Research Article - Current Pediatric Research (2022) Volume 26, Issue 6
Effectiveness of admission TOPRS score in predicting the outcome in pediatric inpatients - A prospective observational multicentric study.
Krithika AP1*, Sasikumar BR2, Senthil Kumar M3 and Sundari S1
1Department of Pediatrics, Sree Balaji Medical College and Hospital, Chennai, India
2Department of Pediatrics, Coimbatore Medical College and Hospital, Coimbatore, India
3Department of Pediatrics, Government Medical College Hospital, Tiruppur, India
- *Corresponding Author:
- Krithika AP, Department of Pediatrics, Sree Balaji Medical College and Hospital, Chennai, India, E-mail: krithika.ap@bharathuniv.ac.in
Received: 02 June, 2022, Manuscript No. AAJCP-22-59857; Editor assigned: 03 June, 2022, PreQC No. AAJCP-22-59857(PQ); Reviewed: 10 June, 2022, QC No. AAJCP-22-59857; Revised: 22 June, 2022, Manuscript No. AAJCP-22-59857(R); Published: 29 June, 2022, DOI:10.35841/0971-9032.26.6.1440-1447.
Abstract
Introduction: Identification and triage of seriously ill patients visiting emergency department is very important for prioritization of care. One of the key tasks in both hospital ER and primary-care settings is therefore, to distinguish children who may have serious infections (e.g., meningitis, bacteremia) or complications from infection (e.g., hypoxia from bronchiolitis, dehydration from gastroenteritis) from the vast majority with self-limiting or minor infections that can be safely managed at home. A simple and effective scoring system using clinical variables can help in guiding through the process of triage. TOPRS score consists of simple clinical variables and can even be done by a paramedic. TOPRS stands for: • T-Temperature • O-Oxygen saturation • P-Pulse rate • R -Respiratory rate • S-Seizure In our study, scoring system, TOPRS uses only vital signs to predict the severity of illness and mortality in pediatric emergency department was evaluated, as a multicentric study, to see if it is applicable and reliable in the existing setup in Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai. Aims and objectives of study: To identify sick children in a busy pediatric outpatient department in a tertiary care hospital by using a simple scoring system. (TOPRS) Secondary objective: To ensure timely and appropriate treatment in a resource poor setting. Material and methods: Children admitted in pediatric wards and PICU at Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai from March 2021 to January 2022. Type of study: Prospective observational multicentric study. Inclusion criteria: Infants from 1month to 1 year and children aged 1 year to 12 years admitted in pediatric ward and PICU Results and observation: This study was conducted in Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, by enrolling 600 children after getting ethical committee clearance. The predictive ability of the test was arrived at, by using the Receiver Operating Curve (ROC). The distribution of each variable in the study population was analyzed and the association between each of these variables to the outcome was also analyzed. The association between the final score and outcome was analyzed using the receiver operating curve. This study included study group with the mean age of 4.87 years. The distribution of boys was greater than that of girls in this study. Boys 51.8%; Girls 48.2%. There was a statistically significant correlation between temperature abnormality, oxygen saturation, pulse rate, respiratory rate and seizures and the adverse outcome.
Conclusion: The TOPRS score is a simple scoring system using simple clinical variables and does not require expertise to perform. This study has shown a definite correlation between the TOPRS score and the poor outcome. It has also revealed that, higher the score, longer the ICU stays. Among the variables, the temperature and the heart rate abnormality were associated with poorer outcomes in comparison to the other variables.
Introduction: Identification and triage of seriously ill patients visiting emergency department is very important for prioritization of care. One of the key tasks in both hospital ER and primary-care settings is therefore, to distinguish children who may have serious infections (e.g., meningitis, bacteremia) or complications from infection (e.g., hypoxia from bronchiolitis, dehydration from gastroenteritis) from the vast majority with self-limiting or minor infections that can be safely managed at home. A simple and effective scoring system using clinical variables can help in guiding through the process of triage.
TOPRS score consists of simple clinical variables and can even be done by a paramedic. TOPRS stands for:
• T-Temperature
• O-Oxygen saturation
• P-Pulse rate
• R -Respiratory rate
• S-Seizure
In our study, scoring system, TOPRS uses only vital signs to predict the severity of illness and mortality in pediatric emergency department was evaluated, as a multicentric study, to see if it is applicable and reliable in the existing setup in Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai.
Aims and objectives of study: To identify sick children in a busy pediatric outpatient department in a tertiary care hospital by using a simple scoring system. (TOPRS)
Secondary objective: To ensure timely and appropriate treatment in a resource poor setting.
Material and methods: Children admitted in pediatric wards and PICU at Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai from March 2021 to January 2022.
Type of study: Prospective observational multicentric study.
Inclusion criteria: Infants from 1month to 1 year and children aged 1 year to 12 years admitted in pediatric ward and PICU.
