Research Article - Biomedical Research (2017) Volume 28, Issue 14
Do economic conditions and in-kind benefits make needy patients bond together? Insights from cross-section data on clusters of co-located patients in Vietnam
Quan Hoang Vuong1,2* and Ha Nguyen2
1Department of Finance, Universite Libre de Bruxelles, Belgium
2FPT University School of Business, Vietnam
- *Corresponding Author:
- Quan Hoang Vuong
Department of Finance
Universite Libre de Bruxelles, Belgium
Accepted date: August 18, 2016
Abstract
Introduction: The phenomenon of desperate patients living together in voluntary co-location clusters has been emerging over the past decade in Vietnam. Patients seek to share facilities, reduce costs and rely on one another for support to make life safer and less miserable. There has not been much research on these clusters and patients' bonding to their community.
Methods: The study uses a cross-section data set containing 336 observations from four patients’ colocation clusters, collected from 2015 Q4 to 2016 Q1. The analysis employs the baseline category logits model for dichotomous variable, and reports logistic regression results. The main hypothesis is both economic conditions and in-kind benefits received from the community have influence on patients' bonding to their community.
Results: Both personal economic conditions and benefits are found statistically significant, but the inkind benefits decrease the bonding strength of the community, while the impact of economic instability is as expected. The strongest factor that serves to bond the patients together is the free will and predetermination of patients themselves to join the community.
Discussion: Patients in unstable conditions will more likely to stick to the co-location community. But those in better economic conditions show a more complex need and their perceptions change depending on the specific conditions. In-kind benefits are not what poorer patients expect and when they see these benefits from the community as “substitutes” for financial means, their expectation of sticking to the community declines.
Keywords
Patients’ quality of life, Medical expenses, Personal economic conditions, In-kind benefits, Bonding strength.
Introduction
Needy patients in Vietnam have been facing risks of destitution [1] and decreasing quality of life [2,3]. The problem appears to have been persistent due largely to undeveloped healthcare and health financing systems, especially for patients from rural areas or those suffering from chronic diseases [1,4]. To cope with harsh realities of life during their medical treatments, an increasing number of Vietnamese patients have chosen to live together in voluntary co-location clusters [5] where they seek to support one another in reducing burdens and sharing resources, apart from information needs [6]. By living together, patients in need hope for some improvement in quality of life [7], which is a crucial part constituting quality of healthcare during their long-term treatment [8].
Patients with lower socio-economic status face more hurdles during their treatments as costs emerge to be major barrier to basic treatment facilities, quality medicine and adequate care giving [4,9,10]. Therefore, co-location clusters that help share basic amenities and reduce costs of accommodation, for some, become the only choice [11-13]. An important part of patients' needs can be met with in-kind benefits [14] that those voluntary communities may be able to deliver [5].
Nonetheless, little research has been done with respect to the emerging phenomenon of patients' co-location clusters in urban areas in Vietnam. This short article communicate new insights acquired from our investigation into a set of cross-section data surveying co-located patients in such clusters in Hanoi, Vietnam.
The main hypothesis that is tested for acquiring the insights reported in this article follows.
Research hypothesis
Personal economic conditions and in-kind benefits provided by the community have impacts on the bonding of patients in a co-location cluster during their treatment period.
Materials and Methods
Data set
The data set employed in this research has been collected by the research team at Hanoi-based Vuong and associates from December 2015 through March 2016, containing 336 observations from four different clusters of co-located patients in Hanoi.
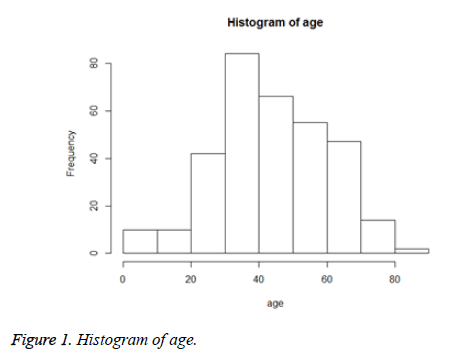
Among 336 patients observed, there were 169 females and 167 males, aged from under one year old to 84 years old. Patients in the 30-50 age brackets made up the largest portion of the sample, accounting for nearly 58% of the total number (Figure 1).
The 4 clusters of co-located patients in Hanoi include: Ngoc Hoi cluster (named after their location, south of Hanoi; many have a Chronic Kidney Disease (CKD)), out-patient residence cluster (patients with dangerous diseases requiring long-term treatment), kidney cluster (patients with a Chronic Kidney Disease (CKD)), and paediatrics cluster (young patients with various long-term diseases). Kidney cluster and out-patient residence cluster housed the most patients, with 139 and 128 individuals respectively. A majority of the above-mentioned patients have received their treatment at Bach Mai Hospital and Agriculture General Hospital, with the exception of paediatrics cluster patients who seek medical help at Vietnam National Hospital of Paediatrics.
