Research Article - Ophthalmology Case Reports (2017) Volume 1, Issue 1
Effects of Topical Timolol and Latanoprost by Tear Film Evaluation and Impression Cytology
Archimedes Lee D Agahan*, Jazel E Verde
Department of iSight Vision Center
- *Corresponding Author:
- Archimedes Lee D Agahan
Department of eye sight vision center
Tel: +632- 336-5203
Fax: +632- 416-6701
E-mail: adagahan@up.edu.ph
Accepted date: April 06, 2017
DOI: 10.35841/ophthalmology.1.1.8-14
Visit for more related articles at Ophthalmology Case ReportsAbstract
Aim or Purpose: The primary objective of this study is to describe the effects of application of topical timolol or latanoprost on the conjunctiva with the use of tear break-up test, Schirmer test and impression cytology; the secondary objective of this study is to evaluate the impact of dry eye symptoms on the quality of life among glaucoma patients.
Design: Prospective case series study.
Methods: All patients were asked to answer the ocular surface disease index (OSDI) questionnaire. Dry eye work-up consisted of tear break-up test, staining tests with fluorescein and Lissamine green, Schirmer test with anesthesia, and conjunctival impression cytology. Conjunctival samples were then examined, evaluated and their changes documented by a single ocular pathologist.
Results: A total of eighteen participants, including twenty eight eyes, fifteen in the timolol group and thirteen in the latanoprost group, were included in this study. Baseline characteristics were comparable between the two groups. There is a trend of decrease in tear break-up time with increasing duration of use of medication in the subgroup analysis for both the timolol and latanoprost groups. The latanoprost group showed a significant decrease in the Schirmer test but the timolol group did not. The conjunctival changes scores for the latanoprost group showed a significant increase with increasing duration of use of medication but the timolol group did not.
Conclusion: Increased duration of use of latanoprost showed significant goblet cell loss, as indicated by increased conjunctival changes score, and also a decreased Schirmer test result. Prolonged use of latanoprost showed significant increase in dry eye symptoms and severity as indicated by increased OSDI score. Long-term use of timolol showed no significant changes in OSDI score, TBUT score, Schirmer test result and conjunctival changes score.
Keywords
Dry Eye,impression Cytology, latanoprost, ocular Surface, disease index, schirmer test, tear break-up test, timolol
Introduction
Glaucoma represents a significant health problem and is an important cause of blindness worldwide (American Academy of Ophthalmology 2009). Its treatment includes long-term use of a single or a combination of topical medications; which poses the development of ocular and systemic side effects (American Academy of Ophthalmology 2009). One of the more common ocular side effects is dry eye (American Academy of Ophthalmology, 2009).Dry eye is a multifactorial disease of the tears and ocular surface (Reddy, 1991). It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.15 Symptoms that are associated with dry eye include discomfort; visual disturbance; and tear film instability with possible injury to the ocular surface (Reddy, 1991). These symptoms may be aggravated in dry environment; windy conditions or areas with low humidity (American Academy of Ophthalmology 2009) [1-6].
Diagnostic approaches to dry eye syndrome mainly involve the evaluation of the tear film and ocular cytology. Tear-film evaluation entails inspection and measurement of the tear meniscus (American Academy of Ophthalmology 2009). Tear breakup time is also used to evaluate the stability of the tear film. Breaks or spots that appear in the tear film in less than ten seconds are considered as abnormal (American Academy of Ophthalmology 2009). Other methods in the assessment of the tear film are the basic secretion test and the Schirmer 2 and Schirmer 1 (reflex secretion) tests (American Academy of Ophthalmology 2009). Measurement is done after five minutes and values of less than 5 and 10 millimeters for basic and reflex secretion tests respectively; are considered abnormal (American Academy of Ophthalmology 2009). Other tests that may be done in assessing dry eye syndrome include tear osmolarity; tear lysozyme and lactoferrin levels; and impression cytology (American Academy of Ophthalmology 2009)In this study; subjective evaluation of dry eye was done with the use of the ocular surface disease index (OSDI) questionnaire. Objective measurement of dry eye was done using tear break up test (TBUT); staining with fluorescein and Lissamine green; Schirmer test and conjunctival impression cytology.This study aims to investigate the association of dry eye disease and long-term use of topical anti-glaucoma medications; specifically timolol and latanoprost. The objectives of this study are to describe the effects of application of topical timolol and latanoprost with the use of tear break-up test (TBUT); staining with fluorescein and Lissamine green; Schirmer test and impression cytology; and to evaluate the impact of dry eye disease on quality of life among glaucoma patients with the use of the ocular surface disease index questionnaire. [6-10].
