Research Article - Biomedical Research (2017) Volume 28, Issue 1
Effect of thoracolumbar posterolateral screw-rod anteroposterior integration fixation
Jianliang Wang#, Feng Guo#, Weifeng Liu, Zhangyong Tan, Xu Lu, Kefeng Xu*Department of Orthopedics, the 101 Hospital of Nanjing Military Area Command of Chinese PLA, Wuxi 214044, Jiangsu Province, PR China
#These authors contributed equally to this work as co-first authors
- *Corresponding Author:
- Kefeng Xu
Department of Orthopedics
The 101 Hospital of Nanjing Military Area Command of Chinese PLA
Jiangsu Province, PR China
Accepted date: June 29, 2016
Abstract
This study aimed to investigate the curative effect of anteroposterior integration fixation with a selfdesigned posterolateral screw-rod on thoracolumbar disease in clinical practice. A total of 12 patients with thoracolumbar disease, who received treatment between December 2009 and May 2010, were retrospectively analyzed. Among the patients, eight were men and four were women. Their ages ranged from 23 to 62 years (average age, 36.4 years). They received pedicle and vertebral internal fixation posterolateral to the vertebral column by using the screw-rod system. Local pain amelioration, kyphotic Cobb angle correction, and neural functional recovery were observed for the evaluation of curative effect. All the patients were followed with an average time of 7.8 months (range, 6-10 months). Local pain ameliorated in all patients, and their kyphoses and neural functions recovered to different degrees. No surgery-related complications occurred. Thoracolumbar posterolateral screw-rod anteroposterior integration fixation might produce a satisfactory curative effect on thoracolumbar disease.
Keywords
Thoracolumbar vertebra, Posterolateral, Screw-rod system, Anteroposterior integration fixation.
Introduction
Thoracolumbar spinal tumor, tuberculosis, and fracture are common diseases in orthopedics. Although these diseases have different causes, their surgical treatments should have the same goals, including nerve decompression, spinal stability recovery, and prevention and correction of kyphotic deformities. Since a posterior approach cannot achieve complete spinal decompression, and because it requires strict skills in vertebral resection and easily causes dural sac and nerve root injury during operation and pedicle nail fracture after vertebral resection, more and more researchers advocate for the use of an anterior approach in the surgical treatment of thoracolumbar tumors, tuberculosis, and fractures [1-5]. However, anterior surgery, regardless of using screw-plate systems or screw-rod systems, has the drawbacks of serious surgical traumas, difficult exposure, difficult operative procedure, unsatisfactory fixation intensity, and numerous complications. Furthermore, exposure needs sufficient experience, which often requires the help of thoracic and general surgeons. Therefore, this approach has the risks of chest and abdominal visceral injuries [6-10].
Sufficient exposure of the vertebral anterior structure with moderate surgical trauma, together with nerve decompression, spinal stability recovery, and kyphotic deformity prevention and correction, has long been a challenge for spine surgeons. In this study, to avoid the drawbacks of the anterior approach and to ensure the reliability of posterior fixation, we designed a thoracolumbar posterolateral Anteroposterior Integration Fixation (APIF) technique based on the characteristics of the anatomic structure and the mechanical weight bearing of the thoracolumbar vertebral bodies. The surgical technique of thoracolumbar posterolateral longitudinal incision is mature, with the advantages of a small surgical incision, moderate trauma, little hemorrhage, and clear exposure of the vertebral anterior and posterior structures on the diseased side. Furthermore, creeping decompression can help expose the structure until the lesion contralateral side, thereby protecting the dural sac and nerve root with an easy operation and avoiding thoracoabdominal injuries. Between December 2009 and May 2010, we successfully treated 12 patients with thoracolumbar disease by using thoracolumbar posterolateral screw-rod APIF.
Subjects and Methods
Subjects
Twelve patients were recruited, including eight men and four women. Their ages ranged from 23 to 62 years (average age, 36.4 years). The inclusion criteria were based on the intraoperative and postoperative pathological diagnoses. Three patients had neglected fractures, two had tuberculosis, two had a tumor, and five had blowout fractures. Moreover, two patients had upper thoracic vertebral disease, three had middle thoracic vertebral disease, five had thoracolumbar disease, and two had lumbar vertebral disease. All patients had lumbodorsal pain to different degrees. Nine patients had accompanying kyphotic deformities. Eight patients had nerve dysfunction with the following Frankel grades: two had grade A, three had grade B, two had grade C, and one had grade D nerve dysfunction. All patients were subjected to anteroposterior and lateral radiography, computed tomography, and magnetic resonance imaging of the diseased vertebra. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of the 101 Hospital of Nanjing Military Area Command of Chinese PLA. Written informed consent was obtained from all participants.