Results and observation: This study was conducted in Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, by enrolling 600 children after getting ethical committee clearance. The predictive ability of the test was arrived at, by using the Receiver Operating Curve (ROC). The distribution of each variable in the study population was analyzed and the association between each of these variables to the outcome was also analyzed. The association between the final score and outcome was analyzed using the receiver operating curve.
This study included study group with the mean age of 4.87 years. The distribution of boys was greater than that of girls in this study. Boys 51.8%; Girls 48.2%.
There was a statistically significant correlation between temperature abnormality, oxygen saturation, pulse rate, respiratory rate and seizures and the adverse outcome.
Conclusion: The TOPRS score is a simple scoring system using simple clinical variables and does not require expertise to perform. This study has shown a definite correlation between the TOPRS score and the poor outcome. It has also revealed that, higher the score, longer the ICU stays. Among the variables, the temperature and the heart rate abnormality were associated with poorer outcomes in comparison to the other variables.
Keywords
Oxygen saturation, Pulse rate, Respiratory rate, seizures.
Introduction
Identification and triage of seriously ill patients visiting emergency department is very important for prioritization of care and answering parent's queries about outcome, hospital stay and cost of treatment especially in developing countries like India where medical insurance of public is not yet developed.
Despite the high burden of pediatric mortality from preventable conditions in low and middle income countries and the existence of multiple tools to prioritize critically ill children in low-resource settings, no analysis of the reliability and validity of these tools in identifying critically ill children in these scenarios exists [1,2].
A simple and effective scoring system using clinical variables can help in guiding through the process of triage. Pediatrics being a very challenging field where failure to recognize serious illness at the earliest, may lead to loss of the child or the child may end up with a sequelae. While on the contrary, early recognition and timely intervention could save the child without sequelae [3].
Most scoring systems which are available are either applicable only to ICU patients or need laboratory parameters and hence cannot be done at admission and are not useful for triage. TOPRS score consists of simple clinical variables and can even be done by a paramedic [4].
TOPRS stands for:
• T-Temperature
• O-Oxygen saturation
• P-Pulse rate
• R -Respiratory rate
• S-Seizure
In our study, scoring system “TOPRS” uses only vital signs to predict the severity of illness and mortality in pediatric emergency department was evaluated to see if it is applicable and reliable to triage children.
Aims and Objectives of Study
Primary objective
To identify sick children in a busy pediatric outpatient department in a tertiary care hospital by using a simple scoring system (TOPRS).
Secondary objective: To ensure timely and appropriate treatment in a resource poor setting.
Material and Methods
Source of data
Children admitted in pediatric wards and PICU at Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, over a period of 1 year from March 2021 to January 2022.
Type of study: Prospective observational multicentric study.
Inclusion criteria: Infants from 1 month to 1 year and children aged 1 year to 12 years admitted in pediatric ward and PICU.
Exclusion criteria: Children with thalassemia admitted for blood transfusion.
• Children with Hemophilia admitted for factor transfusion.
• Children admitted for Rabies Immunoglobulin administration.
• Children less than 1 month.
• Those who left against medical advice.
• Brought dead patient
• Those with surgical problems.
Study area: Coimbatore Medical College and hospital, Government Medical College and Hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, Department of Pediatrics.
Study duration: March 2021 to January 2022.
Method of measurement of outcome
The clinical variables (temperature, oxygen saturation, pulse rate, respiratory rate, and seizures) were recorded on admission. Temperature was measured at the axilla using a digital thermometer. Oxygen saturation was measured using a fingertip pulse oximeter, pulse rate, respiratory rate were measured for a full minute, and seizure was recorded if present (Table 1).
| S.no | Variable | Abnormal ranges | ||
|---|---|---|---|---|
| 1 | Temperature | >38*C; <36*C | ||
| 2 | Saturation | <90% | ||
| 3 | Pulse rate | Age | Maximum | Minimum |
| 1 yr | >180 | <100 | ||
| 2 yr to 5 yr | >140 | <90 | ||
| 6 yr to 12 yr | >130 | |||
| 4 | Respiratory rate | 1 yr | >60 | Respiratory support |
| 2 yr to 5 yr | >50 | |||
| 6 yr to 12 yr | >20 | |||
| 5 | Sensorium | ALOC V/P/U | ||
| 6 | Seizures | Present | ||
Table 1. Measurement of temperature saturation, pulse rate, respiratory rate, sensorium, seizures with their abnormal ranges.