Methodology
A. Study population and design: The study design is a prospective case series study. This study was conducted among patients from the University of the Philippines-Philippine General Hospital; Department of Ophthalmology and Visual Sciences. A total of eighteen consecutive patients were recruited from the glaucoma clinic. The nature; objectives and methodology of the research were fully explained to all patients and an informed consent was signed by each patient prior to participation in this study. An ethics committee review approval was obtained prior to the initiation of this study [13-16].
Inclusion Criteria: Patients at least 18 years of age.
Patients diagnosed with any form of glaucoma from the glaucoma clinic treated with either of the following antiglaucoma medications: timolol or latanoprost.
With written informed consent to participate in the study
Exclusion Criteria: Any patient with history of penetrating trauma to any eye.
1. Any patient with history of ocular surgery to any eye.
2. Any patient with pre-existing primary or secondary ocular surface disease.
3. Any patient on any other topical medications other than timololand atanoprost.
4. Any patient with glaucoma that is not amenable to medical treatment only.
5. Any patient who will not consent for examination.
Information on all eligible patients was entered in a database once appropriate forms are filled. A single ophthalmologist conducted a complete ophthalmologic examination for all patients who participated in the study. Information such as age; sex; and nationality were documented. Examination began with the ocular surface disease index (OSDI) questionnaire. Scores for each of the 3 sub-categories were tallied and the severity of dry eye symptoms were compared with a reference table and noted in the OSDI evaluation form. A complete ophthalmologic examination; including visual acuity; refraction; tonometry; slit lamp examination; and indirect ophthalmoscopy were done and documented. Subsequently; dry eye workup consisting of tear break up test (TBUT); staining tests with fluorescein and Lissamine green; and Schirmer test with anesthesia were doneAfter the initial examination; conjunctival impression cytology was done by the same ophthalmologist. Conjunctival samples were examined; evaluated and documented by a single ocular pathologist. The patients and the results of their OSDI questionnaire; dry-eye workup and impression cytology were categorized based on the duration of their treatment as follows: 1 day to 3 months; more than 3 months to 6 months; more than 6 months to 12 months; more than 12 months to 24 months and more than 24 months [17-20].
B. Osdi questionnaire: The Ocular Surface Disease Index (OSDI) questionnaire is a valid and reliable tool for measuring the severity of dry eye disease (Report, 2007). It consists of 12 questions regarding symptoms of dry eye. The questionnaire is divided into three categories and the subtotal scores are obtained from each category. The participants were assisted in answering the questionnaire. The OSDI scores range from 0 to 100; and were qualitative measures of the severity of dry eye symptoms of the patients that participated in the study.
C. Tear Break-up Test (TBUT): A fluorescein-impregnated strip was moistened with a drop of BSS. The right lower lid was pulled down and the strip was tapped on the inferior palpebral conjunctiva. The same procedure was done on the left. The patient was positioned comfortably on the slit lamp; and was asked to look straight and to blink thrice. Under blue cobalt filter; the pre-corneal tear film was examined. Time was recorded from the last blink to the appearance of a dry spot. The tear break uptime was measured three times for each eye and then averaged afterwards.