Analysis method
Finite element biomechanical analysis was performed by using the following software programs: Mimics 10.0 (medical finite element modeling), Geomagic 8.0 (reverse engineering), Hypermesh 11.0 (finite element preprocessing), Abaqus 6.9 (large-scale finite element analysis software), and Solidworks 2011/UG7.5. Anterior pedicle screw and unilateral vertebral screw models were established as follows.
The anterior edge of the L1 vertebra was lowered by 90% in height to simulate a fracture. Four different surgical approaches were adopted: (i) bilateral pedicle screw implantation, (ii) unilateral pedicle screw + unilateral vertebral screw implantation, (iii) unilateral vertebral screw implantation, and (iv) unilateral double-vertebral screw implantation. The vertebral and pedicle screws and connective rods were made of titanium alloy (Ti6Al4V) with an elastic modulus of 110 GPa and a Poisson ratio of 0.33 [11,12]. The kyphotic Cobb angle, the angle between the upper endplate of the vertebra above and that of the vertebra below the diseased vertebra, was measured. As computer-assisted measurement of the Cobb angle has a higher precision than that with conventional radiographs [13], we used Mimics 10.01 software for measuring the Cobb angle.
Sampling treatment
All patients received general anesthesia and were placed in the supine position. An approximately 12-15 cm posterolateral longitudinal incision was made, with the diseased vertebra as the center. The diseased vertebra and adjacent vertebrae were exposed routinely, and the segmental vessels were moved aside. An approximately 3 cm long rib was cut off, the transverse process was retained, and the nerve roots were protected. Pedicle screws were implanted into the pedicles of the adjacent vertebrae under direct vision (the implantation was attempted along the upper verge of the pedicle). Lateral vertebral screws were implanted into the vertebra inferolateral to the pedicle in a 10-15° angle with the posterior edge of the vertebra.
The angle between the two screws implanted into the same vertebra was 60-70°. After four screws were implanted, the two pedicle screws were propped open by using a pre bent connective rod. During anterior decompression, the intervertebral disc, the pedicle of the diseased vertebra, and the vertebral posterior edge were excised, and the bone block protruding into the spinal canal and the intervertebral disc tissues were thoroughly removed. After satisfactory decompression was achieved, a structural bone block or titanium mesh was inserted. A lateral vertebral screw connective rod was mounted, and the screws were propped open (alternate propping could be performed until a satisfactory result was achieved). The operating time and hemorrhage volumes were recorded. Pain was evaluated by using the visual analogue scale (VAS) [14] before the operation, at 3 days after the operation, and at the time of the final follow-up. The kyphotic Cobb angle was measured before the operation, at 1 week after the operation, and at the time of the final follow-up. Nerve dysfunction Frankel grading was performed before the operation and at the time of the final follow-up for the assessment of curative effect.
Statistical analysis
Data were analyzed by using SPSS 16.0 software. t-Tests were used to compare measurement data, and χ2 tests were used for enumeration data. Differences of P<0.05 were considered statistically significant.