The data are used to assess the degree of significance of patients’ economic conditions and in-kind benefits they receive and evaluate how these factors affect the bonding of patients.
In the structured data Table 1, these factors are coded as “PEC” (Personal Economic Conditions) and “Ben.ikd” (in-kind Benefits provided to a patient).
| “PEC” | “Ben.ikd” | “indisp.dur” | “disp.dur” |
|---|---|---|---|
| “stable” | “met.ikd” | 19 | 25 |
| “unmet.ikd” | 23 | 14 | |
| “unstable” | “met.ikd” | 27 | 27 |
| “unmet.ikd” | 165 | 36 |
Table 1. Distributions of “Bonding” responses against “Personal Economic Conditions (PEC)” and “Ben.ikd (in-kind Benefits provided to a patient)” values.
The variable Personal Economic Conditions (PEC) indicates the patient’s current economic conditions, which contributes to the process of assessing their life quality as well as financial abilities concerning treatment costs. Personal Economic Conditions (PEC) has two states (i.e., values): “stable” and “unstable”, noted per the patient’s self-assessment. A patient with a stable economic is defined as one who has a stable, above-average monthly income, able to overcome financial hardship and cover basic medical costs. Unstable Personal Economic Conditions (PEC) likewise refers to a patient's opposite state of economic security.
Likewise, “Ben.ikd” (in-kind Benefits provided to a patient) has two states (values): “met.ikd” (in-kind benefits that meet a patient's needs) and “unmet.ikd” (in-kind benefits that unmet a patient's needs). A patient who reports the state “met.ikd” (inkind benefits that meet a patient's needs) is basically satisfied with in-kind benefits that his/her community has provided during the treatment period. The opposite state “unmet.ikd” (in-kind benefits that unmet a patient's needs) reports unsatisfactory in-kind benefits from the community. In-kind benefits provided to patients by charitable organizations and individuals usually include food such as rice, noodle, cooking oil, etc. and other basic consumer goods.
These two factors “Personal Economic Conditions (PEC)” and “Ben.ikd (in-kind Benefits provided to a patient)” serve to be predictor variables in our analytical model-which is presented in the statistical analysis subsection-whose numerical values enable us to compute useful empirical probabilities.
Following our hypothesis, these predictors are expected to influence the response variable “Bonding”, which reports whether a patient sees his/her bonding to the co-location cluster as indispensable (value/state: “indisp.dur”) or not (“disp.dur”).
From Table 1 we learn that the majority of surveyed co-located patients are in “unstable” state of PEC: 255 (out of 336). A large portion of patients, nearly 70%, considers living in the community “indispensable” during their medical treatment times, although most of them do not report satisfactory in-kind benefits from the community.
Statistical analysis
This study employs the Baseline Category Logits (BCL) framework for analysis of categorical data. The Baseline Category Logits (BCL) framework that is used to examine the empirical data sets estimates a multivariate Generalized Linear Model (GLM) in the following form:
g(μi)=Xi β,
Where, μi=E (Yi), corresponding to yi=(yi1,yi2,…); row h of the model matrix Xi for observation i contains values of independent (also, predictor) variables for yih.
Due to this set-up of the problem, and as πj (x) =P(Y=j | x) represent a fixed setting for independent variables, with Σjπj (x) =1, categorical data are distributed over J categories of Y as either binomial or multinomial with corresponding probabilities {π_1 (x), …, πj (x)}. Thus, the Baseline Category Logits (BCL) model aligns each dependent (response) variable with a baseline category: ln (πj (x)/πJ (x)), with j=1, …, J-1.
As ln (πa (x)/πb (x)) =ln (πa (x)/πJ (x))-ln (πb (x)/πJ (x)), the set of empirical probabilities from binomial and/or multinomial logits {πj (x)} can be computed using the formula:
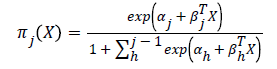
The categorical variables used in our models are dichotomous (e.g., the variate “Ben.ikd” has value of “met.ikd” or “unmet.ikd”), thus practically making the analysis logistic regressions. The coded names and values for those dichotomous variables are described in the corresponding data set in the data section. Practical estimations and technical details are given in [1,15], respectively. A possible alternative for modelling the data is log-linear analysis, with example is provided [16].