Results and Observation
This study was conducted in Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, by enrolling 600 children after getting ethical committee clearance. The predictive ability of the test was arrived at by using the
Receiver Operating Curve (ROC). The distribution of each variable in the study population was analyzed and the association between each of these variables to the outcome was also analyzed. The association between the final score and outcome was analyzed using the receiver operating curve (Table 2).
| S.no | Age group(years) | No. of cases | Percentage |
|---|---|---|---|
| 1 | <5 | 340 | 56.70% |
| 2 | 5 | 24 | 4% |
| 3 | >5 | 236 | 39.30% |
| 4 | Total | 600 | 100% |
Table 2. Descriptive analysis of age group in study population (N=600).
This is the distribution of age group in the study population. Out of 600 children 56.7% belong to <5 years, 39.3% belong to >5 years category. This study included study group with the mean age of 4.87 years (Table 3).
| S.No | Gender | No. of cases | Percentage |
|---|---|---|---|
| 1 | Male children | 311 | 51.80% |
| 2 | Female children | 289 | 48.20% |
| 3 | Total | 600 | 100% |
Table 3. Analysis of gender in the study population (N=600).
The distribution of boys was greater than that of girls in this study. Boys-51.8% Girls-48.2%.
Distribution of the score variables
Temperature: This is the distribution of temperature within the study population. 448 children had normal range temperature on admission and 152 children had temperature within the abnormal range (Table 4).
| S.No | Temp deg F | No of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 448 | 74.70% |
| 2 | Abnormal | 152 | 25.30% |
| 3 | Total | 600 | 100% |
Table 4. Descriptive analysis of temperature in the study population (N=600).
Saturation
This is the distribution of saturation within the study population. 551 children had normal saturation on admission and 49 of them had saturation in the abnormal range (Table 5).
| S.No | SPO2 | No of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 551 | 91.80% |
| 2 | Abnormal | 49 | 8.20% |
| 3 | Total | 600 | 100% |
Table 5. Analysis of SPO2 in study population (N=600).
Heart rate: 470 children had normal heart rate, 130 children had abnormal range of heart rate (Table 6).
| S.No | HR | No. of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 470 | 78.30% |
| 2 | Abnormal | 130 | 21.70% |
| 3 | Total | 600 | 100% |
Table 6. Analysis of heart rate in the study population (N=600).
Respiratory rate: 521 children had normal respiratory rate while 79 had abnormal respiratory rate (Table 7).
| RR | No. of cases | Percentage |
|---|---|---|
| Normal | 521 | 86.80% |
| Abnormal | 79 | 13.20% |
| Total | 600 | 100% |
Table 7. Analysis of respiratory rate in the study population (N=600).
Sensorium: 559 cases had normal sensorium on admission and 41 children had altered sensorium on admission (Table 8).
| S.No | Sensorium | No. of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 559 | 93.20% |
| 2 | Abnormal | 41 | 6.80% |
| 3 | Total | 600 | 100% |
Table 8. Analysis of sensorium in the study population (N=600).
Seizures: 563 children had no seizures on admission, 37 children had seizures on admission (Tables 9 and 10).
| S.No | Seizures | No. of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 563 | 93.20% |
| 2 | Abnormal | 37 | 6.20% |
| 3 | Total | 600 | 100% |
Table 9. Analysis of Seizures in the study population (N=600).
| S.No | Outcome | No. of cases | Percentage |
|---|---|---|---|
| 1 | Discharge | 550 | 91.70% |
| 2 | Death | 50 | 8.30% |
| 3 | Total | 600 | 100% |
Table 10. Analysis of outcome in the study population (N=600).
Association between abnormality in each variable and outcome
There was a statistically significant correlation between temperature abnormality and the outcome of children. Those children having an abnormal temperature had a poor outcome (Table 11).
| Temp deg F | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 424 (77.1%) | 24 (48%) | 448 (74.7%) | 20.506 | <0.001 |
| Abnormal | 126 (22.9%) | 26 (52%) | 152 (25.3%) | ||
| Total | 550 (100%) | 50 (100%) | 600 (100%) | ||
Table 11. Comparison of temperature (deg F ) and outcome (N=600).
Spo2 and outcome
There was a statistically significant correlation between saturation abnormality and outcome with those children having an abnormal range of temperature having an adverse outcome (Table 12).
| Spo2 | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 540 (98.2%) | 11 (22%) | 551(91.8%) | 354.68 | <0.001 |
| Abnormal | 10 (1.8%) | 39 (78%) | 49 (8.2%) | ||
| Total | 550 (100%) | 50 (100%) | 600 (100%) | ||
Table 12. Comparison of Spo2 and outcome (N=600).
Heart rate and outcome
There was a statistically significant correlation between heart rate and the outcome Children having abnormal heart rate had an adverse outcome than those with normal range of heart rate (Table 13).
| RR | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 512 (93.1%) | 9 (18%) | 521(86.8%) | 226.04 | <0.001 |
| Abnormal | 38 (6.9%) | 41 (82%) | 79(13.2% | ||
| Total | 550 (100%) | 50(100%) | 600 (100%) | ||
Table 13. Comparison of heart rate and outcome (N=600).
