 2006; 16: 126-131.
- Hines AL, Andrews RM, Moy E, Barrett ML, Coffey RM. Disparities in rates of inpatient mortality and adverse events: Race/ethnicity and language as independent contributors. Int J Environ Res Public Health 2014; 11: 13017-13034.
- Kim TH, Samson LF, Lu N. Racial/ethnic disparities in the utilization of high-technology hospitals. J Natl Med Assoc 2010; 102: 803-810.
- Petrou S, Kupek E. Socioeconomic differences in childhood hospital inpatient service utilisation and costs: Prospective cohort study. J Epidemiol Community Health 2005; 59: 591-597.
- Qiu P, Yang Y, Zhang J, Ma X. Rural-to-urban migration and its implication for new cooperative medical scheme coverage and utilization in china. BMC Public Health 2011; 11: 520.
- Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJ, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg 2012; 255: 1-5.
- Physician-attributable differences in intensive care unit costs: A single-center study. Am J Respir Crit Care Med 2006; 174: 1206-1210.
- Huang L, Yang D, Yao L, Liu Z, Wu W. Guangxi’s rural health insurance scheme: Evidence from an ethnic minority region in china. Rural Remote Health 2013; 13: 2454.
- Puffer RC, Planchard R, Mallory GW, Clarke MJ. Patient-specific factors affecting hospital costs in lumbar spine surgery. J Neurosurg Spine 2016; 24: 1-6.
- Hussey JM. The effects of race, socioeconomic status, and household structure on injury mortality in children and young adults. Matern Child Health J 1997; 1: 217-227.