D. Staining Tests with Fluorescein and Lissamine green: Conjunctival staining patterns using fluorescein were recorded according to Oxford Scheme (Bron, 2003). After documenting the fluorescein staining pattern; staining with Lissamine greenimpregnated strip was done. As with the fluorescein strip; a single drop of BSS was used to moisten the Lissamine green strip. The patient was positioned comfortably on the slit lamp; and was asked to look straight. The right lower lid was pulled down and the strip was tapped on the inferior palpebral conjunctiva. The same procedure was done on the left. Under a diffuse white light; corneal and conjunctival staining patterns using Lissamine green were recorded based on Oxford Scheme.
E. Schirmer Test : A standard Schirmer test strip was placed at the junction of lateral and middle third of the inferior fornices of both eyes. The patient was instructed to close his/her eyes for 5 minutes. Afterwards; the test strips were removed and measurements were recorded accordingly.
F. Impression Cytology: A single ophthalmologist got conjunctival samples on both eyes of patients. A strip of pre-cut cellulose acetate filter paper; with a pore size of 22 microns; 15 millimeters by 4 millimeters in size; was be used. A drop of proparacaine was instilled on each eye. The cellulose acetate filter strips were then applied on the following areas: superior palpebral conjunctiva; inferior palpebral conjunctiva and temporal bulbar conjunctiva. The rough side of the material was placed side down for three seconds with a glass rod. The filter strips with conjunctival specimen were fixated and stained with periodic acid-Schiff.
A single ophthalmologist-pathologist was then tasked to examine all of the specimens in a masked; non-randomized fashion. The adequacy of the specimen was first assessed. Using a microscope; the following parameters were examined: goblet cell density; nucleus-to-cytoplasm (N/C) ratios; and epithelial cell morphology. N/C ratios of non-goblet epithelial cells were estimated using a micrometer to measure the long axis of the cytoplasm and nucleus in the epithelial cells viewed under a light microscope at 100x. Mean goblet cell densities were determined for all specimens by averaging the number of goblet cells in five 1-mm2 areas as defined by a calibrated microscope grid at 100x. Conjunctival changes were graded from 0 (normal) to 5 (advanced keratinization) as described by Tseng (Thiel, 1997) (Table 1).
| Stage | Description |
|---|---|
| 0 | Normal goblet cell density with an N/C ratio 1/1 |
| 1 | Early loss of goblet cells without keratinization with an N/C ratio 1/2 to 1/3 |
| 2 | Total loss of goblet cells without keratinization and all epithelial cells moderately enlarged with an N/C ratio 1/4 |
| 3 | (Mild keratinization); all epithelial cells markedly squamoid with an N/C ratio 1/6 |
| 4 | (Moderate keratinization); more densely packed keratin filament; pyknotic nuclei with an N/C ratio 1/8 |
| 5 | (Advanced keratinization); shrunken cytoplasm |
Table 1: Grading of conjunctival cytological changes
G. Data analysis: The results of the OSDI questionnaire; dryeye workup and impression cytology were documented. Each participant; including subject eyes; were categorized into either of the two medications: timolol or latanoprost; and subsequently into any of the five subgroups based on the duration of their use of topical anti-glaucoma medication: 1 day to 3 months; more than 3 months to 6 months; more than 6 months to 12 months; more than 12 months to 24 months and more than 24 months. Paired t-test was used to compare the data between the two groups and linear regression was used to analyze results within the group subcategories.
H. Limitation of the study: One of the limitations of this study was that the investigator had to rely on the patients’ honesty during screening with regards to their compliance in applying their medication. A decline in the conjunctival goblet cell density due to aging may also manifest as dry eye syndrome. Aging as a contributory or confounding factor cannot be eliminated among the group using the topical timolol or latanoprost for more than twenty four months.
