Research Article - Current Pediatric Research (2022) Volume 26, Issue 9
Double aortic arch: A rare cause of wheezing and respiratory distress in infants: A case Report.
Abhishek Chakraborty*, Sanket R, Ebor Jacob
Department of Pediatric, Critical Care Medicine, Christian Medical College Vellore, Tamil Nadu, India
- *Corresponding Author:
- Abhishek Chakraborty
Department of Pediatric
Critical Care Medicine
Christian Medical College Vellore
Tamil Nadu
India
E-mail: abhismch12@gmail.com
Received: 02 September, 2022, Manuscript No. AAJCP-22-70972; Editor assigned: 05 September, 2022, PreQC No. AAJCP-22-70972(PQ); Reviewed: 12 September, 2022, QC No. AAJCP-22-70972; Revised: 19 September, 2022, Manuscript No. AAJCP-22-70972(R); Published: 27 September, 2022, DOI:10.35841/0971-9032.26.9.1640-1642.
Abstract
Double aortic arch is a rare congenital disorder. A symptom arises due to compression of treachea or esophagus. Its presentation varies from asymptomatic cases to life threatening respiratory distress. Clinical diagnosis is often difficult due to presence of wide verities of symptoms. We describe a three month old child presented with wheezing and severe respiratory distress and found to have double aortic arch.
Keywords
Double aortic arch, Wheeze, Stridor, Feed intolerance, Treacheal compression.
Introduction
Vascular ring reportedly represents less than 1% of all congenital cardiovascular anomalies, but this may be an underestimate because some conditions are asymptomatic [1]. Double aortic arch is the most common vascular ring (40%) [2]. Failure of regression of both the right and left fourth branchial arches resulting in right and left aortic arches, respectively. These two arches encircle and compress treachea and esophagus. Presentation may vary from life threating respiratory distress to aymptomatic condition.
Case Report
3 months old, male infant presented with h/o cough and coryza for 1 week and respiratory distress for one day. He was apparently well thrived infant was treated in local hospital as OPD basis with oral bronchodilator and later on with nebulization. However with worsening of symptoms, he was referred to our hospital. There was h/o intermittent noisy breathing since birth. There was no h/o fever, vomiting or regurgitation of feeds. Past history was uneventful. On examination had tachypnea (RR-65/MIN), sub costal retraction, SPo2 was 91%.
On examination of the respiratory system, he had bilateral wheeze .The cardiovascular findings were unremarkable. Baby was otherwise awake. The chest X-ray revealed hyper inflated lung fields bilaterally. He was started on high flow oxygen and inhalation and IV bronchodilator therapy. As his respiratory distress worsens, his respiratory support was upgraded to non-invasive ventilation in the form of nasopharyngeal CPAP. However despite of all these measures his condition was worsened and on day 3 of PICU admission he was intubated and started on mechanical ventilation. However after intubation, had rapid improvement in clinical status with minimal ventilator requirements and had no wheeze. So all bronchodilator was tapered and stopped. His treacheal aspirate was examined for respiratory viral PCR and corona virus (not covid 19) was positive. After 48 hours of invasive ventilation, he was extubated to high flow oxygen.
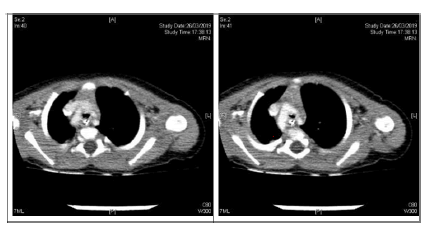
After 24 hours of extubation, his respiratory distress worsens. There was stridor and also worsening of wheeze, not responding to bronchodilator. Baby was again started on non-invasive ventilation (nasopharyngeal CPAP) and adrenaline nebulization was given. Baby gradually improved and after 48 hours he was weaned to high flow oxygen and gradually he was weaned from all types of respiratory support. In view of h/o intermittent noisy breathing and rapid improvement of wheeze post extubation, structural anomaly was suspected. Nasopharyngeal laryngoscopy was done and laryngomalacia was ruled out. We planned CT thorax with contrast was done and it revealed double aortic arch with atretic segment present posterolaterally on the left side causing treacheal stenosis. Patient was the referred to CTVS; surgery was planned on a later date.
Intraoperative findings were presence of double aortic arch, the posterior arch was continuing as left subclavian artery, beyond this it was a fibrous band joining the anterior arch which was continuing as descending aorta, thereby forming a sling compressing the distal treachea and left main bronchus. The compression was completely released by dividing the fibrous band and the ductal tissue. Post-operative patient was well, extubated on same day. Baby was discharged on 5th post-operative day on breast feeding (Figure 1).
Discussion
Aortic arch anomalies are rare congenital anomaly & have different types of clinical presentation. During embryonic life, dorsal and ventral aortas are connected by 6 aortic arch. Out of six arch, 1st, 2nd and 5th arch regressed eventually. The fourth aortic arch persists on both sides, but its ultimate fate is different on the right and left sides. On the left, it forms part of the arch of the aorta, between the left common carotid and the left subclavian arteries arteries. On the right, it forms the most proximal segment of the right subclavian artery [2]. In normal development, the right 4th arch is regressed. Failure of regression of right fourth arch forms double aortic arch.