Results
Clinical data
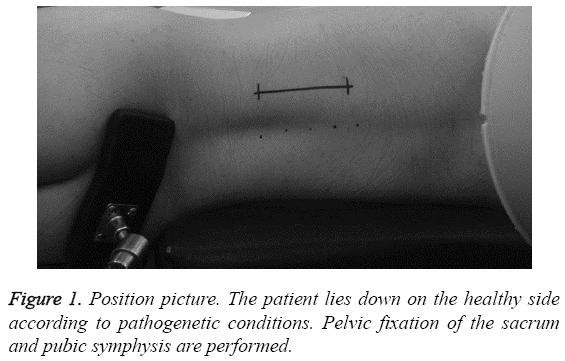
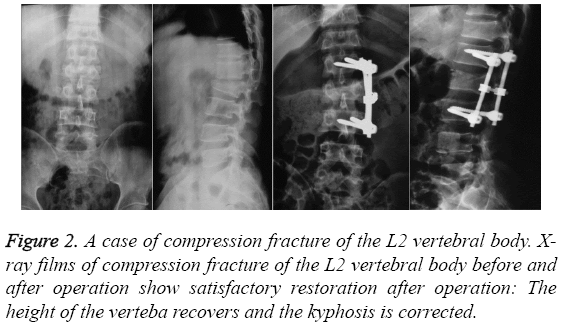
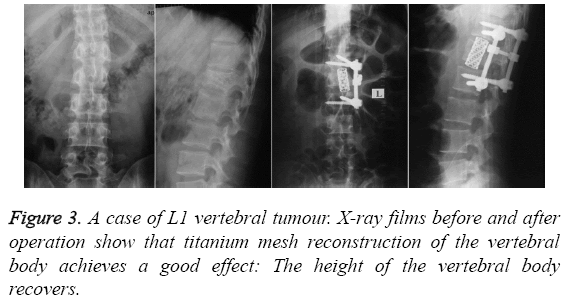
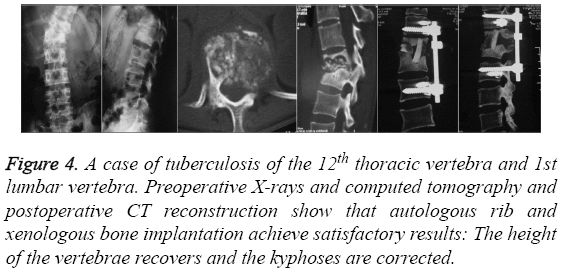
All patients were followed for 4-10 months, with an average follow-up time of 6.8 months. Surgery was smoothly accomplished for all patients in a lateral position, and pelvic fixation was then performed (Figure 1). The operating time ranged from 60 to 120 min, with an average of 90 min. The hemorrhage volumes were between 400 and 1100 mL, with an average of 600 mL. During and after the operation, no anesthesia-related complications occurred. No pressure sores occurred at the location of fixation. One patient developed hydrothorax, which disappeared after thoracentesis and drainage. No postoperative infection occurred. During the follow-ups, no fixator fracture or loosening was observed. The results of the image examinations for some typical cases are shown in Figures 2-4.
Figure 4: A case of tuberculosis of the 12th thoracic vertebra and 1st lumbar vertebra. Preoperative X-rays and computed tomography and postoperative CT reconstruction show that autologous rib and xenologous bone implantation achieve satisfactory results: The height of the vertebrae recovers and the kyphoses are corrected.
Detected VAS scores
After the operation, pain was relieved to different degrees in all patients. The VAS scores 3 days after the operation and at the time of the final follow-up noticeably improved compared with that before the operation (P<0.01), whereas no significant difference was observed between the scores at 3 days after the operation and at the time of the final follow-up (P>0.05). The results are summarized in Table 1.
| 24 h before operation | 3 d after operation | Final follow-up | |
|---|---|---|---|
| VAS | 7.8±0.9 | 3.8±1.0* | 2.5±0.9*# |
Table 1: Visual analogue scores (VAS) 24 h before operation and 3 d and the final follow-up after operation.
Comparison of the kyphotic Cobb angles before and after the operation
Postoperative radiography showed that the kyphotic Cobb angles were corrected to different degrees in the nine patients with kyphotic angulation deformities. Before the operation, their average Cobb angle was 15.9 ± 3.6°. At 1 week after the operation, the value decreased to 0.9 ± 2.9°. At the time of the final follow-up, this value was 1.1 ± 3.1°. The kyphotic Cobb angle significantly improved at 1 week after the operation and at the time of the final follow-up compared with that before the operation (P<0.01), whereas no significant difference was observed between the angles at 1 week after the operation and at the time of the final follow-up (P>0.05). The results are summarized in Table 2.
| Preoperative | 1 w after operation | Final follow-up | |
|---|---|---|---|
| Cobb angle | 15.9±3.6º | 0.9±2.9º* | 1.1±3.1º*# |
Table 2: Kyphotic Cobb angles before operation, 1 w after operation, and during the final follow-up.