Respiratory rate and outcome
There was a statistically significant correlation between respiratory rate and outcome. 82% of those with poor outcome had an abnormal respiratory rate (Tables 14 and 15).
| RR | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 512 (93.1%) | 9 (18%) | 521(86.8%) | 226.04 | <0.001 |
| Abnormal | 38 (6.9%) | 41 (82%) | 79(13.2% | ||
| Total | 550 (100%) | 50(100%) | 600 (100%) | ||
Table 14. Comparison of respiratory rate and outcome (N=600).
| Sensorium | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 535 (97.3%) | 24(48%) | 559(93.2%) | 174.784 | <0.001 |
| Abnormal | 15 (2.7%) | 26(52%) | 41(6.8%) | ||
| Total | 550 (100%) | 50(100%) | 600(100%) | ||
Table 15. Comparison of sensorium and outcome (N=600).
There is a statistically significant correlation between sensorium and outcome. Among the 41 children who had altered sensorium, 63% died (Table 16).
| Seizures | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 521(94.7%) | 42 (84%) | 563(93.8%) | ||
| Abnormal | 29 (5.3%) | 8 (16%) | 37 (6.2%) | 9.115 | 0.003 |
| Total | 550(100%) | 50 (100%) | 600(100%) | ||
Table 16. Comparison of Seizures and outcome (N=600).
6.2% of the study population had seizures. Seizures were present in 16% of all deaths. There was a statistically significant correlation between seizure occurrence and outcome (Table 17).
| S.No | Total score | Total No. of children | Outcome | Chi square | P value | |
|---|---|---|---|---|---|---|
| Discharge (n=550) | Death (n=50) | |||||
| 1 | 0 | 323 | 323 | 0 | 429.015 | <0.001 |
| 2 | 1 | 166 | 160 | 6 | ||
| 3 | 2 | 63 | 60 | 3 | ||
| 4 | 3 | 19 | 7 | 12 | ||
| 5 | 4 | 12 | 0 | 12 | ||
| 6 | 5 | 10 | 0 | 10 | ||
| 7 | 6 | 7 | 0 | 7 | ||
Table 17. Comparison of total score and outcome (N=600).
Total score and outcome
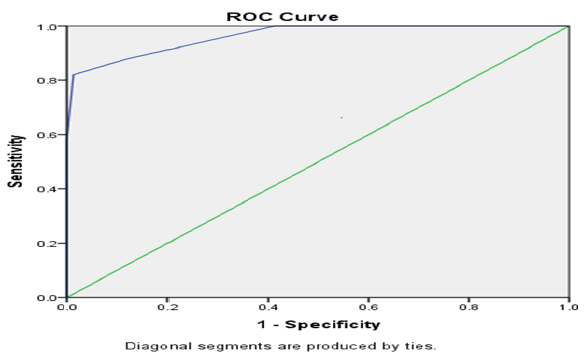
When the total TOPRS score was zero, there was no mortality, whereas when the total score ranged from 4 to 6, there was 100% mortality (P value <0.001) (Figure 1 and Table 18).
| Test result variable(s): Total score | ||||
|---|---|---|---|---|
| Area under the curve | Std. Error | P value | 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||
| 0.962 | 0.013 | <0.001 | 0.936 | 0.988 |
Table 18. Predictive validity of total score in predictive mortality.
Data was analyzed bi-variably and multivariably using regression analysis. In the present study the area under the curve was found to be 0.96 i.e. the predictive value of the score was 96.2%.
A score of 2.5 has maximum discrimination with sensitivity of 84% and specificity of 96%. The predictability of severity of illness on admission by the TOPRS score was excellent and was found to be statistically significant (p value <0.001) and uses less time, less resources, less manpower. Harmesh et al. conducted a study entitled “A simple clinical score TOPRS to predict outcome in pediatric emergency department in a teaching hospital in India’s during the year 2011 in Dayanand medical college and hospital, Ludhiana, India.
They found that out of six variable temperature, oxygen saturation, respiratory rate, were found to be significantly associated with mortality whereas in the present study it was found that abnormality in all the six variable was significantly associated with mortality. They also found that mortality increased with increase in number of abnormal variables [5]. In the present study also, similar results were obtained. Predictive value of the score was found to be 81.7 whereas in the present study the predictive value of the score was 96%. In another study conducted by Dr. Arthilatha at Thirunelveli medical college,titled “A simple clinical scoring system TOPRS to predict the outcome and mortality in paediatrics emergency department in TVMCH”, it was found that the performance of the TOPRS score was excellent and the predictive value of the score was 92% which was almost similar to the present study [4]. It was also found that mortality increases with decreasing age which is also similar to the present study.
