Research Article - Journal of Public Health Policy and Planning (2023) Volume 7, Issue 3
Effect of an integrated neuromuscular exercise program on chronic Achilles tendinopathy in middle-aged women
Shivanjali S. Kadam, Rutuja Arulekar, Sandeep B. Shinde*
Department of Physiotherapy, Intern, Krishna Institute of Medical Sciences, Karad, India.
- *Corresponding Author:
- Sandeep B. Shinde
Department of Physiotherapy, Intern
Krishna Institute of Medical Sciences, Karad, India
E-mail: drssndeepshinde24@gmail.com
Received: 16-Feb-2023, Manuscript No. AAPHPP-23-89384; Editor assigned: 21-Feb-2023, PreQC No. AAPHPP-23-89384 (PQ); Reviewed: 02-Mar-2023, QC No. AAPHPP-23-89384; Revised: 25-Apr-2023, Manuscript No. AAPHPP-23-89384 (R); Published: 02-May-2023, DOI: 10.35841/aaphpp-7.3.172
Citation: Shinde SB. Effect of an integrated neuromuscular exercise program on chronic Achilles tendinopathy in middle-aged women. J Public Health Policy Plan. 2023;7(3):172.
Keywords
Achilles tendinopathy, Neuromuscular exercise, Neural tissue mobilization, Eccentric exercises, pain, Muscle length.
Introduction
The term tendinopathy is different from the term tendinitis and tendinosis. Tendinosis implies tendon degeneration without clinical or histological signs of intra-tendinous inflammation whereas Tendinitis is a clinical syndrome with inflammatory features [1]. Thus, Achilles Tendinopathy is a tendon disorder characterized by a combination of pain, swelling (diffuse or localized), and impaired performance of the Achilles tendon with histopathological entities [2]. The Achilles tendon is the most commonly affected tendon seen in athletes as well as in the general population.
The Achilles tendon is the thickest tendon of the body located at the back of the lower leg [3-5]. It connects the gastrocnemius and soleus muscles, together called calf muscles, to the calcaneal tuberosity of the calcaneus (heel bone) hence, also called as calcaneal tendon. In walking, the soleus muscle overcomes the inertia of the body and when the movement is underway, the fast-acting gastrocnemius increases the speed. The soleus is more powerful than the gastrocnemius and is the postural muscle that helps to steady the leg over the foot [6]. The Achilles tendon gets its sensory nerve supply from the nerves of the attaching muscles particularly the sural nerve, and posterior tibial nerve [7]. Tendon functions in transmitting the force to the bone generated by the muscles and absorbing the force to limit muscle damage [8].
Tendon injuries are classified into acute, where extrinsic factors predominate, and chronic, where extrinsic, as well as intrinsic factors, are responsible equally. Some of the intrinsic factors are tendon vascularity, Gastro-soleus dysfunction, age, gender, body weight, height, etc. lateral heel strike with compensatory pronation also contributes to Achilles Tendinopathy. Previous injuries and types of footwear also predispose to Achilles Tendinopathy [9]. Articles shows Increased BMI puts stress on the Achilles tendon resulting in pain additionally, forefoot varus is commonly seen in patients with Achilles Tendinopathy [10].
Achilles tendinopathy is an overuse injury as the Achilles tendon is the most commonly used tendon during daily activities [11, 12]. Women in their middle-age face a lot of hormonal imbalances, decreased bone density, and loss of flexibility resulting in muscle pain and stiffness. The middleage is the age at which symptoms of the perimenopause period start to occur so there is a decrease in the levels of estrogen, progesterone, and testosterone levels in the women’s body [13]. Also, there are changes in the growth hormones and thyroid hormones as age increases. All these hormones have a particular role in the composition of tendon collagen, maturation of tendons, and maintaining the strength and thickness of the tendon [14].
Women start losing bone density as the age increases due to decreasing calcium levels in the body which gives rise to muscle cramps and pain resulting in increased perimenopausal symptoms [15]. The physical activity of women is related to age. With the increasing age, women become less active physically and this may be due to decreased muscle strength, flexibility, and other changes that start occurring in the body [16].
Despite some of the causative factors of tendinopathy, many women face a typical type of Achilles tendon pain after their third decade. As the tendon connects the muscles to the bone and both muscles and tendon work together, any discomfort in the tendon results in discomfort in the muscle to which it connects. So, Achilles tendon pain will affect the calf muscles too.