Neural function-based Frankel grades
Among the eight patients with different degrees of neural dysfunction, seven were observed to have improved by no less than one grade, with the exception of one patient with a blowout fracture who showed no improvement after a complete paraplegia. According to the Frankel grading at the time of the final follow-up after the operation, one patient was grade A, one was grade B, one was grade C, three were grade D, and two were grade E (Table 3). The patients were divided into the intact, bilateral pedicle screw, unilateral pedicle screw + lateral screw, lateral screw, and unilateral bilateral-approach screw groups based on the four basic operating conditions. In each group, parameters including extension, flexion, left bending, right bending, left torsion, and right torsion were calculated, resulting in a total of 30 groups of operating condition data.
| Preoperative Frankel | Case number | Final follow-up Frankel grade | ||||
|---|---|---|---|---|---|---|
| Grade | A | B | C | D | E | |
| A | 2 | 1 | 1 | |||
| B | 3 | 1 | 2 | |||
| C | 2 | 1 | 1 | |||
| D | 1 | 1 | ||||
| E | 4 | 4 | ||||
Table 3: Neural function-based Frankel grades of the 12 patients before operation and at the time of the final follow-up.
Activity evaluation
All the screw-rod systems significantly enhanced the stability of the operated segment and decreased the activity of the spinal system. Bilateral pedicle fixation and unilateral pedicle screw + lateral vertebral screw fixation both achieved good stability after the operation. Bilateral pedicle fixation showed the best stability in resistance to anteflexion and extension among all the techniques. Unilateral pedicle screw + lateral vertebral screw fixation had better performance in terms of resistance to side flexion and torsion. Noticeably, pedicle screw + lateral vertebral screw fixation had a slightly worse effect on the resistance to bending toward the opposite side than did bilateral pedicle fixation. Unilateral vertebral screw fixation showed poor stability.
Maximum stress on the endplate and on the intervertebral disc
Concerning the maximum stress on the endplate, under the same activity, all three surgeries reduced the maximum stress on the endplate to some degree. Unilateral bone screw fixation showed poorer stability than did any other operation and the stress on the endplate was closer to that in an injury-free model. Concerning the maximum stress on the intervertebral disc and implant, after bilateral pedicle screw fixation, the load on the implant was well distributed. This method achieved the least maximum stress on the implant, followed by unilateral pedicle screw + lateral bone screw fixation (achieving a maximum stress very close to bilateral pedicle screw fixation). Unilateral bone screw fixation caused the greatest stress on the implant. Considering that the maximum stress on the implant after any of the above-mentioned technique was far smaller than the yield stress of the titanium alloy Ti6Al4V (about 840 MPa), any of the three techniques had a rather satisfactory instant safety coefficient after the operation.
Discussion
A thoracolumbar screw-rod APIF technique was designed through a posterolateral incision based on the anatomic characteristics of the thoracolumbar vertebrae. This posterior approach avoided the drawbacks of the anterior approach, such as serious traumas, exposure difficulty, requirement for exposure experience, increased risks of thoracic and abdominal organ injuries, difficult surgical operation, poor fixation intensity, and numerous complications. The approach of thoracolumbar posterolateral longitudinal incision has significant advantages. First, thoracolumbar posterolateral longitudinal incision is a mature technique. As only a small number of tissues are involved, this method leads to minor trauma and small hemorrhage volume, with an easy operation. Second, compared with the large screw insertion angle in the conventional lateral anterior double screw and rod fixation, in this technique, the screw insertion directions both had a forward deviation, and the screw insertion sites were more posterior. These changes enabled easier screw insertion and made excessive dragging unnecessary, which helped avoid nerve and vessel injuries. Third, in this technique, the two pedicle screws were first propped open and fixed by using a pre bent connective rod, and then vertebral decompression and lesion removal were performed.
This treatment did not only guarantee safety and reliability but also facilitated the installation of a bone graft, a titanium mesh, or a fusion device such as a cage. Fourth, it facilitated the corrections of scoliotic and kyphotic deformities because the two groups of screws and rods were inserted into the lateral and posterior sides of the diseased vertebra, respectively. Fifth, the finite element biomechanical analysis showed that the thoracolumbar posterolateral screw-rod APIF designed in this study achieved a fixation as intense as that of bilateral pedicle screw fixation, stability in resistance to anteflexion and extension close to that of bilateral pedicle screw fixation, and satisfactory postoperative instant stability. Moreover, it showed better performance in terms of resistance to side bending and torsion than did bilateral pedicle screw fixation. In contrast, the unilateral vertebral screw technique showed poor stability. Furthermore, creeping decompression can help expose the structure until the lesion contralateral side, thereby protecting the dural sac and nerve root with an easy operation and avoiding thoracic and abdominal injury.