It was found that the individual variable, pulse rate, respiratory rate, SpO2, and Senorium, each was significantly associated with mortality whereas in present study all the individual variables had a statistical significant association with mortality. In an article published by Salah et al. entitled “Use of vital signs as predictors for serious bacterial infections in children with acute febrile illness in a pediatric emergency setting in Sudan in the year 2014, it was found that tachycardia and tachypnoea were the most sensitive and specific indicator in predicting serious bacterial infections with 80%; 86.6% sensitivity and 97.4%, 83.7% specificity respectively [6].
This present study also substantiates these findings. It was found that temperature and severe hypoxaemia were least sensitive but highly specific signs of serious bacterial infections in pediatric emergency department and has comparable sensitivity to more complicated triage systems. In a study done by Salamati et al. entitled validation of pediatric index of mortality 2 scoring system in a single pediatric intensive care unit in lran, it was found that the area under the ROC curve was 0.795 (0.715-0.875 for 95% confidence interval) and standardized mortality ratio was 1.8 which is less than that obtained in this present study [7].
TOPRS score of 3 was significantly associated with mortality in the previous study done at the institute of child health, Chennai in the year 2006 to validate the usefulness of PRISM III score in predicting the mortality in PICU involving the same age group, the area under ROC was 0.853 i.e., 85% correct in predicting mortality. The TOPRS score has performed better than PRISM score in predicting mortality in this population with area under ROC being 0.96. In conclusion, on admission TOPRS score has performed very well in predicting the outcome of patients with area under the curve of 0.96 i.e., 96% correct prediction of severity.
Hence the utilization of the TOPRS score will help in:
• Mortality prediction.
• Identification of the sick children requiring urgent intervention.
• Counseling of the caretakers of the condition of their child.
• Proper utilization of resources.
Conclusion
• TOPRS score is a simple scoring system using simple clinical variables and does not require expertise to perform.
• This study has shown a definite correlation between the TOPRS score and the poor outcome.
• It has also revealed that, higher the score, longer the ICU stays.
• Among the variables, the temperature and the heart rate abnormality were associated with poorer outcomes in comparison to the other variables.
References
- https://pubmed.ncbi.nlm.nih.gov/23056866/
- Anthony RB, David H, Stephanie B, et al. Assessment and optimization of mortality prediction tools for admissions to pediatric intensive care in the United Kingdom. Pediatrics 2006; 117(4): e733-42.
- https://www.aap.org/en/my-account/login/
- http://repository-tnmgrmu.ac.in/5870/
- Barbara HF, Amber H, Brenda K, et al. Transdisciplinary Obesity Prevention Research Sciences (TOPRS) curriculum increases knowledge about complex causes and consequences of obesity for undergraduate students. Front Public Health 2019; 22(1): 97.
- https://www.semanticscholar.org/paper/The-use-of-vital-signs-as-predictors-for-serious-in-Salah-Ahmed/3a7ea116a64b7fffff675b8ea9623694981217e8
- Salamati P, Talaee S, Eghbalkhah A, et al. Validation of pediatric index of mortality-2 scoring system in a single pediatric intensive care unit in Iran. Iran J Pediatr 2012; 22(4): 481.
References
Introduction
Identification and triage of seriously ill patients visiting emergency department is very important for prioritization of care and answering parent's queries about outcome, hospital stay and cost of treatment especially in developing countries like India where medical insurance of public is not yet developed.
Despite the high burden of pediatric mortality from preventable conditions in low and middle income countries and the existence of multiple tools to prioritize critically ill children in low-resource settings, no analysis of the reliability and validity of these tools in identifying critically ill children in these scenarios exists [1,2].
A simple and effective scoring system using clinical variables can help in guiding through the process of triage. Pediatrics being a very challenging field where failure to recognize serious illness at the earliest, may lead to loss of the child or the child may end up with a sequelae. While on the contrary, early recognition and timely intervention could save the child without sequelae [3].
Most scoring systems which are available are either applicable only to ICU patients or need laboratory parameters and hence cannot be done at admission and are not useful for triage. TOPRS score consists of simple clinical variables and can even be done by a paramedic [4].
TOPRS stands for:
• T-Temperature
• O-Oxygen saturation
• P-Pulse rate
• R -Respiratory rate
• S-Seizure
In our study, scoring system “TOPRS” uses only vital signs to predict the severity of illness and mortality in pediatric emergency department was evaluated to see if it is applicable and reliable to triage children.
Aims and Objectives of Study
Primary objective
To identify sick children in a busy pediatric outpatient department in a tertiary care hospital by using a simple scoring system (TOPRS).
Secondary objective: To ensure timely and appropriate treatment in a resource poor setting.
Material and Methods
Source of data
Children admitted in pediatric wards and PICU at Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, over a period of 1 year from March 2021 to January 2022.
Type of study: Prospective observational multicentric study.