Results
The results reported in Table 2 below are estimated using the statistical package R 3.2.3. (See Appendix for the actual estimation that leads to subsequent analysis and computing of numerical values.)
| Intercept | “PEC” | “Ben.ikd” | |
|---|---|---|---|
| “stable” | “met.ikd” | ||
| β0 | β1 | β2 | |
| Logit ( indisp.dur | disp.dur) | 1.445*** (8.476) | -0.669* (-2.336) | -1.272*** (-4.734) |
Table 2. Estimation results on influence of predictor variables Personal Economic Conditions (PEC) and Ben.ikd (in-kind Benefits provided to a patient) on response variable “Bonding” during patients’ medical treatment period.
All estimated coefficients are statistically significant at any conventional levels (p<0.01). And both β1, β2<0. Generally speaking, such factors as Personal Economic Conditions (PEC) and Ben.ikd (in-kind Benefits provided to a patient) are all influential to patient’s bonding strength.
With, β1=-0.669 (p<0.01) corresponding to Personal Economic Conditions (PEC) =stable, and β2=-1.272 (p<0.0001) for Ben.ikd (in-kind Benefits provided to a patient) =met.ikd (inkind benefits that meet a patient's needs), the empirical data show that stable economic conditions and satisfactory in-kind benefits from the community both reduce the bonding strength of patients in the community. However the larger absolute numerical value with positive sign of the intercept β0=+1.445 (p<0.0001) tells us that the propensity of staying with the community is somewhat natural and less dependent on economic conditions and/or benefits received from the community.
From Table 2, we arrive at the empirical relationship given in Equation RQ1:
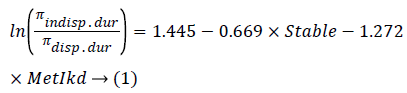
An example of the computation of an empirical probability from Equation RQ1 for a patient in unstable economic condition and in receipt of in-kind benefits provided by the community is as follows:
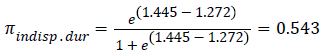
Thus, there is a probability of 54.3% that such a patient will be likely to be loyal and stick to the community. Distributions of probabilities conditional on different states for “PEC” and “Ben.ikd” are provided in Appendix B.
Appendixes
A. Estimating the relationship in R (3.2.3) using the data set:
>RQ1=read.csv ("D: /.../Data/Data336/tab 12.34.41.csv", header=T)
>attach (RQ1)
>contrasts (RQ1$Ben.ikd) =contr.treatment (levels (RQ1$Ben.ikd), base=2)
>contrasts (RQ1$PEC) =contr.treatment (levels (RQ1$PEC), base=2)
>fit.RQ1=glm (cbind (indisp, disp) ~ PEC+Ben.ikd, data=RQ1, family=binomial)
>summary (fit.RQ1)
B. Computed probabilities for a patient to stick to the community against different Patient Economic Conditions (PEC) and in-kind benefits conditions
| “Bonding” | “indisp.dur” (a) | “dis.dur” (b) | ||
|---|---|---|---|---|
| “PEC” | “Ben.ikd” | “met.ikd” | “unmet.ikd” | “met.ikd” | “unmet.ikd” |
| “stable” | 0.378 | 0.685 | 0.622 | 0.315 |
| “unstable” | 0.543 | 0.809 | 0.457 | 0.191 |
Discussion
From the above results, we arrive at some insights and potential ideas for future examination, as discussed in what follows.
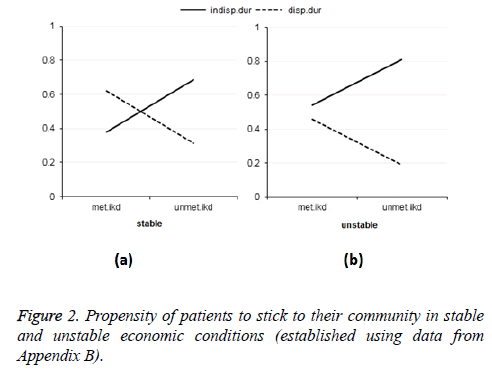
First, patients who face less stable economic conditions tend to be sticking to the community regardless of the level of in-kind benefits they receive from the community. The trend can be observed in Figure 2.
Figure 2a, unstable (right-hand-side) graph shows a clear difference with a much stronger propensity of patients to stick to the community compared to the other graph. This effect of economic conditions agrees with the basis on which co-located patient clusters were formed: poor patients in expensive longterm treatment banding together in attempt to lower costs [6]. Patients with unstable income are in a greater need of support, therefore finding the community to be more important than those in better economic conditions. In other words, the poorer patients are, the more they need the community and the more closely they bond. Even so, it seems more likely that the patient’s predetermination plays a greater role in knitting them closer within the cluster. Perhaps it is not only financial concerns, but also the very human need to feel the neither financial nor in-kind support, that comes into play.