Women with Achilles tendon pain tend to change their pattern of gait by decreasing the normal range of ankle dorsiflexion while walking to compensate for the pain. This results in a reduced range of ankle dorsiflexion as the condition worsens, increasing the risk of fall as the centre of gravity gets shifted forward. The reduced range of ankle dorsiflexion may develop weakness of the tibialis anterior muscle which is the ankle dorsiflexor resulting in a condition called tibialis muscular dystrophy.
Women who are less active physically develop calf muscle dysfunction and are more prone to Achilles tendinopathy. The loss of flexibility of the calf muscle can pull the Achilles tendon which puts stress on the tendon leading to strain which further contributes to Achilles tendinopathy and other issues of the calf muscle.
Neural tissue mobilization is a technique that aims at mobilizing the nerve by increasing the blood circulation in and around the nervous system [17, 18]. Neural mobilization facilitates movement between neural and surrounding structures by reducing the force [19]. There is no doubt that the nerves in the body also glide during any kind of movement. The tightness of the gastrocnemius may put pressure on the underlying nerves and might have difficulty in gliding and have other effects as both the branches of the sural nerve pierce the medial head of the gastrocnemius muscle above the knee [20]. The tightness produced is like constant contraction of the calf muscles creating discomfort while doing any activities.
The human body is interconnected; any kind of discomfort in one joint or muscle affects the proximal and/ or distal joint. Thus, Achilles tendinopathy has contributed to the knee, foot, and hip problems. The pain in the Achilles tendon and calf muscles further starts worsening with time if left untreated.
Gradually this can cause problems in the knee and ankle as the Achilles tendon and calf muscle especially gastrocnemius as it is two-joint muscles that are in contact with both the joints. Women might feel difficulty in straightening their legs while walking due to tightness and pain which contributes to other issues of quadriceps and hamstrings. This further can restrict the movements in the hips (reduced hip extension) resulting in decreased walking stride.
Also, the calf tightness can lead to tightness of the Achilles tendon which may put stress on the hips and contribute to increased hip angle resulting in low back pain and creating issues in the pelvis. An individual with Achilles tendinopathy has referred pain in the sole as well as the knee. The alignment of the ankle is important as well. If the foot is over pronated, the pain in the Achilles tendon and foot gets aggravated.
Many researchers focus only on relieving the symptoms and strengthening the Achilles tendon in Achilles tendinopathy. But the condition of the underlying nerves also has to be addressed because any condition that is causing stress or other problems to the muscle and tendon affects the nerve too. A lot of women keep neglecting their health issues and nowadays, we also find women in every sector of work, so women must be healthy. Thus, this study is intended to focus on finding the effectiveness of an integrated neuromuscular exercise protocol in women of middle age.
Materials and Methods
This was an experimental study carried out in Karad, Satara district. Total of 150 females between the age group of 30 to 44 years were selected with random allocation method. All the 150 participants selected fulfilled the inclusion criteria of being women with mild Achilles tendinopathy and BMI greater than 25kg/m2 with no history of osteoarthritis of the hip, knee, and ankle along with no history of diabetes mellitus, peripheral neuropathy, and trauma to the lower limb, foot conditions, peripheral arterial disease, deep vein thrombosis, and implants of the hip, knee, and ankle.
Procedure
After getting approval from the ethical committee, the study was carried out in Karad. Participants were selected according to the inclusion and exclusion criteria and were given information about the study procedure, interventions and its benefits. They were given an informed consent form before initiation of the treatment.
Subjects’ demographic information like name, age, body mass index, and lifestyle was documented before initiating the treatment. Assessment of participants were done to check if any injury to the achilles tendon, pain and mobility.
The Thompson test will be performed on all the subjects to confirm that the Achilles tendon is not injured. In this test, the subject will be prone with foot over the end of the table. Alternatively, the subject could lie prone with his knee flexed to 90°.
The examiner will squeeze the calf muscles, specifically the gastrocnemius - soleus complex, with his hand. Squeezing the calf should cause contraction of the Achilles tendon, resulting in plantar flexion. This confirms that the achilles tendon is not injured.
The assessment of pain will be taken with the help of a visual analog scale. The subject will be asked to mark a point based on the amount of pain they feel from 0 to 10 on a line measuring 10cm where 0 indicates no pain and 10 indicates severe, intolerable pain. A higher score indicates greater pain intensity.