Inclusion criteria: Infants from 1 month to 1 year and children aged 1 year to 12 years admitted in pediatric ward and PICU.
Exclusion criteria: Children with thalassemia admitted for blood transfusion.
• Children with Hemophilia admitted for factor transfusion.
• Children admitted for Rabies Immunoglobulin administration.
• Children less than 1 month.
• Those who left against medical advice.
• Brought dead patient
• Those with surgical problems.
Study area: Coimbatore Medical College and hospital, Government Medical College and Hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, Department of Pediatrics.
Study duration: March 2021 to January 2022.
Method of measurement of outcome
The clinical variables (temperature, oxygen saturation, pulse rate, respiratory rate, and seizures) were recorded on admission. Temperature was measured at the axilla using a digital thermometer. Oxygen saturation was measured using a fingertip pulse oximeter, pulse rate, respiratory rate were measured for a full minute, and seizure was recorded if present (Table 1).
| S.no | Variable | Abnormal ranges | ||
|---|---|---|---|---|
| 1 | Temperature | >38*C; <36*C | ||
| 2 | Saturation | <90% | ||
| 3 | Pulse rate | Age | Maximum | Minimum |
| 1 yr | >180 | <100 | ||
| 2 yr to 5 yr | >140 | <90 | ||
| 6 yr to 12 yr | >130 | |||
| 4 | Respiratory rate | 1 yr | >60 | Respiratory support |
| 2 yr to 5 yr | >50 | |||
| 6 yr to 12 yr | >20 | |||
| 5 | Sensorium | ALOC V/P/U | ||
| 6 | Seizures | Present | ||
Table 1. Measurement of temperature saturation, pulse rate, respiratory rate, sensorium, seizures with their abnormal ranges.
Results and Observation
This study was conducted in Coimbatore medical college and hospital, government medical college and hospital, Tiruppur and Sree Balaji medical college and hospital, Chennai, by enrolling 600 children after getting ethical committee clearance. The predictive ability of the test was arrived at by using the
Receiver Operating Curve (ROC). The distribution of each variable in the study population was analyzed and the association between each of these variables to the outcome was also analyzed. The association between the final score and outcome was analyzed using the receiver operating curve (Table 2).
| S.no | Age group(years) | No. of cases | Percentage |
|---|---|---|---|
| 1 | <5 | 340 | 56.70% |
| 2 | 5 | 24 | 4% |
| 3 | >5 | 236 | 39.30% |
| 4 | Total | 600 | 100% |
Table 2. Descriptive analysis of age group in study population (N=600).
This is the distribution of age group in the study population. Out of 600 children 56.7% belong to <5 years, 39.3% belong to >5 years category. This study included study group with the mean age of 4.87 years (Table 3).
| S.No | Gender | No. of cases | Percentage |
|---|---|---|---|
| 1 | Male children | 311 | 51.80% |
| 2 | Female children | 289 | 48.20% |
| 3 | Total | 600 | 100% |
Table 3. Analysis of gender in the study population (N=600).
The distribution of boys was greater than that of girls in this study. Boys-51.8% Girls-48.2%.
Distribution of the score variables
Temperature: This is the distribution of temperature within the study population. 448 children had normal range temperature on admission and 152 children had temperature within the abnormal range (Table 4).
| S.No | Temp deg F | No of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 448 | 74.70% |
| 2 | Abnormal | 152 | 25.30% |
| 3 | Total | 600 | 100% |
Table 4. Descriptive analysis of temperature in the study population (N=600).
Saturation
This is the distribution of saturation within the study population. 551 children had normal saturation on admission and 49 of them had saturation in the abnormal range (Table 5).
| S.No | SPO2 | No of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 551 | 91.80% |
| 2 | Abnormal | 49 | 8.20% |
| 3 | Total | 600 | 100% |
Table 5. Analysis of SPO2 in study population (N=600).
Heart rate: 470 children had normal heart rate, 130 children had abnormal range of heart rate (Table 6).
| S.No | HR | No. of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 470 | 78.30% |
| 2 | Abnormal | 130 | 21.70% |
| 3 | Total | 600 | 100% |
Table 6. Analysis of heart rate in the study population (N=600).
Respiratory rate: 521 children had normal respiratory rate while 79 had abnormal respiratory rate (Table 7).
| RR | No. of cases | Percentage |
|---|---|---|
| Normal | 521 | 86.80% |
| Abnormal | 79 | 13.20% |
| Total | 600 | 100% |
Table 7. Analysis of respiratory rate in the study population (N=600).
Sensorium: 559 cases had normal sensorium on admission and 41 children had altered sensorium on admission (Table 8).
| S.No | Sensorium | No. of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 559 | 93.20% |
| 2 | Abnormal | 41 | 6.80% |
| 3 | Total | 600 | 100% |
Table 8. Analysis of sensorium in the study population (N=600).