Results
A total of eighteen participants; including twenty eight eyes; fifteen in the timolol group and thirteen in the latanoprost group; were included in this study. Linear regression was used to analyze the data within the five subgroups. Analysis was separate between the timolol and latanoprost groups. The change among the OSDI scores; TBUT scores; Schirmer test result and conjunctival changes scores were plotted through time in months (Table 2).
| Timolol | Latanoprost | |
|---|---|---|
| Mean age | 55.4 | 54.8 |
| M:F ratio | 1:2.67 | 1:2 |
Table 2: Baseline characteristics of the timolol and latanoprost groups
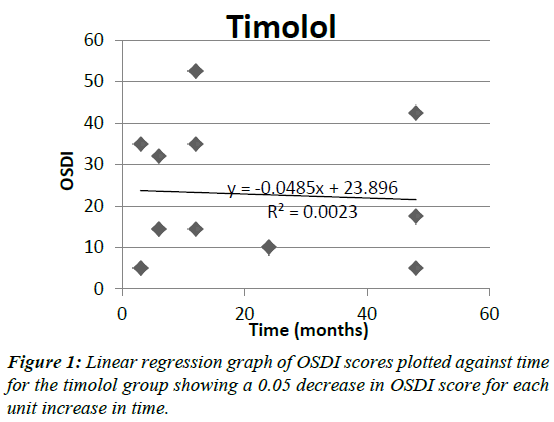
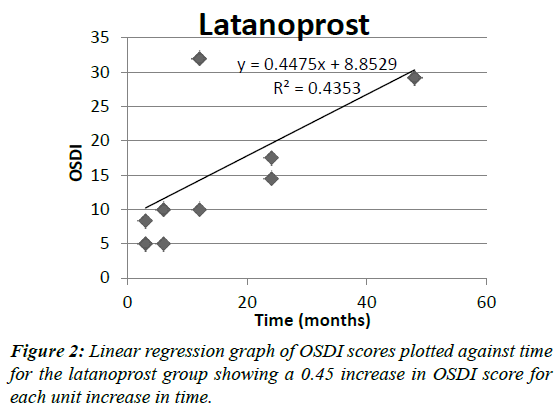
Figures 1 and 2 show the OSDI scores plotted through time for the two groups. In the timolol group; the OSDI score decreased by 0.05 for each unit increase in time with a p-value 0.8642. On the other hand; in the latanoprost group; the OSDI score significantly increased by 0.45 units for each unit increase in time with a p-value 0.01.
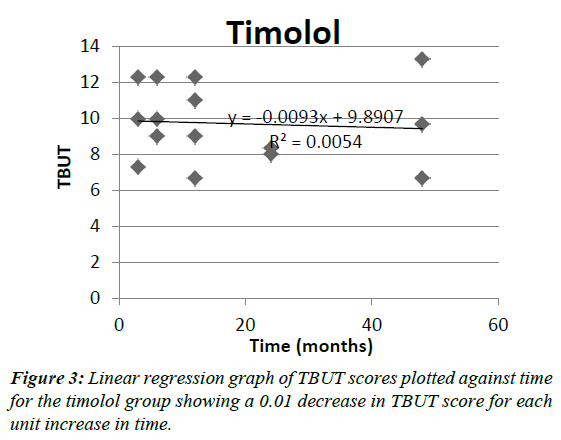
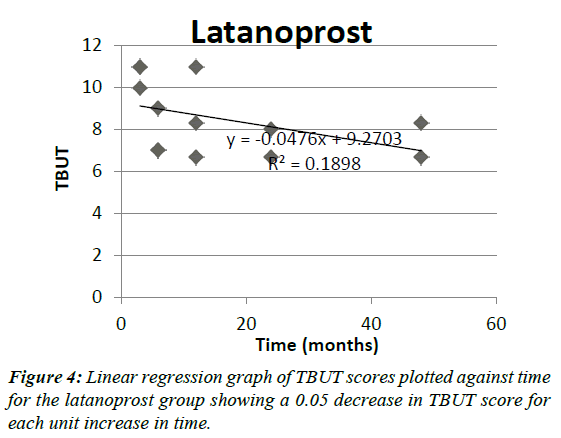
Figures 3 and 4 show the TBUT scores plotted through time for the two groups. In the timolol group; the TBUT score decreased by 0.01 for each unit increase in time; with a p-value 0.7947 On the other hand; in the latanoprost group; the TBUT score decreased by 0.05 for each unit increase in time; with a p-value 0.1367. For both groups; the decrease was not significant.