The length of the calf muscles in a weight-bearing position was taken with the help of a goniometer. The subject was taken in standing position, with the knee extended and the foot in 0 degrees of inversion and eversion. While maintaining the knee in full extension, the heel should remain in full contact with the floor. The subject was asked to dorsiflex the ankle by leaning forward. The end of testing motion was considered when the subject felt tension in the posterior calf and knee. The fulcrum of a goniometer was placed on the lateral aspect of the lateral malleolus; a fixed arm on the lateral midline of the fibula using the head of the fibula for reference and the moving arm was parallel to the lateral aspect of the fifth metatarsal. An angle less than 20 degrees was indicative of shortened length of the calf muscle.
The next assessment will be of the severity of the Achilles tendinopathy which will be based on an index to measure the severity of the Achilles tendinopathy. In this measure, the subject will be asked some questions regarding their Achilles tendon pain and activity and to mark a point from 0 to 10 that they feel suitable about their pain. A score greater than 35 out of 50 will be considered mild. The higher the score, the lesser will be the severity of tendinopathy. The questions will be as follows:
1. For how many minutes do you have stiffness in the Achilles region on first getting up?
2. Once you are warmed up for the day, do you have pain when stretching the Achilles tendon fully over the edge of a step? (Keeping the knee straight)
3. After walking on flat ground for 30 minutes, do you have pain within the next 2 hours? (If unable to walk on flat ground for 30 minutes because of pain, the score will be 0 for this question).
4. Do you have pain walking downstairs with a normal gait cycle?
5. Do you have pain during or immediately after doing 10 (single leg) heel raises from a flat surface?
After this, the subjects’ walking distance will be measured. The subjects will be asked to walk for some distance and a note will be made if she feels pain during or after walking. Then the subjects will be divided into groups A and B where group A will be given an integrated neuromuscular program and Group B will follow a conventional exercise program. After completion of the treatment program, a post-assessment of pain, muscle length, severity of the condition, and distance of walking was remeasured.
Intervention
In this integrated neuromuscular exercise program [21].
Group A
Day 1-4
1. Rest
2. Hot moist pack for 5mins followed by a simultaneous hot pack and stretching of calf muscles with a towel then an ice pack for 5mins.
3. Ankle toe movements 2 sets of 10 reps
4. Heel slides
Day 5- 7
1. Stretching of the calf muscles for 15sec of 3 reps,
2. Bilateral heel raises on the ground (neutral, heel in, heel out)
3. Step up and step down 2 sets of 10 reps was done.
4. Neural tissue mobilization of the tibial nerve, sural nerve, and common peroneal nerve 10 reps of 2 sets
5. Toe and heel walking.
Day 8 to 11
1. Unilateral heel raises 10 reps of 2 sets
2. Pelvic bridging 2 sets of 10 reps
3. Single leg pelvic bridging with 15 degrees of raise 2 sets of 5 reps
4. Seated heel raises with 1/2kg weights on the thigh (10*2)
Day 12 to 16
1. Going upstairs and downstairs (2 flights) were done from
2. Single-leg pelvic bridging (30-45degrees raise) (5*3)
3. Seated heel raises with 1kg weight on the thigh (10*2)
4. Going upstairs and downstairs by carrying ½ kg weights (2 flights)
5. Light jogging (1 min)
Day 17 to 22
1. Start Walking (10 mins) performed from
2. Single-leg pelvic bridging (30-45degrees raise) (15*3)
3. Seated heel raises with 1kg weight on the thigh (15*3),
4. Going upstairs and downstairs by carrying ½ kg weights (3 flights),
5. Light jogging (2 mins)
Day 23 to 28
1. Walking (15 mins) was done from
2. Stretching was done regularly throughout the treatment.
Group B
1. Stretching of calf muscles 15 sec 3 sets
2. Strengthening of calf muscles–bilateral heel raise 10 reps 2 sets
3. Unilateral heel raise 10 reps 2 sets.
Results
All the Statistical analysis was done using paired t-test. A p-value for all the measures was <0.0001 which is considered extremely significant.