On the other hand, for the Figure 2b, stable (left-hand-side), the trends for patients in stable conditions change when switching from significant to insignificant in-kind benefits. The situation is a little more complicated than for those in unstable economic conditions: while financially unstable patients always show inclination to bond with the cluster despite their satisfaction with in-kind benefits, patients with stable Patient Economic Conditions (PEC) are more likely to find the community inessential when, oddly enough, in-kind benefits match their needs. The observation raises questions: could it be that patients don’t truly appreciate benefits when given in kind, or that they see in-kind needs as less urgent than financial ones? Given that in-kind donations constitute a large part of charity in general, does this mean co-located clusters receive less efficient social support compared to other people in need?
In the same vein, it is noteworthy that in-kind benefits do not appear to be a driver for patients to bond together, rather the opposite. While patients with unstable Patient Economic Conditions (PEC) are always more attached to the community than their more stable counterparts, the gap in fact widens slightly when patients think the received in-kind benefits are adequate to their needs. Perhaps a proper explanation for this phenomenon is that most patients who decide to co-live in these clusters have a primary concern of seeking financial means. In-kind benefits are not what they expect, and thus, when they see these benefits as a “substitute” for financial means (such as low-cost borrowings, income-generating supports or giving in cash.) the benefits end up decreasing the perceived bonding strength (as opposed to how appreciative they are of financial benefits) [6]. It’s interesting to remark that even though the patients are in dire need, they still show clear preferences when it comes to benefits-or lack thereof, in the case of in-kind benefits. The question is: do co-located patients hold the same preferences when given help from the society? Seeing as the type of benefits they receive greatly affects how they bond within the cluster, would getting the “wrong” kind of benefits from the society impact their state of mind and decreases their quality of life even further during treatment?
The subject of co-located patient clusters, though highly specific, leaves many curious questions worth investigating.
References
- Vuong QH. Be rich or dont be sick: estimating Vietnamese patients’ risk of falling into destitution. Springer plus 2015; 4: 529.
- Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Soc Sci Med 2001; 52: 1501-1516.
- Long Q, Smith H, Zhang T, Tang S, Garner P. Patient medical costs for tuberculosis treatment and impact on adherence in China: a systematic review. BMC Public Health 2011; 11: 393.
- Bach TX, Long NH, Vuong NM, Cuong NT. Health status and health service utilization in remote and mountainous areas in Vietnam. Health Qual Life Outcomes 2016; 14: 85.
- Vuong QH, Nguyen TK, Do TD, Vuong TT. Whither voluntary communities? A study of co-located patients in Vietnam. Working Papers CEB 2016; 16-24.
- Vuong QH, Nguyen, TK. Vietnamese patients’ choice of healthcare provider: in search of quality information. Int J Behav Healthc Res 2015; 5: 184-212.
- Lehman AF, Possidente S, Hawker F. The quality of life of chronic patients in a state hospital and in community residences. Hosp Commun Psych 1986; 37: 901-907.
- Li MY, Yang YL, Liu L, Wang L. Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: a cross-sectional study. Health Qual Life Outcomes 2016; 14: 73.
- Clavarino AM, Lowe JB, Carmont SA, Balanda K. The needs of cancer patients and their families from rural and remote areas of Queensland. Aus J Rural Health 2002; 10: 188-195.
- Hardeman W, Van Damme W, Van Pelt M, Por I, Kimvan H. Access to health care for all? User fees plus a Health Equity Fund in Sotnikum, Cambodia. Health Policy Plan 2004; 19: 22-32.
- Delva D, Vanoost S, Bijttebier P, Lauwers P, Wilmer A. Needs and feelings of anxiety of relatives of patients hospitalized in intensive care units: implications for social work. Soc Work Healthc 2002; 35: 21-40.
- Duggleby W, Williams A, Ghosh S, Moquin H, Ploeg J, Markle-Reid M, Peacock S. Factors influencing changes in health related quality of life of caregivers of persons with multiple chronic conditions. Health Qual Life Outcomes 2016; 14: 81.
- Ekback MP, Lindberg M. Social support: an important factor for quality of life in women with hirsutism. Health Qual Life Outcomes 2014; 12: 183.
- Wen KY, Gustafson DH. Needs assessment for cancer patients and their families. Health Qual Life Outcomes 2004; 2: 11.
- Agresti A. Category data anal John Wiley NY (3rd edn.) 2013.
- Vuong QH, Napier NK, Tran TD. A categorical data analysis on relationships between culture, creativity and business stage: the case of Vietnam. Int J Trans Innov Sys 2013; 3: 4-24.