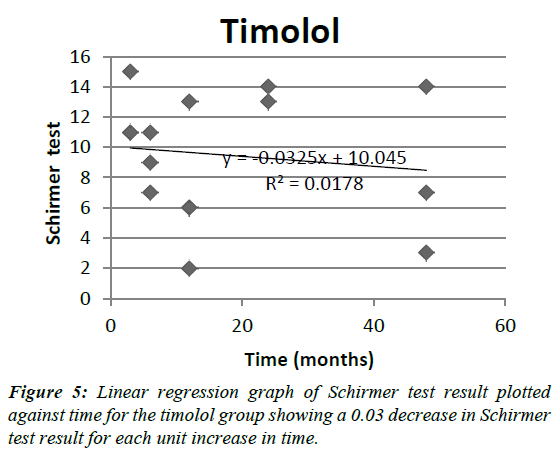
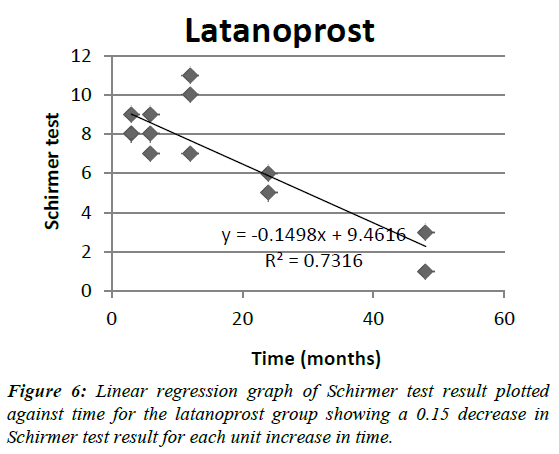
Figures 5 and 6 show the Schirmer test result plotted through time for the two groups. In the timolol group; the Schirmer test result decreased by 0.03 for each unit increase in time; with a p-value 0.6351. On the other hand; in the latanoprost group; the Schirmer test result significantly decreased by 0.15 for each unit increase in time; with a p-value 0.0002.
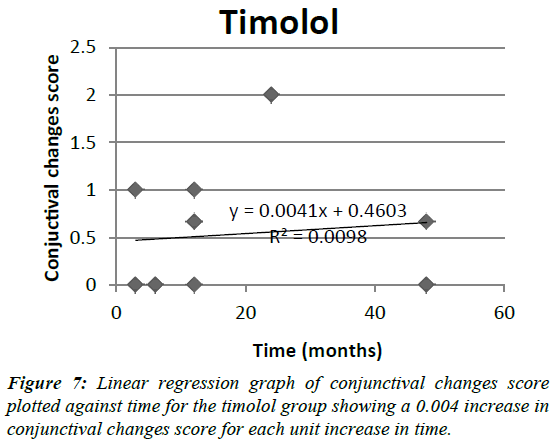
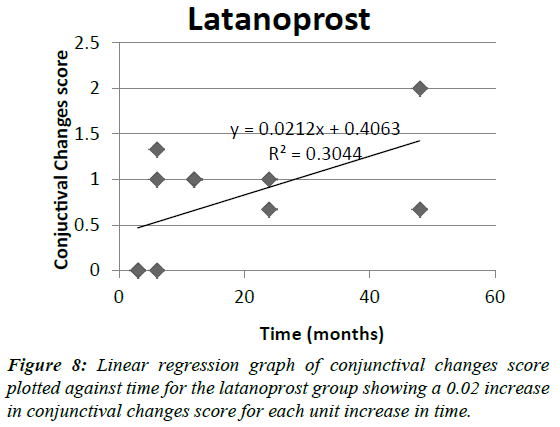
Figures 7 and 8 show the conjunctival changes score plotted through time for the two groups. In the timolol group; the conjunctival changes score increased by 0.004 for each unit increase in time; with a p-value 0.7261. On the other hand; in the latanoprost group; the conjunctival changes score significantly increased by 0.02 for each unit increase in time; with a p-value 0.0506.
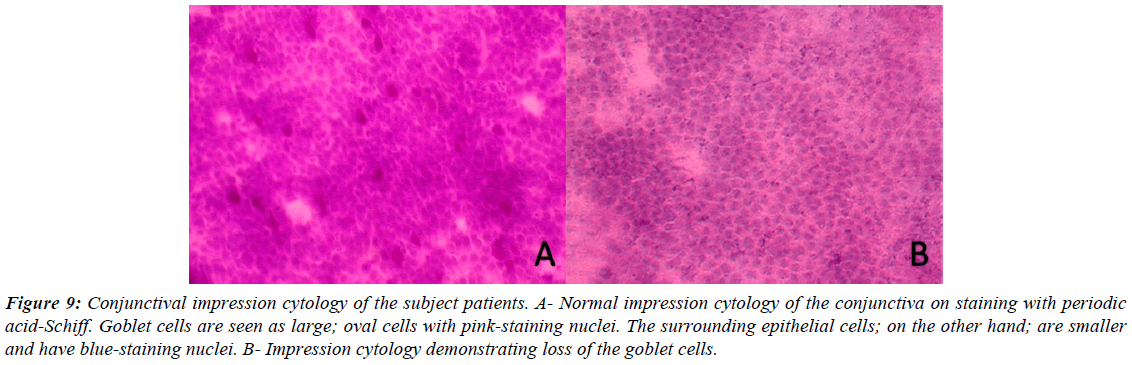
Paired t-test was used to compare the results between the timolol and latanoprost groups. It showed no significant difference between the OSDI values; TBUT values; Schirmer test result and conjunctival changes score of the two groups (Figure 9) [21,22].
Figure 9: Conjunctival impression cytology of the subject patients. A- Normal impression cytology of the conjunctiva on staining with periodic acid-Schiff. Goblet cells are seen as large; oval cells with pink-staining nuclei. The surrounding epithelial cells; on the other hand; are smaller and have blue-staining nuclei. B- Impression cytology demonstrating loss of the goblet cells.
Discussion
This study demonstrated goblet cell loss with increasing duration of use of both timolol and latanoprost. The conjunctival changes scores for the latanoprost group showed a statistically significant increase with increasing duration of use with a p-value of 0.05 but the increase for the timolol group was not significant. A similar study done by Hong et al. evaluated the conjunctival changes score among patients applying different anti-glaucoma medications; including timolol; latanoprost and a combination of timolol and latanoprost (Guenoun, 2005). Mean cytology scores for timolol; latanoprost and the combination of timolol and latanoprost are 0.20; 1.62 and 2.13; respectively (Hong, 2006). This is comparable with the results of this study which demonstrated mean cytology scores for timolol and latanoprost at 0.53 and 0.74; respectively. Both studies showed a higher conjunctival changes score for latanoprost. The study done by Hong et al also showed an even higher cytology score for a fixed combination of timolol and latanoprost (Hong, 2006).
Other studies have also demonstrated conjunctival metaplasia consequential to the use of topical anti-glaucoma drugs (Arici, 2000; Pisella, 2004 & Turacli, 1997). Studies were done by Arici et al and Turacli et al; tried to compare the changes in the conjunctiva in eyes treated with different antiglaucoma medications compared to a control group using impression cytology (Arici, 2000 & Turacli, 1997). Both studies demonstrated significant conjunctival metaplasia observed from the treatment group compared to the control group (Arici, 2000 & Turacli, 1997). A study done by Pisella et al compared the toxicity of preserved latanoprost; and preserved and unpreserved timolol on conjunctival cells by impression cytology and flow cytometry (Pisella, 2004). Their results showed that patients treated with preserved timolol and latanoprost have a significant decrease in mucin-expressing cells compared with normal eyes and patients treated with preservative-free timolol (Pisella, 2004).