Table 1 shows there were 43.3% of subjects from the age group 35-39 which is the highest followed by 37.3% from 40-44 and 19.3% from the age group 30-34. 62.6% of women were found to be overweight and 37.3% of women were obese. The percentage of inactive and active women was 50.6% and 49.3% respectively.
| Age (30-44) | Frequency | Percentage (%) |
|---|---|---|
| 30-34 | 29 | 19.3% |
| 35-39 | 65 | 43.3% |
| 40-44 | 56 | 37.3% |
| BMI (kg/m2) | Frequency | Percentage (%) |
| 25.9-30 (overweight) | 94 | 62.6% |
| 30-40 (obese) | 56 | 37.3% |
| Lifestyle | Frequency | Percentage (%) |
| Active | 74 | 49.3% |
| Inactive | 76 | 50.6% |
Table 1. Demographic Variables
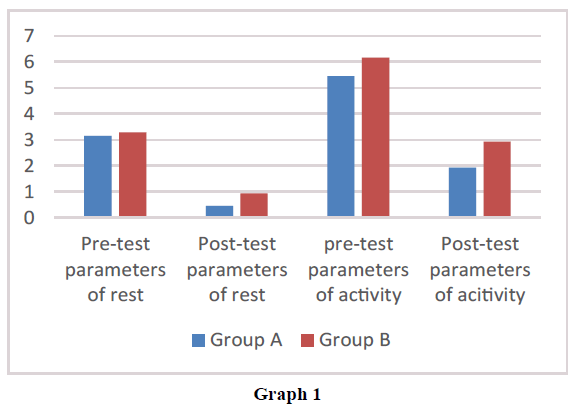
Interpretation: The above Table 2 and Graph 1 showed a decrease in the intensity of the pain of group A in comparison with group B. Group A had a mean of 3.0150± 0.7175 at rest which was then reduced to 0.450± 0.567 while Group B had a mean of 3.285± 0.683 pre-tests which got reduced to 0.945± 0.566 post-tests. The mean of group A on activity was 5.449± 1.88 and group B was 6.164± 0.859 which was decreased to 1.927± 0.650 for group A and 2.933± 0.486 for group B. The paired t-test had a value of 32.771 at rest and 34.563 on activity for group A and 32.609 at rest and 42.734 on activity for group B with a p-value of <0.0001 for both the groups at rest and on activity which is extremely significant.
| Pre-parameters / Post-parameters of group A | Mean | Standard Deviation | p-value | Result | t-value |
| At rest | 3.150/0.450 | 0.7185/ 0.5677 | <0.0001 | Extremely significant | 32.771 |
| On activity | 5.449/ 1.927 | 1.188/ 0.6504 | <0.0001 | Extremely significant | 34.563 |
| Pre-parameters/ post-parameters of Group B | Mean | Standard Deviation | p-value | Result | t-value |
| At rest | 3.285/ 0.945 | 0.6831/ 0.5660 | <0.0001 | Extremely significant | 32.609 |
| On activity | 6.164/ 2.933 | 0.854/ 0.486 | <0.0001 | Extremely significant | 42.734 |
Table 2. Pain Assessment
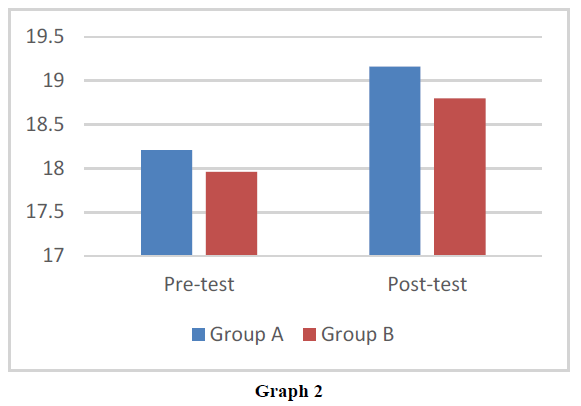
Interpretation: As shown in the above Graph 2 and Table 3, we can interpret that the length of the calf muscle is improved in group A as compared to group B with a mean of 18.21± 1.398 to 19.16± 1.166 and 17.96± 1.350 to 18.8± 1.294 respectively. The p-value is <0.0001 which is extremely significant and the value of paired t-tests is 11.500 and 11.809 for group A and group B respectively.