Seizures: 563 children had no seizures on admission, 37 children had seizures on admission (Tables 9 and 10).
| S.No | Seizures | No. of cases | Percentage |
|---|---|---|---|
| 1 | Normal | 563 | 93.20% |
| 2 | Abnormal | 37 | 6.20% |
| 3 | Total | 600 | 100% |
Table 9. Analysis of Seizures in the study population (N=600).
| S.No | Outcome | No. of cases | Percentage |
|---|---|---|---|
| 1 | Discharge | 550 | 91.70% |
| 2 | Death | 50 | 8.30% |
| 3 | Total | 600 | 100% |
Table 10. Analysis of outcome in the study population (N=600).
Association between abnormality in each variable and outcome
There was a statistically significant correlation between temperature abnormality and the outcome of children. Those children having an abnormal temperature had a poor outcome (Table 11).
| Temp deg F | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 424 (77.1%) | 24 (48%) | 448 (74.7%) | 20.506 | <0.001 |
| Abnormal | 126 (22.9%) | 26 (52%) | 152 (25.3%) | ||
| Total | 550 (100%) | 50 (100%) | 600 (100%) | ||
Table 11. Comparison of temperature (deg F ) and outcome (N=600).
Spo2 and outcome
There was a statistically significant correlation between saturation abnormality and outcome with those children having an abnormal range of temperature having an adverse outcome (Table 12).
| Spo2 | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 540 (98.2%) | 11 (22%) | 551(91.8%) | 354.68 | <0.001 |
| Abnormal | 10 (1.8%) | 39 (78%) | 49 (8.2%) | ||
| Total | 550 (100%) | 50 (100%) | 600 (100%) | ||
Table 12. Comparison of Spo2 and outcome (N=600).
Heart rate and outcome
There was a statistically significant correlation between heart rate and the outcome Children having abnormal heart rate had an adverse outcome than those with normal range of heart rate (Table 13).
| RR | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 512 (93.1%) | 9 (18%) | 521(86.8%) | 226.04 | <0.001 |
| Abnormal | 38 (6.9%) | 41 (82%) | 79(13.2% | ||
| Total | 550 (100%) | 50(100%) | 600 (100%) | ||
Table 13. Comparison of heart rate and outcome (N=600).
Respiratory rate and outcome
There was a statistically significant correlation between respiratory rate and outcome. 82% of those with poor outcome had an abnormal respiratory rate (Tables 14 and 15).
| RR | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 512 (93.1%) | 9 (18%) | 521(86.8%) | 226.04 | <0.001 |
| Abnormal | 38 (6.9%) | 41 (82%) | 79(13.2% | ||
| Total | 550 (100%) | 50(100%) | 600 (100%) | ||
Table 14. Comparison of respiratory rate and outcome (N=600).
| Sensorium | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 535 (97.3%) | 24(48%) | 559(93.2%) | 174.784 | <0.001 |
| Abnormal | 15 (2.7%) | 26(52%) | 41(6.8%) | ||
| Total | 550 (100%) | 50(100%) | 600(100%) | ||
Table 15. Comparison of sensorium and outcome (N=600).
There is a statistically significant correlation between sensorium and outcome. Among the 41 children who had altered sensorium, 63% died (Table 16).
| Seizures | Outcome | Total | Chi square | P value | |
|---|---|---|---|---|---|
| Discharge | Death | ||||
| Normal | 521(94.7%) | 42 (84%) | 563(93.8%) | ||
| Abnormal | 29 (5.3%) | 8 (16%) | 37 (6.2%) | 9.115 | 0.003 |
| Total | 550(100%) | 50 (100%) | 600(100%) | ||
Table 16. Comparison of Seizures and outcome (N=600).
6.2% of the study population had seizures. Seizures were present in 16% of all deaths. There was a statistically significant correlation between seizure occurrence and outcome (Table 17).
| S.No | Total score | Total No. of children | Outcome | Chi square | P value | |
|---|---|---|---|---|---|---|
| Discharge (n=550) | Death (n=50) | |||||
| 1 | 0 | 323 | 323 | 0 | 429.015 | <0.001 |
| 2 | 1 | 166 | 160 | 6 | ||
| 3 | 2 | 63 | 60 | 3 | ||
| 4 | 3 | 19 | 7 | 12 | ||
| 5 | 4 | 12 | 0 | 12 | ||
| 6 | 5 | 10 | 0 | 10 | ||
| 7 | 6 | 7 | 0 | 7 | ||
Table 17. Comparison of total score and outcome (N=600).