The method used in this study solved the difficult problems of the anterior approach. A group of vertebral screws were implanted externally posteroinferior to the thoracolumbar vertebra, which is a new concept in itself in three-dimensional cross-screw fixation. Meanwhile, this method gave consideration to the anterior and posterior approaches and APIF. Furthermore, anteroposterior and lateral integral corrections could be made during the installation of the fixation rod and the transverse connection. The new technique of thoracolumbar posterolateral screw-rod fixation based on empirical studies overcomes the limitations of the anterior or posterior approach alone and is a reliable method for anteroposterior correction and fixation at the same time. The thoracolumbar anterior approach has a comparatively high risk of trauma and complications, and its procedure is more complex than that of the posterior approach [15-17]. The designed thoracolumbar posterolateral screw-rod APIF technique in this study reduced the difficulty of thoracolumbar anterior decompression. It successfully realized the integration fixation with pedicle and vertebral screws through the same posterolateral incision, and thus presents noticeable advantages.
Some precautions should be taken during thoracolumbar posterolateral screw-rod APIF. First, posterior pedicle screw insertion is easily performed under direct vision. It is not feasible to insert the screws into the spinal canal, which will injure the spinal cord and nerve roots. Pedicle screws should be inserted close to the upper edge of the pedicle as much as possible, to allow enough space for lateral vertebral screw insertion. The vertebral screws should be inserted laterally into the vertebra inferior to the pedicle. The screws should be in an angle of 10–15° with the posterior edge of the vertebra, and the included angle between the screws in the same vertebra should be kept at 60-70°. Second, after the insertion of four screws, the posterior two pedicle screws should be first propped open by using a prebent connective rod, and then a vertebral lateral screw connective rod should be mounted to prop open the rest of the screws; that is, sagittal correction should be made first, followed by lateral correction. During the operation, the prebending and propping of the connective rods should be adjusted to satisfactory degrees by using C-arm radiography. If decompression is needed, decompression and fusion should be performed from the diseased pedicle to the vertebra. Then, the intervertebral disc after the posterior two pedicle screws are connected and fixed, which will greatly benefit the operation. Third, the nerve roots and their recurrent branches should be pulled aside and protected rather than being cut off during screw insertion and decompression.
Although the approach used in this study does not involve thoracoabdominal organs and important vessels like the anterior approach, possible intraoperative and postoperative complications should be prevented [18-21]. Pleura injury should be avoided during rib resection in case of hemopneumothorax, atelectasis, and pulmonary infection. The angle of the inserted vertebral screws should be strictly secured, and an excessive angle may pose the risks of penetrating the vertebra and damaging the great vessels (thoracic and abdominal aortas and vena cavae). For patients with osteoporosis, the reliability of the internal fixator should be given due attention and its indications should be strictly followed. The indications of thoracolumbar posterolateral screw-rod APIF include thoracolumbar vertebral tumors, spinal tuberculosis, blowout fracture where the fractured bone intrudes into more than one-half of the spinal canal (i.e., posterior longitudinal ligament rupture), spinal anterior compression caused by thoracolumbar old compression fracture, dorsal disc prolapse in the segment above L1/2, and scoliosis. Thoracolumbar posterolateral screw-rod anteroposterior integration fixation has the potential to be an effective treatment for thoracolumbar diseases.
Conclusion
Thoracolumbar posterolateral screw-rod APIF is usually used in infants. Our results proved that this technique might be a simple, convenient, and high-performance new approach in adults as well.
Limitations
One of the limitations of this study is the insufficient number of patients. The second limitation is the lack of the quality data evaluating the effects of thoracolumbar posterolateral screwrod APIF. Finally, the third limitation is the short follow-up time.
References
- Aligizakis AC, Katonis PG, Sapkas G, Papagelopoulos PJ, Galanakis I, Hadjipavlou A. Gertzbein and load sharing classifications for unstable thoracolumbar fractures. ClinOrthopRelat Res 2003; 411: 77-85.