| Pre-parameters/ post-parameters of group A | Mean | Standard Deviation | p-value | Result | t-value |
| 18.21/ 19.16 | 1.398/ 1.166 | <0.0001 | Extremely significant | 11.500 | |
| Pre-parameter/ post-parameter of Group B | Mean | Standard Deviation | p-value | Result | t-value |
| 17.96/18.8 | 1.350/ 1.294 | <0.0001 | Extremely Significant | 11.809 |
Table 3. Calf Muscle Length
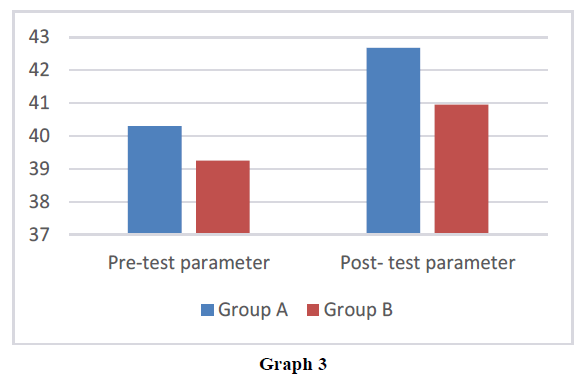
Interpretation: From the above Table 4 and Graph 3, we can state that subjects of group A have an improvement in the severity of Achilles tendinopathy in comparison with group B with the mean from 40.306± 3.866 to 42.68± 3.666 while the mean of group B changed from 39.266± 2.356 to 40.906 ± 2.579. The p-value and value of paired t-test are <0.0001 and 17.210 and 12.387 in both the groups respectively which are considered extremely significant.
| Questions | Mean | Standard Deviation | p-value | Result | t-value |
|---|---|---|---|---|---|
| Pre-parameters/ post-parameters of group A | 40.306/ 42.68 | 3.866/ 3.666 | <0.0001 | Extremely Significant | 17.210 |
| Pre-parameters/ post-parameters of Group B | 39.266/ 40.906 | 2.356/ 2.579 | <0.0001 | Extremely significant | 12.387 |
Table 4. Achilles Tendinopathy Questions
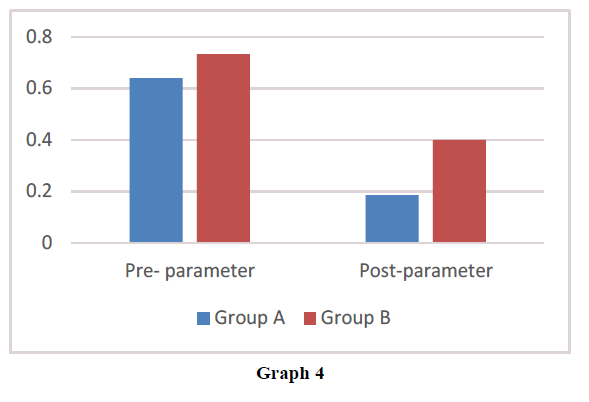
Interpretation: From the above Graph 4 and Table 5, we can interpret that walking distance without pain has significantly increased in group A as compared to group B with a mean of 0.64± 0.483 to 0.186± 0.392 in comparison with the mean of 0.733± 0.445 to 0.4± 0.493. The p-value is 0.0001 which is extremely significant and paired test shows a value of t= 7.384 and t=6.083 for groups A and B respectively.
| Walking distance | Mean | Standard Deviation | p-value | Result | t-value |
|---|---|---|---|---|---|
| Pre-parameters/ post- parameters of group A | 0.64/ 0.1866 | 0.4832/ 0.3923 | <0.0001 | Extremely Significant | 7.384 |
| Pre-parameters/ post-parameters of Group B | 0.733/ 0.4 | 0.4452/ 0.4932 | <0.0001 | Extremely Significant | 6.083 |
Table 5. Walking Distance
Discussion
Achilles tendinopathy is an overuse injury that is caused by overuse of the Achilles tendon. A combination of pathological changes like pain, swelling, and impaired performance of Achilles tendon is seen in Achilles tendinopathy. After a certain period of age, various factors contribute in women to cause the condition that later on can affect their quality of performance. Therefore, it was necessary to have a light on the Achilles tendon in the middle-age women.
This study aimed to find out the effect of an integrated neuromuscular exercise program on chronic Achilles tendinopathy in middle-aged women and to compare the efficiency of an integrated neuromuscular exercise program and conventional exercise program on chronic Achilles tendinopathy.