If the double aortic arch remains at this stage, it may form a vascular ring surrounding trachea and esophagus and can compress them at different degrees. Double aortic arch is of three types, right arch is dominant in about 75% of cases, left dominant arch is around 20%, and in 5% cases both are of same size [3] (balanced arch). In our case, right arch dominant was detected. Double aortic arch is usually an isolated cardiac anomaly, but may rarely be associated with other cardiac anomaly like tetralogy of fallot, truncus arteriosus, TGA, VSD or coarctation of aorta, pulmonary artery stenosis [4-6].
The clinical diagnosis of vascular rings is often challenging for the pediatrician because the clinical manifestations are heterogeneous and nonspecific. Symptoms can vary from wheezing, stridor, dyspnea, and/or dysphagia to life-threatening conditions [5]. Many cases are asymptomatic. Most cases of vascular ring presents with inspiratory stridor and feeding problems. In double aortic arch, symptoms tend to appear before 3 months of age and they are more severe than those in right aortic arch with left ligamentum arteriosum. Symptoms often made worse by feeding [1]. Many cases present with recurrent wheezing mistreated as asthma. Many patients had recurrent upper respiratory tract infections, chronic cough, or both [3]. Sometimes diagnosis becomes difficult due to variation in clinical spectrum [4]. In our case, h/o intermittent mild noisy breathing was present since birth and at three months the child presented with wheezing and severe respiratory distress.
Vascular rings can be identified by several imaging studies and sometimes multiple imaging tests may be required to make a diagnosis [7,8]. Chest radiograph is often the initial imaging test and some abnormalities are found in almost all patients with vascular rings [9]. Arch laterality may be inferred from the Anteroposterior (AP) radiograph by the pattern of indentation of the tracheal air column, which is from the right in a right arch, left in a left arch and bilateral in a double arch. On the lateral view, tracheal narrowing may be apparent. Barium oesophagography is often performed in children with feeding difficulties. The specific type of vascular ring can often be diagnosed based on the pattern of oesophageal indentation on the oesophagram in combination with the pattern of tracheal indentation on the radiograph.
Bilateral indentation in the AP view is due to a double arch. Right indentation is caused by a right arch or a double arch with left atresia. Left indentation is caused by a double arch with a right arch atresia or circumflex aortic arch with right ductus. Echocardiography with colour-flow Doppler can sometimes detect vascular ring. It is also useful in the detection of associated congenital abnormalities. CT has emerged as the preferred imaging examination for the diagnosis and characterization of vascular rings. It is performed in symptomatic patients with a suspected vascular ring to delineate the anatomy and help surgical planning. Advantages of CT include the rapid acquisition time without the need for sedation or general anaesthesia; high spatial and temporal resolution; large field of view; isotropic voxels with multiplanar reconstruction capabilities; and simultaneous evaluation of the vasculature, airways and, to a lesser degree, the oesophagus.
The 3D volume-rendered and shaded surface display images can be helpful for surgical planning and depicting the anomalous anatomy [7], but has the disadvantage of radiation exposure and need for nephrotoxic IV contrast media. MRI is another imaging modality. Advantages of MRI include a wide field of view, multiplanar imaging capabilities and adequate spatial resolution to detect vascular ring and associated airway anomalies, without the use of ionising radiation or iodinated contrast material. The disadvantage is it needs good sedation sometimes general anaesthesia with intubation. Intubation also limits tracheal evaluation [10]. Bronchoscopy is rarely performed now days as this is an invasive procedure and adds little information to the diagnosis. However it is a useful tool in delineating tracheobronchial malacia associated with vascular ring in some patient.
Conclusion
Vascular ring is rare cause of respiratory distress in infancy. However in patients with stridor, feeding difficulties, recurrent wheezing or respiratory tract infection, proper investigation should be done to rule out vascular ring.
References
- Park Myung K. Park’s pediatric cardiology for practioners. (6th edn). Philadelphia: Elsevier 2014; pp: 307-313.
- Sadler TW. Langman’s medical embryology. (12th edn) Philadelphia: Wolters Kluwer 2012; pp: 185-191.
- Backer CL, Mavroudis C, Rigsby CK, et al. Trends in vascular ring surgery. J Thorac Cardiovasc Surg 2005; 129: 1339–47.
- https://www.hkjpaed.org/pdf/2003;8;126-129.pdf
- Licari A, Manca E, Rispoli GA, et al. Congenital vascular rings: A clinical challenge for the pediatrician. Pediatr Pulmonol 2015; 50: 511-524.
- McElhinney DB, Clark BJ, Weinberg PM, et al. Association of chromosome 22q11 deletion with isolated anomalies of aortic arch laterality and branching. J Am Coll Cardiol 2011; 37: 2114-2119.
- Etesami M, Ashwath R, Kane J, et al. Computed tomography in the evaluation of vascular rings and slings. Insights Imaging 2014; 5(4): 507–521.
- Browne LP. What is the optimal imaging for vascular rings and slings? Pediatr Radiol 2009; 39 (Supp 2): 191–195.
- Pickhardt P, Siegel M, Gutierrez F. Vascular rings in symptomatic children; frequency of chest radiographic findings. Radiology 1997; 203: 423–426.
- Kussman BD, Geva T, McGowan FX. Cardiovascular causes of airway compression. Paediatric Anaesth 2004; 14: 60–74.