- Alvine GF, Swain JM, Asher MA, Burton DC. Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis: case series and literature review. J Spinal Disord Tech 2004; 17: 251-264.
- Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D, Study Group on Scoliosis. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976) 2012; 37: 693-700.
- Zhong W, Xiong G, Wang B, Lu C, Dai Z, Lv G. Surgical management for thoracic spinal tuberculosis posterior only versus anterior video-assisted thoracoscopic surgery. PLoS One 2015; 3: e0119759.
- Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine 2009; 34: E729-E734.
- Yong MR, Izatt MT, Adam CJ, Labrom RD, Askin GN. Secondary curve behavior in Lenke type 1C adolescent idiopathic scoliosis after thoracoscopic selective anterior thoracic fusion. Spine (Phila Pa 1976) 2012; 23: 1965-1974.
- Etchepare F, Rozenberg S, Mirault T, Bonnet AM, Lecorre C, Agid Y, Bourgeois P, Fautrel B. Back problems in Parkinson's disease: an underestimated problem. Joint Bone Spine 2006; 73: 298-302.
- Konstantinidis L, Mayer E, Strohm PC, Hirschmüller A, Südkamp NP, Helwig P. Early surgery-related complications after anteroposterior stabilization of vertebral body fractures in the thoracolumbar region. J OrthopSci 2010; 15: 178-184.
- Leduc S, Mac-Thiong JM, Maurais G, Jodoin A. Posterior pedicle screw fixation with supplemental laminar hook fixation for the treatment of thoracolumbar burst fractures. Can J Surg 2008; 51: 35-40.
- Nam TK, Park SW, Shim HJ, Hwang SN. Endovascular treatment for common iliac artery injury complicating lumbar disc surgery: limited usefulness of temporary balloon occlusion. J Korean NeurosurgSoc 2009; 46: 261-264.
- Qiu Y, Wang S, Wang B, Yu Y, Zhu F, Zhu Z. Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one chinese institution. Spine 2008; 33: 519-526.
- Schmidt H, Heuer F, Drumm J, Klezl Z, Claes L, Wilke HJ. Application of a calibration method provides more realistic results for a finite element model of a lumbar spinal segment. ClinBiomech (Bristol, Avon) 2007; 22: 377-384.
- Schmidt H, Kettler A, Heuer F, Simon U, Claes L, Wilke HJ. Intradiscal pressure, shear strain, and fiber strain in the intervertebral disc under combined loading. Spine (Phila Pa 1976) 2007; 32: 748-755.
- Tezeren G, Gumus C, Bulut O, Tukenmez M, Oztemur Z, Sever G. Anterior versus modified combined instrumentation for burst fractures of the thoracolumbar spine: a biomechanical study in calves. J OrthopSurg (Hong Kong) 2008; 16: 281-284.
- Lee M, Song C, Jo Y, Ha D, Han D. The effects of core muscle release technique on lumbar spine deformation and low back pain. J PhysTherSci 2015; 27: 1519-1522.
- Lee MG, Hwang JS, Seo BD, Im G, Jeon N, Yang H, Kim T, Kim H, Han D. The effects of the core muscle release technique on scoliosis. J PhysTherSci 2013; 25: 445-448.
- Kim ER. Effect of Vibration Frequency on Serratus Anterior Muscle Activity during Performance of the Push-up Plus with a Redcord Sling. J PhysTherSci 2014; 26: 1275-1276.
- Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, Oner FC. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976) 2004; 29: 803-814.
- Wang Y, Fei Q, Qiu G, Lee CI, Shen J, Zhang J, Zhao H, Zhao Y, Wang H, Yuan S. Anterior spinal fusion versus posterior spinal fusion for moderate lumbar/thoracolumbar adolescent idiopathic scoliosis: a prospective study. Spine (Phila Pa 1976) 2008; 33: 2166-2172.
- Wills BP, Auerbach JD, Zhu X, Caird MS, Horn BD, Flynn JM, Drummond DS, Dormans JP, Ecker ML. Comparison of Cobb angle measurement of scoliosis radiographs with preselected end vertebrae: traditional versus digital acquisition. Spine (Phila Pa 1976) 2007; 32: 98-105.
- Abudou M, Chen X. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database of Systematic Reviews 2013; 6: 957-969.