Achilles tendinopathy has an impact on the quality of life of an individual. ML Ceravolo, JE Gaida, and RJ Keegan conducted research on experiences and quality of life in adults with Achilles tendinopathy where participants with Achilles tendon pain were eligible for the study. In this study, they concluded that Quality of life scores of pains, mental health, senses, and the physical super dimensions was significantly lower in Achilles tendinopathy. They were adapted to the lifestyles, living with the condition. Also, changes in their mental and social well-being, conflict with their identity frustration, and individual experiences were included [22].
Various studies suggested that eccentric calf muscle training has good clinical results in managing symptoms of chronic Achilles tendinopathy [23]. A study done by R Beyer, and M Kongsgaard showed that both the heavy slow resistance and eccentric training were effective for 12 weeks but not after 52 weeks [24]. F Mayer, A Hirschmüller, S Müller did research in which results showed that they experienced a reduction in pain to more than half after 4 weeks of treatment [25]. H Yoshida, N Sato, T Maeda, K Hara in their study on Simultaneous execution of hot pack and muscle stretching enables stronger muscle stretching due to the reduction of stretch pain suggested that simultaneous application of hot pack and muscle stretching will allow stronger muscle stretch by activating spinal gating mechanism [26]. Also, stretching exercises for calf muscles has shown improvement in the pain and flexibility of the muscles. It takes about weeks to months for the Achilles tendon to recover [27].
The Achilles tendon does not have a synovial sheath instead it has a connective tissue that surrounds the tendon called paratenon. Nowadays, the injuries to the Achilles tendon are increasing due to increased or decreased physical activity with age. A study was done by N Gheidi, TW Kernozek, JD Willson, and A Revak where they concluded that bilateral and standing exercises helped in the recovery process of Achilles tendon injury [23]. Another study made a conclusion that the number of repetitions performed has an impact on muscle activation due to ground reaction forces [28].
Neural tissue mobilization is a manipulative treatment that involves stretching or moving the neural tissues with the help of movement. Neural mobilization helps in the reduction in pain and symptoms thus, improving the quality of life of an individual. It also helps in increasing the flexibility of the muscles. A study was done by Romero-Morales C, Calvo Lobo C, Rodriguez Sanz D, Lopez-Lopez D, San Antolin M, Mazoteras Pardo V, Martinez Jimenez EM, Losa Iglesias M, Becerro-de- Bengoa-Vallejos where they stated that neural tissue mobilization is effective in the treatment of pain in various regions and other lower limb musculoskeletal disorders [29].
Wyndow N, Cowan SM underwent a study on neuromotor control of lower limb in Achilles tendinopathy where they concluded that there may be altered neuromotor control of triceps surae in Achilles tendinopathy. Another study was done by MA Matocha and RT Baker on the effects of neuro mobilization on tendinopathy: Part I and II stated that neuro mobilization may be an effective intervention in treating tendinopathies and may have effective changes when the proper classification of tendinopathy is done.
From all the mentioned studies, we can say that there can be possibility of neural involvement in the Achilles tendinopathy, also it takes months to recover from the condition, hence, we had done an experimental study to lessen the recovery time by adding neural tissue mobilisation in this integrated neuromuscular exercise program.
This study is very important because along with the musculoskeletal issues women might experience neural issue thereafter due to underlying pathology of the Achilles tendon. Hence, neuromuscular exercise program can be considered as an essential part in the treatment of Achilles tendinopathy.
Conclusion
In this study we concluded that group A who followed an integrated neuromuscular exercise program has shown an improvement in the length of the calf muscle and intensity of pain as compared to group B. Neural tissue mobilization along with stretching and strengthening has proven to have a greater impact on the betterment of chronic mild Achilles tendinopathy. The distance of walking without pain was increased after the completion of treatment and the overall quality of life was improved because of an integrated neuromuscular exercise program. Thus, we can conclude that an integrated neuromuscular program is significantly effective in the treatment of Achilles tendinopathy.
Conflict of Interest
There were no conflicts of interest in this study.
Ethical Clearance
Ethical clearance was taken from an institutional committee of Krishna Institute of Medical Sciences Deemed to be University, Karad.
Source of Funding
Krishna Institute of Medical Sciences Deemed to be University, Karad.
Suggestions and Recommendations
Study can be done on a larger population.
Study can be made more precise with more details.
Study can be used to treat men with chronic Achilles tendinopathy.
Further research can be done using a longer interventional period.
Similar study can be done for other tendinopathies.