Goblet cells produce the mucin component of the tear film. Mucin allows for stability of the tear film. Epithelial cell damage and goblet cell apoptosis are caused by a cascade of events that begins with tear hyperosmolarity (Report, 2007). Tear hyperosmolarity causes release of inflammatory mediators into the tears and consequently a decrease in goblet cell density (Report, 2007). One of the extrinsic etiologies that may also trigger the release of inflammatory mediators into the tears is the use of preserved topical medications (Report, 2007). Clinically; stability of the tear film is evaluated by the tear breakup time. This study demonstrated a decrease in tear breakup time with increasing duration of use of medication in the subgroup analysis for both the timolol and latanoprost groups. The decrease however for both groups was not significant. The study done by Arici et al also evaluated tear breakup time in addition to impression cytology in measuring changes in the ocular surface. Their results showed a significant decrease in tear breakup time among patients treated with antiglaucoma medications (Arici, 2000).
Schirmer test evaluates tear production. In this study; the latanoprost group showed a statistically significant decrease in the Schirmer test with a p-value of 0.0002. The timolol group also showed a decrease in Schirmer test value but the decrease was not significant. The study done by Arici et al also utilized the Schirmer test. Their results showed a significant decrease in Schirmer test among patients treated with anti-glaucoma medications (Arici, 2000).
Several components of eye drop formulations; including anti-glaucoma medications; may induce a toxic response on the ocular surface; but the most common offenders are the preservatives; such as benzalkonium chloride (Baudouin, 1994; Broadway, 1993; Broadway, 1994 & Guenoun, 2005). Changes induced on the ocular surface include inflammatory changes; an increase in keratinization and a decrease in the number of goblet cells. The pathophysiology of the decrease of mucin production secondary to the decrease in goblet cell density may be explained by two mechanisms as proposed in the study done by Pisella et al; either by chronic inflammatory reaction of the ocular surface induced by the preservative or; by direct toxicity of benzalkonium chloride on goblet cells (Pisella, 2004). The study of Guenoun et al. investigated the effects of three prostaglandin analogues: latanoprost; travoprost; bimatoprost; in different concentrations of benzalkonium chloride on conjunctiva-derived cells. The authors of the study proposed that the toxic effects on conjunctival cells in prolonged use of prostaglandin analogues may be attributed principally to the preservative benzalkonium chloride (Guenoun, 2005). However; total absence of toxic effects of the active compounds could not be absolutely eliminated because the preservative-free preparations of latanoprost; travaprost and bimatoprost were not available at the time of their study (Guenoun, 2005).
One limitation of this study; however; was that patients may have had different concentrations of the preservative in their medications. The differences in the concentration may also explain the decrease in TBUT score and Schirmer test result; and the increase in conjunctival changes score.
Among patients with prolonged use of latanoprost; there is a statistically significant increase in the OSDI score with a p-value of 0.01. This correlates with the increase in conjunctival changes score and decrease in tear breakup time demonstrated in the latanoprost group. Patients treated with timolol showed a decrease of the OSDI score with long-term use of the medication. The decreasing severity of dry eye symptoms among patients in the timolol group may be explained by nonsignificant changes in the TBUT score; Schirmer test result and conjunctival changes score.
Conclusion
Increased duration of use of latanoprost showed significant goblet cell loss; as indicated by increased conjunctival changes score; and also a decreased Schirmer test result. Also; prolonged use of latanoprost showed significant increase in dry eye symptoms and severity as indicated by increased OSDI score; which correlates with the goblet cell loss demonstrated by impression cytology with increase in the duration of use of the medication. Long-term use of timolol showed no significant changes in OSDI score; TBUT score; Schirmer test result and conjunctival changes score.
The authors recommend continuation of the study to include more patients and be able to come up with a more robust conclusion. Also; the authors recommend further investigation comparing preserved and non-preserved preparations of both timolol and latanoprost among newlydiagnosed glaucoma patients to better demonstrate the effect of preservatives; such as benzalkonium chloride; in inducing ocular surface changes with long-term use of anti-glaucoma medications.
Acknowledgements
Ms. Lilibeth Manganip; ocular pathologist from the Institute of Ophthalmology
References
- American Academy of Ophthalmology. External Disease and Cornea. San Francisco; 2008; 528-29.
- American Academy of Ophthalmology. Glaucoma. San Francisco.2009; 258.
- Arici M.K, Arici D.S, Topalkara A,et al. Adverse effects of topical anti-glaucoma drugs on the ocular surface. Clin Experiment Ophthalmol. 2010; 28:113-17.
- Baudouin C, Garcher C, Haouat N,et al. Expression of inflammatory membrane markers by conjunctival cells in chronically treated patients with glaucoma.Ophthalmology.1994;101:454-60.
- Baudouin C, Pisella P.J, Goldschild M,et al. Ocular surface inflammatory changes induced by topical antiglaucoma drugs, human and animal studies.Ophthalmology .2008 ;106: 556-63.
- Broadway D.C, Grierson I, O’Brien, C et al. Adverse effects of topical anti-laucomatous medications on the conjunctiva. Br J Ophthalmol.1998; 77: 590-6.
- Broadway D.C, Grierson I, O’Brien, C,et al. Adverse effects of topical anti-laucomatous medications. II, the outcome of filtration surgery. Arch Ophthalmol. 112;1446-54.
- Bron AJ, EvansVE, Smith JA. Grading of corneal and conjunctival staining in the context ofother dry eye tests. Cornea.2003; 22: 640-50.
- Grubbs J, Tolleson-Rinehart S, Huynh K,et al. A review of quality of life measures in dry eye questionnaires. Cornea.2003;33: 215-18.
- Guenoun J, Baudouin C, Rat P, et al. In Vitro Study of Inflammatory Potential and Toxicity Profile of Latanoprost; Travoprost; and Bimatoprost in Conjunctiva-Derived Epithelial Cells. Invest. Ophthalmol Vis Sci.2001;46: 2444-50.
- Hong S., Lee CS, Seo K.Yet al. Effects of topical antiglaucoma application on conjunctival impression cytology specimens. Am J Ophthalmol.2006; 142:185-6.
- MietzH, Niesen, U, Krieglstein, G.K . The effects of preservatives and anti-glaucomatous medication on histopathology of the conjunctiva. Graefes Arch Clin Exp Ophthalmol.2001; 232: 561-5.
- Nelson, J.Impression cytology. Cornea,2002; 7: 71-81.
- Pisella P.J, Debbasch C, Hamard P, et al. Conjunctival Proinflammatory and Proapoptotic Effects of Latanoprost and Preserved and Unpreserved Timolol, An Ex Vivo and In Vitro Study. Invest Ophthalmol Vis Sci.2001;45: 1360-8.
- Reddy P.R, Reddy S.C. Conjunctival impression cytology in dry eye states. Indian J.Ophthalmol.2003; 39: 22-4.
- Research in dry eye, report of the Research Subcommittee of the International Dry Eye WorkShop.2007; 5:179-193.
- Schiffman R, Christianson M, Jacobsen G,et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol.2001;118: 615-21.
- Singh R, Joseph A,Umapathy Tet al. Impression cytology of the ocular surface. Br J Ophthalmol.2003; 89: 1655-9.
- Tole D, McKelvie P, Daniell M. Reliability of impression cytology for the diagnosis of ocular surface squamous neoplasia employing the Biopore membrane. Br J Ophthalmol.2003; 85:154-8
- Thiel M, Bossart W , Bernauer. Improved impression cytology techniques for the immunopathological diagnosis of superficial viral infections. Br J Ophthalmol.2003:82: 984-8.
- TsengS.C.staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology.1995; 92: 728-33.
- Turacli E, Budak K., Kaur A,et al. The effects of long-term topical glaucoma medication on conjunctival impression cytology. Int Ophthalmol.1997;21:27-33.