Total score and outcome
When the total TOPRS score was zero, there was no mortality, whereas when the total score ranged from 4 to 6, there was 100% mortality (P value <0.001) (Figure 1 and Table 18).
| Test result variable(s): Total score | ||||
|---|---|---|---|---|
| Area under the curve | Std. Error | P value | 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||
| 0.962 | 0.013 | <0.001 | 0.936 | 0.988 |
Table 18. Predictive validity of total score in predictive mortality.
Data was analyzed bi-variably and multivariably using regression analysis. In the present study the area under the curve was found to be 0.96 i.e. the predictive value of the score was 96.2%.
A score of 2.5 has maximum discrimination with sensitivity of 84% and specificity of 96%. The predictability of severity of illness on admission by the TOPRS score was excellent and was found to be statistically significant (p value <0.001) and uses less time, less resources, less manpower. Harmesh et al. conducted a study entitled “A simple clinical score TOPRS to predict outcome in pediatric emergency department in a teaching hospital in India’s during the year 2011 in Dayanand medical college and hospital, Ludhiana, India.
They found that out of six variable temperature, oxygen saturation, respiratory rate, were found to be significantly associated with mortality whereas in the present study it was found that abnormality in all the six variable was significantly associated with mortality. They also found that mortality increased with increase in number of abnormal variables [5]. In the present study also, similar results were obtained. Predictive value of the score was found to be 81.7 whereas in the present study the predictive value of the score was 96%. In another study conducted by Dr. Arthilatha at Thirunelveli medical college,titled “A simple clinical scoring system TOPRS to predict the outcome and mortality in paediatrics emergency department in TVMCH”, it was found that the performance of the TOPRS score was excellent and the predictive value of the score was 92% which was almost similar to the present study [4]. It was also found that mortality increases with decreasing age which is also similar to the present study.
It was found that the individual variable, pulse rate, respiratory rate, SpO2, and Senorium, each was significantly associated with mortality whereas in present study all the individual variables had a statistical significant association with mortality. In an article published by Salah et al. entitled “Use of vital signs as predictors for serious bacterial infections in children with acute febrile illness in a pediatric emergency setting in Sudan in the year 2014, it was found that tachycardia and tachypnoea were the most sensitive and specific indicator in predicting serious bacterial infections with 80%; 86.6% sensitivity and 97.4%, 83.7% specificity respectively [6].
This present study also substantiates these findings. It was found that temperature and severe hypoxaemia were least sensitive but highly specific signs of serious bacterial infections in pediatric emergency department and has comparable sensitivity to more complicated triage systems. In a study done by Salamati et al. entitled validation of pediatric index of mortality 2 scoring system in a single pediatric intensive care unit in lran, it was found that the area under the ROC curve was 0.795 (0.715-0.875 for 95% confidence interval) and standardized mortality ratio was 1.8 which is less than that obtained in this present study [7].
TOPRS score of 3 was significantly associated with mortality in the previous study done at the institute of child health, Chennai in the year 2006 to validate the usefulness of PRISM III score in predicting the mortality in PICU involving the same age group, the area under ROC was 0.853 i.e., 85% correct in predicting mortality. The TOPRS score has performed better than PRISM score in predicting mortality in this population with area under ROC being 0.96. In conclusion, on admission TOPRS score has performed very well in predicting the outcome of patients with area under the curve of 0.96 i.e., 96% correct prediction of severity.
Hence the utilization of the TOPRS score will help in:
• Mortality prediction.
• Identification of the sick children requiring urgent intervention.
• Counseling of the caretakers of the condition of their child.
• Proper utilization of resources.
Conclusion
• TOPRS score is a simple scoring system using simple clinical variables and does not require expertise to perform.
• This study has shown a definite correlation between the TOPRS score and the poor outcome.
• It has also revealed that, higher the score, longer the ICU stays.
• Among the variables, the temperature and the heart rate abnormality were associated with poorer outcomes in comparison to the other variables.
References
- https://pubmed.ncbi.nlm.nih.gov/23056866/
- Anthony RB, David H, Stephanie B, et al. Assessment and optimization of mortality prediction tools for admissions to pediatric intensive care in the United Kingdom. Pediatrics 2006; 117(4): e733-42.
- https://www.aap.org/en/my-account/login/
- http://repository-tnmgrmu.ac.in/5870/
- Barbara HF, Amber H, Brenda K, et al. Transdisciplinary Obesity Prevention Research Sciences (TOPRS) curriculum increases knowledge about complex causes and consequences of obesity for undergraduate students. Front Public Health 2019; 22(1): 97.
- https://www.semanticscholar.org/paper/The-use-of-vital-signs-as-predictors-for-serious-in-Salah-Ahmed/3a7ea116a64b7fffff675b8ea9623694981217e8
- Salamati P, Talaee S, Eghbalkhah A, et al. Validation of pediatric index of mortality-2 scoring system in a single pediatric intensive care unit in Iran. Iran J Pediatr 2012; 22(4): 481.