References
- Maffulli N. Overuse tendon conditions: time to change a confusing terminology. J Arthrosc Relat Surg. 1998;14(8):840-3.
- Doral MN, Alam M, Bozkurt M, et al. Functional anatomy of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2010;18(5):638-43.
- Louise Spilsbury; Richard Spilsbury. The Science of the Skeleton and Muscles. 2017.
- Chaurasia BD. Human anatomy. 2000.
- Stilwell Jr DL. The innervation of tendons and aponeuroses. Am J Anat. 1957;100(3):289-317.
- Kirkendall DT, Garrett WE. Function and biomechanics of tendons. Scand J Med Sci Sports. 1997;7(2):62-6.
- Khan KM, Maffulli N. Tendinopathy: an Achilles' heel for athletes and clinicians. Clin J Sport Med. 1998;8(3):151-4.
- Franceschi F, Papalia R, Paciotti M, et al. Obesity as a risk factor for tendinopathy: a systematic review. Int J Endocrinol. 2014.
- Rompe JD, Nafe B, Furia JP, et al. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a randomized controlled trial. Am J Sports Med. 2007;35(3):374-83.
- Petersen W, Welp R, Rosenbaum D. Chronic Achilles tendinopathy: a prospective randomized study comparing the therapeutic effect of eccentric training, the AirHeel brace, and a combination of both. Am J Sports Med. 2007;35(10):1659-67.
- Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med. 2009;19(1):54-64.
- Oliva F, Piccirilli E, Berardi AC, et al. Hormones and tendinopathies: the current evidence. Br Med Bull. 2016;117(1):39-58.
- Pravina P, Sayaji D, Avinash M. Calcium and its role in the human body. Int J res pharm biomed sci. 2013;4(2):659-68.
- Milanovic Z, Pantelic S, Trajkovic N, et al. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging. 2013;8:549.
- Basson A, Olivier B, Ellis R, et al. The effectiveness of neural mobilization for neuromusculoskeletal conditions: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2017;47(9):593-615.
- Coppieters MW, Butler DS. Do ‘sliders’ slide and ‘tensioners’ tension? An analysis of neurodynamic techniques and considerations regarding their application. Man Ther. 2008;13(3):213-21.
- Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7(1):36-49.
- Webborn N, Webborn NA. Neuropathic model to the etiology and management of Achilles tendinopathy. Tendinopathy in athletes. 2007:145-59.
- Ceravolo ML, Gaida JE, Keegan RJ. Quality-of-life in Achilles tendinopathy: an exploratory study. Clin J Sport Med. 2020;30(5):495-502.
- Fahlström M, Jonsson P, Lorentzon R, et al. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):327-33.
- Nakano J, Yamabayashi C, Scott A, et al. The effect of heat applied with stretch to increase range of motion: a systematic review. Phys Ther Sport. 2012;13(3):180-8.
- Beyer R, Kongsgaard M, Hougs Kjaer B, et al. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: a randomized controlled trial. Am J Sports Med. 2015;43(7):1704-11.
- Mayer F, Hirschmuller A, Muller S, et al. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Br J Sports Med. 2007;41(7).
- Yoshida H, Sato N, Maeda T, et al. Simultaneous execution of hot pack and muscle stretching enables stronger muscle stretching due to the reduction of stretch pain. Physiother. 2015;101:e1700.
- Mazzone MF, McCue T. Common conditions of the Achilles tendon. Am Fam Physician. 2002;65(9):1805.
- Grigg NL, Wearing SC, O’Toole JM, et al. The effect of exercise repetition on the frequency characteristics of motor output force: Implications for Achilles tendinopathy rehabilitation. J Sci Med Sport. 2014;17(1):13-7.
- Romero-Morales C, Calvo-Lobo C, Rodriguez-Sanz D, et al. Effectiveness of neural mobilization on pain and disability in individuals with musculoskeletal disorders. InTreatments, Mechanisms, and Adverse Reactions of Anesthetics and Analgesics. 2022; 555-64. Academic Press.
- Wyndow N, Cowan SM, Wrigley TV, et al. Neuromotor control of the lower limb in Achilles tendinopathy: implications for foot orthotic therapy. Sports Med. 2010;40:715-27.
- Matocha MA, Baker RT, Nasypany AM, et al. Effects of neuromobilization on tendinopathy: Part II. Int J Athl Ther Train. 2015;20(2):41-7.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref